Last Updated on November 27, 2025 by Bilal Hasdemir

Thoracic surgery is a complex procedure that can save lives. Many patients, however, worry about ICU after thoracic surgery. Research shows that intensive monitoring is needed depending on the surgery’s complexity and the patient’s overall health.
Knowing about the recovery process helps ease patient worries. We’ll look into what affects the need for post-surgical monitoring and what it means.
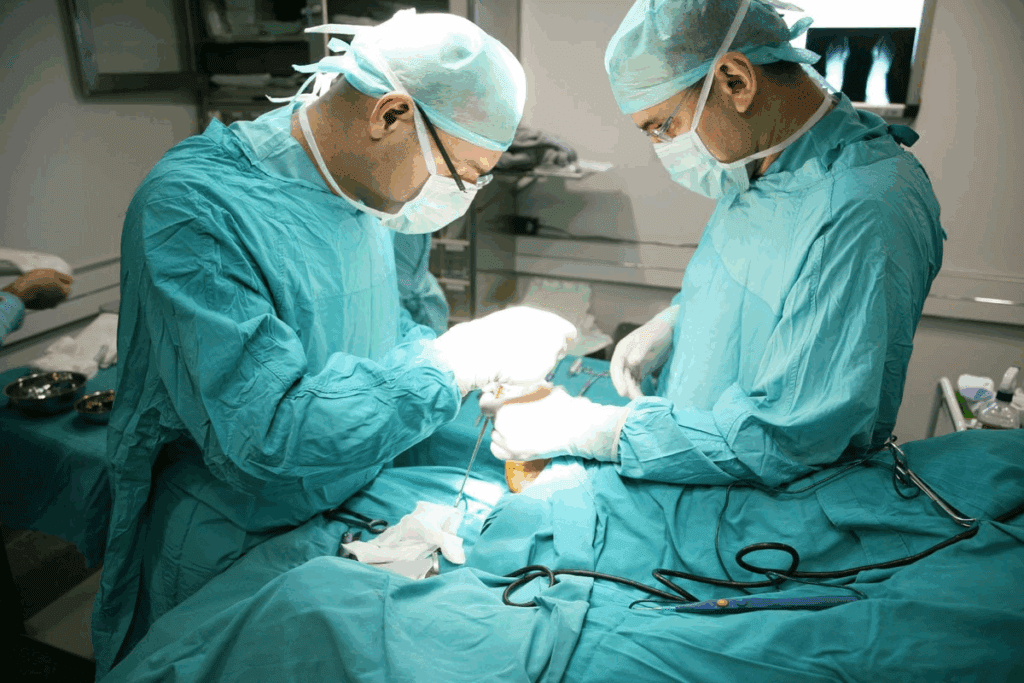
Thoracic surgery covers a wide range of operations in the chest area. These surgeries are complex and need great precision and care.
They involve the lungs, heart, esophagus, and other chest structures. The complexity depends on the condition and the patient’s health.
Lung surgeries like lobectomy and pneumonectomy remove diseased lung parts. This is often for cancer or other issues. Other common surgeries include:
Cardiac surgeries, like coronary artery bypass grafting (CABG) and heart transplant, treat heart disease. Esophageal surgeries, including esophagectomy, remove esophageal cancer or repair damage.
These surgeries show the complexity and variety of thoracic surgery. They highlight the need for specialized care and sometimes ICU monitoring after surgery.

Whether a patient needs ICU care after thoracic surgery depends on many things. We look at each case closely to decide the right care level.
Today’s post-surgery care is more advanced. It uses better monitoring and treatments. Enhanced Recovery After Surgery (ERAS) is becoming more popular. It focuses on preoperative optimization, minimally invasive techniques, and effective pain management.
But, deciding if a patient needs ICU care is not simple. We consider the patient’s health, the surgery’s complexity, and any health issues they have.
Several important factors help decide if a patient needs ICU care after thoracic surgery:
By carefully looking at these factors, we make sure patients get the right care after thoracic surgery.
It’s key to spot who might face big risks after chest surgery. We look at many factors to see if someone should go to the ICU after thoracic surgery.
Some patients are at higher risk for problems after chest surgery. This includes those with heart disease, COPD, or diabetes. Being older or not being very active before surgery also raises the risk.
Here are some key traits of high-risk patients:
We use systems to guess the chance of problems after surgery. These tools help us find who needs the ICU’s watchful eye.
The Thoracoscore is one tool that guesses how likely a patient is to die in the hospital after thoracic surgery. The American Society of Anesthesiologists (ASA) Physical Status system also rates a patient’s health before surgery.
| Risk Stratification System | Description | Key Factors Considered |
| Thoracoscore | Predicts in-hospital mortality after thoracic surgery | Age, performance status, dyspnea score, priority of surgery, procedure class, diagnosis group |
| ASA Physical Status | Assesses the physical status of a patient before surgery | Overall health, presence of systemic disease, functional limitation |
These systems help us pinpoint who’s at high risk for complications. They guide us to decide if someone needs ICU care after chest surgery.
The first 24 hours after thoracic surgery are very important. Patients are watched closely for any problems. They also get help to manage pain and aid in their recovery.
Patients go to the recovery room after surgery. Here, they are watched as they wake up from anesthesia. The staff makes sure they are comfortable and their vital signs are okay.
Key aspects of post-anesthesia care include:
Watching vital signs is key in post-operative care. We keep a close eye on our patients’ signs to spot any problems early. This helps us act fast to avoid complications.
The table below outlines the key vital signs monitored and the interventions that may be implemented:
| Vital Sign | Normal Range | Intervention if Abnormal |
| Heart Rate | 60-100 bpm | Administer medication to control heart rate if necessary |
| Blood Pressure | 90/60 – 120/80 mmHg | Adjust medication or administer fluids as needed |
| Oxygen Saturation | 95-100% | Provide supplemental oxygen if saturation falls below 95% |
Good monitoring and care in the first 24 hours after thoracic surgery are vital. Our team works hard to give the best care. This ensures our patients have the best chance of a good recovery.
Respiratory care is key for thoracic surgery patients in the ICU. It helps avoid complications and aids in a smooth recovery.
Patients after thoracic surgery might need ventilation support. The type and how long they need it depends on their health and the surgery’s complexity.
There are different ventilation support options. These include invasive mechanical ventilation and non-invasive methods like CPAP and BiPAP.
The weaning process is about slowly taking the patient off the ventilator. It’s a critical step that must be done carefully to prevent breathing problems.
Respiratory therapy is essential in the weaning process. It includes chest physiotherapy, breathing exercises, and aerosol therapy. These help clear mucus and improve lung function.
| Ventilation Support Type | Typical Duration | Patient Profile |
| Invasive Mechanical Ventilation | Several hours to days | Critically ill patients or those undergoing complex surgeries |
| Non-Invasive Ventilation (CPAP/BiPAP) | Variable, often shorter than invasive ventilation | Patients with less severe respiratory compromise |
Monitoring the heart after chest surgery is key to spotting and fixing problems early. We keep a close eye on our patients’ heart health to help them recover safely and smoothly.
Keeping an eye on the heart’s function is very important, more so for those who have had heart surgery. We use ECG to watch for heart rhythm problems and check the heart’s output continuously.
Our methods include:
It’s vital to manage heart rhythm issues and blood pressure changes after surgery. We employ medicines and lifestyle changes to keep the heart stable.
| Monitoring Type | Purpose | Method |
| ECG Monitoring | Detect arrhythmias and cardiac issues | Continuous electrocardiogram |
| Cardiac Output Monitoring | Assess heart function | Various techniques including invasive and non-invasive methods |
| Blood Pressure Monitoring | Manage hypertension or hypotension | Continuous or intermittent monitoring |
“The key to successful post-operative care is meticulous monitoring and timely intervention. Cardiovascular monitoring plays a vital role in this process.”
Dr. John Smith, Cardiothoracic Surgeon
By watching our patients’ heart health closely, we can spot and fix problems fast. This ensures the best results for them.
Advanced pain control is key in the thoracic ICU. It’s vital for patient comfort and to avoid complications from poor pain relief.
We use multimodal analgesia to manage pain well. This method combines different pain relief medicines and techniques. Multimodal analgesia often includes opioids, non-opioid analgesics, and other medications.
This approach cuts down on opioid use, lowers opioid side effects, and improves pain control. By targeting different pain pathways, we make pain management more effective.
Regional techniques like epidural analgesia and nerve blocks are important for pain management. Epidural analgesia sends pain relief medication to the epidural space around the spinal cord. It helps thoracic surgery patients a lot.
Nerve blocks inject local anesthetics around specific nerves to block pain signals. These methods offer great pain relief with fewer side effects than opioids.
Both epidural analgesia and nerve blocks need careful patient selection and precise technique. We also monitor them closely to avoid complications and ensure the best pain control.
Managing chest tubes and drainage systems is key in post-operative care for thoracic surgery patients. It’s vital for preventing complications and ensuring a smooth recovery.
There are mainly two types of drainage systems: traditional and digital. Traditional drainage systems use a water seal to control airflow and fluid out of the chest. They’ve been the standard for many years.
Digital drainage systems offer a newer approach. They use electronic sensors to monitor airflow and pressure, giving real-time data. This makes them popular for their accuracy and detailed information.
It’s important to monitor chest tube output to spot complications early. This includes checking the amount, color, and consistency of the fluid drained. Air leaks can also be detected through monitoring.
When troubleshooting chest tube issues, check for kinks or blockages. Make sure the system is working right and the patient isn’t in pain or having breathing problems. Regular checks and adjustments are key for the best patient care.
In summary, managing chest tubes well means more than just placing them. It involves ongoing monitoring and adjusting the system. Knowing about different systems and how to fix common problems helps healthcare providers improve patient outcomes after thoracic surgery.
Keeping fluid balance right and giving enough nutrients are key after surgery. After thoracic surgery, patients need careful fluid and nutrition management. This helps them recover well.
Managing IV fluids well is very important after surgery. We use a special method to adjust IV fluids for each patient. This method helps keep the heart working right and blood flowing well, lowering the chance of problems.
Key components of IV fluid management include:
A leading anesthesiology journal says, “Goal-directed fluid therapy has been shown to reduce postoperative complications and shorten hospital stay.” We follow this advice for our patients after thoracic surgery.
Starting enteral nutrition early is also very important. We start it within 24-48 hours after surgery if we can. This helps with healing, keeps the gut working, and lowers infection risk.
Benefits of early enteral nutrition include:
Our nutrition team works with the surgical team to make nutrition plans for each patient. This ensures they get the right nutrients for a good recovery.
“Nutritional support is not just about providing calories; it’s about supporting the body’s complex physiological processes during recovery.”
— Expert in Surgical Nutrition
Complications after thoracic surgery often mean a longer stay in the ICU. These issues can come from the patient’s health before surgery, how complex the surgery is, and the care after. Knowing about these complications helps us take better care of our patients.
Respiratory problems are common after thoracic surgery. These can include:
We treat these issues with respiratory therapy, careful watching, and sometimes bronchoscopy to clear airways.
Other complications can also affect ICU stay. These include:
Managing these issues means watching the heart closely, keeping blood pressure right, and catching infections or bleeding early.
| Complication Type | Common Issues | Management Strategies |
| Respiratory | Respiratory failure, pneumonia, atelectasis | Respiratory therapy, mechanical ventilation, bronchoscopy |
| Non-Respiratory | Cardiac issues, bleeding, infection/sepsis | Cardiac monitoring, blood pressure management, infection control measures |
By tackling these complications, we can help patients recover better and spend less time in the ICU.
The time a patient spends in the ICU after thoracic surgery varies a lot. This depends on the surgery type. Knowing this helps both patients and doctors plan better for recovery.
Lung resection or pneumonectomy surgeries often mean a longer ICU stay. This is because these surgeries are complex. Patients usually stay in the ICU for 2 to 5 days.
A study showed that lung resection patients stay in the ICU for about 3 days on average. The time can vary based on the patient’s health before surgery and any complications after.
Cardiac surgery, like CABG or heart transplant, needs a longer ICU stay. Patients typically stay for 3 to 7 days. Some may need to stay longer due to complications or extra treatments.
Even with better surgery techniques and care, cardiac surgery is complex. This means patients often need more time in the ICU.
The type of surgery affects how long a patient stays in the ICU. Minimally invasive surgeries, like VATS, usually mean shorter stays. This is because they cause less damage and pain.
| Surgical Approach | Average ICU Stay | Typical Complications |
| Minimally Invasive (VATS) | 1-3 days | Less frequent respiratory complications |
| Open Thoracic Surgery | 3-7 days | Higher risk of respiratory and cardiac complications |
The table shows that choosing minimally invasive surgery can make a big difference. It can shorten ICU stays and lower complication risks. Surgeons often choose these techniques to help patients recover faster.
In summary, ICU stay times after thoracic surgery vary a lot. They depend on the surgery, the patient’s health, and any complications. Knowing this helps in planning the best care after surgery.
When patients get better after thoracic surgery, moving from the ICU to a less intense care area is key. This move is more than just changing rooms. It shows the patient is stable and doesn’t need the ICU’s intense care anymore.
Deciding when to move a patient from the ICU is based on clear criteria. These include stable vital signs and better health. The patient should also be able to breathe on their own and manage pain without needing a ventilator or strong drugs.
We check these criteria closely to make sure patients are moved at the right time. Moving too soon can cause problems. Waiting too long can use up ICU space and slow recovery.
After moving to a step-down unit or ward, patients keep getting careful care. Their vital signs are watched closely, and pain and other symptoms are managed. They also get help with eating and learn about post-surgery care.
Here’s a table showing what care looks like in a step-down unit or ward:
| Care Aspect | Monitoring/Intervention | Frequency |
| Vital Signs | Temperature, Blood Pressure, Heart Rate, Oxygen Saturation | Every 4-6 hours |
| Pain Management | Assessment of pain levels and adjustment of analgesia | Every 4-6 hours or as needed |
| Nutritional Support | Assessment of nutritional status and dietary advice | Daily or as needed |
By managing the move from ICU to a less intense setting, we make sure patients get the right care. This helps them on their path to full recovery.
When you’re getting ready for thoracic surgery, think about the chance of needing ICU care. Knowing what to expect and how to get ready can really help your recovery. We suggest that patients take steps to get ready for ICU care.
Talking openly with your surgical team is key to getting ready for ICU. We tell patients to ask about the surgery, the chance of ICU, and what care they’ll get. This helps them mentally and emotionally prepare.
Ask about the monitoring and treatments in the ICU. Learn about life-supporting therapies like mechanical ventilation. Knowing this can make you feel less anxious and more in control.
Getting mentally and emotionally ready is just as important as the medical side. We recommend stress-reducing activities and support from loved ones or mental health experts. Meditation, deep breathing, or guided imagery can help with anxiety.
Remember, an ICU stay is common for many thoracic surgeries. Knowing ICU staff are skilled can give you peace of mind. Focus on your health before surgery, eat well, stay hydrated, and follow your team’s instructions.
By preparing in these ways, patients can face ICU with less fear. Our team is here to support you every step of the way, aiming for the best results for you.
Leaving the ICU is a big step, but the real recovery journey starts then. The path to full recovery involves getting better physically and mentally.
Physical therapy is key for patients after thoracic surgery and ICU stays. Tailored rehabilitation programs help patients regain strength and function. They also lower the chance of future health problems.
These programs mix physical therapy, occupational therapy, and respiratory therapy. The aim is to help patients live better lives.
Recovering mentally is just as important as recovering physically. Many face post-ICU syndrome, leading to anxiety, depression, or brain fog.
We tackle these mental health issues with multidisciplinary care. This includes psychological support and counseling. It helps patients deal with their emotional and mental recovery.
It’s vital to understand the full recovery journey after ICU. By focusing on both physical and mental health, we support a better recovery for all.
Thoracic surgery is a complex and delicate procedure. It needs thorough care for the best recovery. We’ve looked at the different parts of post-surgical care, from the ICU to long-term recovery.
Specialized care after thoracic surgery is key. It helps manage complications, ensures wound healing, and supports physical and emotional recovery. Critical care teams watch over patients, manage pain, and provide nutrition.
Recovering well after surgery is a detailed process. It needs a focus on the patient and their needs. By understanding the importance of specialized care, patients and families can better handle the recovery process.
We stress the need for a detailed care plan for each patient. This ensures they get the best support during their recovery.
Thoracic surgery deals with operations in the chest area, like lung and heart surgeries. ICU care is needed because these surgeries are complex. They can lead to serious complications like breathing or heart problems.
Thoracic surgery includes removing parts of the lung, heart surgeries, and operations on the esophagus. These surgeries are complex and carry risks.
Deciding if a patient needs ICU care depends on their health, the surgery’s complexity, and any health issues they have. The surgical team makes this decision based on each patient’s situation.
High-risk patients often have serious health conditions like heart disease or lung problems. Doctors use special systems to figure out who needs ICU care.
In the first 24 hours, patients are closely watched. They recover from anesthesia and get help with pain and any complications. This time is key for their recovery.
Patients might need help breathing, from using machines to special masks. The choice depends on how well they can breathe and the surgery they had.
Doctors use different pain medicines and special techniques like epidural blocks. These methods help control pain and reduce the need for strong pain drugs.
How long a patient stays in the ICU varies with the surgery. For example, lung surgery might be shorter than heart surgery.
Doctors handle complications with various treatments, like breathing therapy and heart support. They also address specific problems as they happen.
Doctors check if a patient’s vital signs are stable, if they’re in control of their pain, and if they can breathe well. If they pass these checks, they can move to a less intensive unit.
Patients can talk to their doctors before surgery to understand the risks and ICU needs. They can also prepare mentally to reduce stress.
Recovery after leaving the ICU includes physical therapy to regain strength. Patients may also face mental challenges, like post-ICU syndrome, which need support.
Specialized care in the ICU and other units is vital for patients after thoracic surgery. It helps manage their complex needs for the best recovery.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!