Last Updated on December 1, 2025 by Bilal Hasdemir
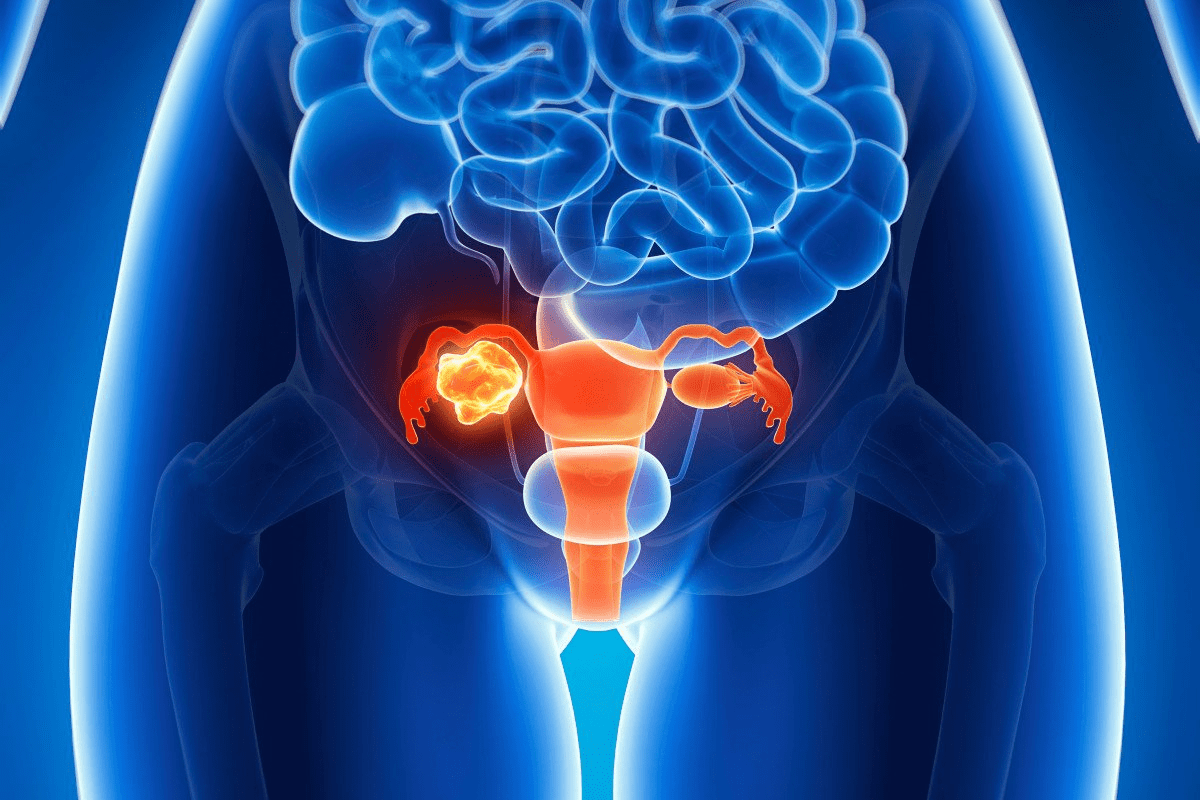
icu neuro difference
When a loved one is critically ill, it can be hard to understand the differences in care. Life-threatening neurological conditions need special care, which is what a neuro ICU provides.
A general ICU handles a wide range of severe illnesses or injuries. On the other hand, a neuro ICU focuses on patients with serious brain or spinal cord problems. This includes stroke, traumatic brain injury, or spinal cord injury.
Finding your way through these options can be tough. We aim to clear up the unique care neuro ICUs offer. This way, you can make better choices about your medical care.
Key Takeaways
- Neuro ICUs specialize in caring for patients with life-threatening neurological conditions.
- General ICUs provide critical care for a broad range of severe illnesses or injuries.
- The level of specialized care differs significantly between general ICUs and neuro ICUs.
- Understanding these differences is crucial for patients and families seeking medical care.
- Neuro ICUs offer targeted treatment for complex neurological conditions.
Understanding Intensive Care Units (ICUs)

A sprawling intensive care unit, illuminated by crisp, natural lighting filtered through large windows. The foreground features various medical equipment and monitoring devices, their sleek, modern designs complementing the sterile, yet calming atmosphere. In the middle ground, medical professionals in pristine white coats and scrubs move with purposeful efficiency, tending to the needs of their critically ill patients. The background showcases the expansive layout of the ICU, with separate sections for different levels of care, each area distinguished by subtle variations in color and equipment. The overall scene conveys a sense of focused, professional care within a state-of-the-art healthcare facility.
ICUs started in the 1950s as a response to the polio epidemic. They have since become a key part of healthcare. The polio virus made it necessary to ventilate and closely watch patients.
Intensive Care Units (ICUs) are special parts of hospitals. They offer intensive care medicine. This means watching over patients who are very sick. Critical illness includes many conditions, like severe infections and organ failure.
Definition and Purpose of ICUs
ICUs are for the sickest patients. They offer a multi-system approach to care. This is not found in regular hospital wards.
The main goal of ICUs is to give a safe and therapeutic place. Here, patients get life-saving treatments and are closely watched.
Teams of experts lead the care in ICUs. These teams include intensivists, critical care nurses, and others. They work together to meet the complex needs of very sick patients. They use advanced technologies to help.
Types of ICUs in Modern Hospitals
Today’s hospitals have different ICUs for various patients. Some common ones are:
- General ICUs, for many critical illnesses.
- Surgical ICUs, for patients after major surgery.
- Cardiac ICUs, for severe heart conditions.
- Neuro ICUs or Neurocritical care units, for life-threatening brain illnesses or injuries.
Having different ICUs lets hospitals give specialized care. This improves patient outcomes and care quality.
General ICU: Structure and Function
A sterile, clinical ICU ward with state-of-the-art medical equipment. In the foreground, a ventilator machine with a clear display panel and various knobs and settings. Beside it, a heart rate monitor with a steady pulsing waveform. In the middle ground, an IV stand with multiple hanging bags, and a mobile ultrasound machine with a sleek, angular design. In the background, a wall-mounted oxygen tank and a tall, metal medical cart stocked with supplies. Soft, even lighting illuminates the scene, creating a sense of order and professionalism. The overall atmosphere is one of advanced medical technology dedicated to patient care and recovery.
General ICUs are the heart of hospital critical care. They support a wide range of life-threatening conditions. These units handle many medical emergencies, making them key in healthcare.
Patient Population in General ICUs
The patients in general ICUs face many critical conditions. They need immediate and intensive care. This includes post-operative patients, those with severe infections, or trauma victims.
- Critically ill patients requiring close monitoring
- Post-operative patients needing intensive care
- Patients with severe medical conditions such as sepsis or acute respiratory distress syndrome (ARDS)
Common Conditions Treated
General ICUs manage a wide range of critical conditions. They handle respiratory failure, cardiac issues, and severe infections.
Common conditions treated in general ICUs include:
- Respiratory failure requiring mechanical ventilation
- Cardiac arrest and other cardiovascular emergencies
- Severe sepsis and septic shock
- Trauma and post-traumatic complications
Equipment and Resources
General ICUs have advanced equipment for high-quality critical care. They have ventilators, cardiac monitors, and dialysis machines.
This equipment helps healthcare professionals give the right care to critically ill patients. It improves outcomes and lowers mortality rates.
Neuro ICU: Specialized Neurological Care
A well-equipped neuro ICU ward with advanced medical equipment and highly trained staff. The room is brightly lit with a combination of warm overhead lighting and natural light streaming in through large windows. The foreground features various monitoring devices, IV stands, and a hospital bed with a patient undergoing specialized neurological care. The middle ground showcases a team of medical professionals, including nurses and neurologists, closely observing the patient and coordinating their treatment. The background depicts a clean, organized, and technologically advanced environment, with additional beds and monitoring stations, creating an atmosphere of focused, high-quality neurological care.
Neuro ICUs are a big step forward in treating severe brain conditions. They offer intensive care for patients with life-threatening brain illnesses or injuries. This level of care is not found in regular ICUs.
Definition and Purpose of Neurocritical Care Units
Neurocritical care units, or Neuro ICUs, focus on patients with critical brain disorders. Their main goal is to closely monitor and treat severe brain conditions. This includes stroke, traumatic brain injury, or seizures.
Neurological injuries and illnesses are complex. They need a team effort to manage. So, Neuro ICUs have a team of experts. This team includes neurologists, neurosurgeons, nurses, and more.
History and Development of Neuro ICUs
The idea of Neuro ICUs has grown over time. This growth came from new medical technology and better understanding of brain conditions. At first, ICUs treated many critical illnesses. But, as brain care got more complex, specialized units were needed.
Now, Neuro ICUs have the latest technology. This includes advanced brain monitoring and neuroimaging. These tools help doctors quickly spot and act on changes in a patient’s condition.
When Patients Need Neuro ICU Care
Patients go to Neuro ICUs for severe brain conditions. They need close monitoring and treatment. Some reasons for admission include:
- Stroke or cerebral vasculitis
- Traumatic brain injury
- Seizures or status epilepticus
- Neurosurgical complications
- Critical neuromuscular disorders
These patients need a lot of care. This includes watching their brain closely, managing pressure inside the skull, and other special treatments.
“The development of Neuro ICUs has been a significant step forward in the care of patients with critical neurological illnesses. By providing a dedicated team of healthcare professionals with specialized training, we can improve patient outcomes and reduce the risk of long-term disability.”
Key ICU Neuro Difference: Patient Population
A hospital ward filled with patients, some connected to breathing tubes and monitors, conveying the specialized care required in an intensive care unit for neurological conditions. Soft lighting illuminates the scene, creating an atmosphere of quiet focus and medical intervention. The patients exhibit a range of neurological symptoms, highlighting the unique challenges and differences between a general ICU and a dedicated neuro ICU. The room’s layout and equipment portray the tailored environment needed to manage this specific patient population.
General ICUs and neuro ICUs care for different types of patients. Each group has unique needs that require special medical care. It’s crucial for doctors to know these differences to provide the best care.
General ICU Patient Profiles
General ICUs handle patients with many serious conditions. These include breathing problems, infections, and issues after surgery. These patients need constant watch and sometimes life-saving treatments.
Common characteristics of general ICU patients include:
- Critical illnesses that are not necessarily neurological in nature
- Need for multi-organ support, including mechanical ventilation and cardiovascular management
- Variable lengths of stay, depending on the severity of their condition and response to treatment
Neuro ICU Patient Profiles
Neuro ICUs focus on patients with brain or spinal cord injuries. This includes strokes, brain trauma, and spinal cord damage. These patients need careful brain monitoring and special treatments.
Key features of neuro ICU patients include:
- Acute neurological conditions that require intensive monitoring and intervention
- Need for specialized neurological care, including intracranial pressure monitoring and neuroimaging
- Often require a multidisciplinary team approach, involving neurologists, neurosurgeons, and rehabilitation specialists
Understanding the unique needs of each patient group helps doctors improve care. The differences between general ICU and neuro ICU patients highlight the need for specialized care in these settings.
Specialized Equipment in Neuro ICUs
A well-lit, high-resolution image of a modern neuro ICU room, showcasing a variety of specialized medical equipment. In the foreground, a sleek, state-of-the-art ventilator with digital displays and advanced monitoring capabilities. In the middle ground, a complex array of IV pumps, infusion devices, and patient monitoring systems, all neatly arranged and illuminated by soft, ambient lighting. In the background, a large, high-definition screen displaying real-time neurological data and brain imaging scans. The overall atmosphere is one of clinical efficiency and technological sophistication, conveying the specialized nature of the neuro ICU environment.
Neuro ICUs use top-notch equipment to care for patients with serious brain injuries or illnesses. The specialized equipment is key for watching and treating critical conditions.
Brain Monitoring Technologies
Brain monitoring tools are vital in neuro ICUs to check brain function all the time. EEG monitoring helps spot seizures or other issues not seen by doctors. It’s especially useful for patients at risk of seizures.
Intracranial Pressure Monitoring Devices
Intracranial pressure (ICP) monitoring is crucial for patients with brain injuries or conditions causing high ICP. These tools let doctors measure and control ICP, helping avoid more brain damage.
Neuroimaging Accessibility
Having neuroimaging tools in the neuro ICU is essential for diagnosing and managing complex brain conditions. This includes CT scanners and MRI machines. They help quickly check on a patient’s condition and guide treatment.
Using these advanced technologies, we can offer detailed care that meets each patient’s specific needs in the neuro ICU.
Staff Expertise and Training Differences
A team of highly specialized neuro ICU staff gathered around a patient’s bed, deeply focused on monitoring vital signs and medical equipment. Soft, directional lighting illuminates their faces, conveying a sense of expertise and concentration. The scene is captured from a low angle, emphasizing the staff’s towering presence and the importance of their work. The background is blurred, keeping the attention on the foreground, where the staff’s extensive training and medical knowledge are on full display.
Staff in neuro ICUs get special training. This makes them different from general ICU staff. They are key to giving top care to patients with serious brain issues.
General ICU Staff Qualifications
General ICU staff are very skilled. They know how to handle sick patients. They can deal with many emergencies. General ICU nurses usually have:
- Basic Life Support (BLS) certification
- Critical care experience
- Ability to operate complex medical equipment
Specialized Training for Neuro ICU Nurses
Nurses in neuro ICUs get extra training. This training helps them understand brain care better. They learn:
- How to do neurological checks and monitoring
- How to care for patients with brain injuries
- How to use special equipment like intracranial pressure monitors
Neuro ICU nurses know how to handle brain problems like seizures and swelling.
Neurointensivist Physicians
Neurointensivist physicians are experts in brain and critical care. They are very important because they:
- Help figure out and treat brain problems
- Work with other doctors to plan care
- Use the best treatments for brain emergencies
Having neurointensivists in the ICU helps patients a lot. They make sure care fits the patient’s brain needs.
The team in neuro ICUs has the best training and knowledge. They are ready to give the best care to patients with serious brain problems.
Neurological Conditions Requiring Specialized ICU Care
A state-of-the-art neuro ICU ward, dimly lit with a soft, muted glow from overhead medical equipment. In the foreground, a patient lies unconscious, various tubes and wires connected to monitoring devices. Nurses and doctors in scrubs move with a sense of urgency, carefully tending to the patient’s needs. The background is a blur of high-tech medical machinery, shelves of medical supplies, and a large window overlooking a city skyline. The atmosphere is one of tense focus and quiet professionalism, as the medical team works to stabilize the patient’s neurological condition.
Neuro ICUs offer critical care for severe neurological conditions. We treat complex disorders needing immediate, specialized attention.
Stroke Management
Stroke management is key in neuro ICU care. We use timely interventions like thrombolytic therapy and mechanical thrombectomy. This helps restore blood flow to the brain.
Our team watches patients closely for signs of brain deterioration. We adjust treatment plans as needed.
Effective stroke care requires a team effort. Neurologists, radiologists, and rehabilitation specialists work together. We create personalized treatment plans for each patient.
Traumatic Brain Injury Care
Traumatic brain injuries need quick, specialized care. Our neuro ICU team manages TBI patients from start to finish. We use advanced monitoring, like intracranial pressure monitoring, to guide treatment.
Traumatic brain injury care is complex. It involves surgery, medication, and rehabilitation therapy. Our goal is to reduce long-term damage and improve patient outcomes.
Seizure Management and Monitoring
Seizure management is crucial in neuro ICU care. This is especially true for patients with seizure disorders or brain injuries. We use continuous EEG monitoring to catch and manage seizures quickly.
Our team uses advanced seizure management protocols to prevent complications. We work with neurologists to adjust medication and plan long-term treatment.
Neurosurgical Recovery
Patients after neurosurgery need close monitoring in the neuro ICU. We provide specialized post-operative care. This includes pain management, infection prevention, and neurological monitoring.
Neurosurgical recovery requires a team effort. Neurosurgeons, intensivists, and rehabilitation specialists work together. Our team ensures patients get comprehensive care and support during recovery.
Treatment Protocols: General ICU vs. Neuro ICU
General ICUs and neuro ICUs have different treatment plans. General ICUs deal with many critical conditions. Neuro ICUs focus on patients with brain injuries or illnesses.
Multi-System Approach in General ICUs
General ICUs use a multi-system approach. They handle many organ systems at once. This is key for patients with complex issues.
For example, a patient with sepsis needs help with breathing, heart, and kidneys. The ICU team must manage these areas well and work together.
- Respiratory support
- Cardiovascular management
- Renal replacement therapy
- Nutritional support
Neurological-Focused Protocols in Neuro ICUs
Neuro ICUs focus on brain care. They deal with strokes, brain injuries, and seizures. Their goal is to help the brain recover and avoid more damage.
They use advanced tools like ICP monitoring and cEEG. These help make treatment decisions.
Protocol Aspect | General ICU | Neuro ICU |
Primary Focus | Multi-organ support | Neurological care |
Monitoring Techniques | Standard vital signs, invasive monitoring | ICP monitoring, cEEG, neuroimaging |
Treatment Strategies | Broad-spectrum antibiotics, vasopressors | Hyperosmolar therapy, seizure management |
Knowing these differences helps healthcare providers understand the unique needs of brain patients. It also shows the special challenges faced by neuro ICUs.
Brain Swelling and Pressure Management
Managing brain swelling and intracranial pressure is key in neurocritical care. It requires a careful balance of treatments and monitoring. We use advanced methods to lower the risks of high intracranial pressure, aiming for the best results for our patients.
Unique Challenges of Intracranial Pressure
Managing intracranial pressure (ICP) is complex. It involves the balance of blood, cerebrospinal fluid, and brain tissue. High ICP can cause serious problems, like brain herniation and death. We must watch and control ICP closely to avoid these dangers.
Handling ICP is not just about the medical issue. It also depends on the patient’s health and how they react to treatment. Early detection and intervention are key to reducing the risks of high ICP.
Specialized Interventions in Neuro ICUs
Neuro ICUs have special treatments for managing intracranial pressure. These include osmotherapy, which uses osmotic agents to shrink brain swelling. There’s also cerebrospinal fluid drainage, which lowers ICP by removing extra fluid.
We also use sedation and analgesia to lessen stress and pain, which can raise ICP. Additionally, we use advanced neuromonitoring techniques to keep an eye on brain activity. This helps us adjust our treatments as needed.
With these specialized treatments, we can manage intracranial pressure well. This improves patient outcomes in neuro ICUs.
Ventilator Management Differences
Ventilator management varies between general ICUs and neuro ICUs. General ICUs handle a wide range of critical conditions. Neuro ICUs focus on patients with neurological injuries or disorders, needing special care.
General Respiratory Support in ICUs
In general ICUs, the main goal is to help patients with respiratory failure. This can be due to pneumonia, sepsis, or trauma. The aim is to provide enough oxygen and ventilation without harming the lungs.
Ventilator settings are adjusted based on the patient’s condition. This includes factors like tidal volume, respiratory rate, and PEEP. Lung-protective ventilation strategies are used to prevent lung injury from the ventilator.
Neuro-Specific Ventilation Strategies
Neuro ICUs take a more detailed approach to ventilator management. This is especially true for patients with TBI, stroke, or other neurological conditions. The main goal is to manage intracranial pressure (ICP) and ensure proper blood flow to the brain.
Neuro-specific ventilation strategies aim to avoid worsening brain injury. This is done by controlling CO2 levels, which affect blood flow and ICP. Hyperventilation can be used to lower ICP, but it must be done carefully to avoid causing ischemia.
Neuro ICUs use advanced neuromonitoring techniques. This allows for precise adjustments to ventilator settings based on real-time data. This approach is key to improving outcomes for patients with severe neurological injuries.
Neuro ICU Guidelines and Best Practices
Quality neurocritical care is built on evidence-based protocols and guidelines. These standards are key to ensuring patients get consistent, top-notch care. This is true no matter their specific neurological condition.
Evidence-Based Protocols
Neuro ICUs stick to evidence-based protocols based on the latest research and clinical trials. These protocols cover many areas of neurocritical care. This includes managing traumatic brain injuries, stroke, and seizures.
By following these guidelines, healthcare providers can give patients the most effective treatments. This is crucial for their recovery.
Some important parts of these protocols include:
- Standardized tools for checking neurological health
- Guidelines for managing intracranial pressure
- Protocols for sedation and pain relief in neurocritical care
- Proven ways to prevent complications
Quality Metrics in Neurocritical Care
Neuro ICUs also focus on quality metrics to measure and better patient care. These metrics include things like:
- How long patients stay in the ICU
- Mortality rates
- Complication rates (like ventilator-associated pneumonia)
- Patient satisfaction scores
By watching these metrics, neuro ICUs can spot areas to get better. They then make changes to improve patient outcomes. This is key to effective neuro ICU management.
We know neurocritical care is always changing. So, our guidelines and best practices are always being updated. This keeps us at the leading edge of neuro ICU care. It ensures our patients get the best treatment possible.
Patient Outcomes and Recovery Trajectories
It’s key to know how patients do and how they get better in different ICUs. The care they get really shapes their recovery paths.
Outcome Measurements in General ICUs
In general ICUs, doctors look at how patients get better overall. They check if vital signs are stable, if infections are controlled, and if organs are working right. They use scores like APACHE II or SAPS II to guess how likely a patient is to die in the hospital.
How well a patient does in a general ICU depends on their starting health, any other health issues they have, and how well they respond to treatment. Early mobilization and family-centered care help improve patient outcomes.
Neurological Recovery Metrics
In neuro ICUs, doctors focus on how well the brain is working. They check cognitive function, use scales like the NIH Stroke Scale, and manage pressure inside the brain. These are key to tracking patients with brain injuries or conditions.
Recovery for neuro ICU patients is more complex. It’s not just about keeping vital signs stable. It’s also about getting the brain to function right again. Rehabilitation starts early, with a team that includes neurologists, neurosurgeons, and therapists.
Understanding these differences helps doctors give better care. This leads to better patient outcomes and recovery trajectories.
When Patients Transfer Between Units
The decision to move a patient to or from a neuro ICU depends on their medical needs. As their condition changes, they might need more or less care. This could mean moving them to a different unit.
Criteria for Transfer to Neuro ICU
Patients often go to a neuro ICU for specialized care they can’t get elsewhere. This includes those with severe brain injuries, stroke, or other neurological issues. They need close monitoring and advanced treatments.
The reasons for moving to a neuro ICU include:
- Severe neurological deficits requiring close monitoring
- Need for advanced brain monitoring technologies
- Presence of conditions that may lead to rapid neurological deterioration
For example, a patient with a stroke in a general ICU might need to move to a neuro ICU. This is if their condition gets worse or they need more specialized care, like monitoring of intracranial pressure.
Transitioning from Neuro ICU to General ICU
When a patient no longer needs the intense care of a neuro ICU, they might move to a general ICU. This decision is based on their clinical stability and if the general ICU can handle their ongoing needs.
The steps for this transition include:
- Assessing the patient’s neurological stability
- Evaluating the need for continued close monitoring
- Ensuring the general ICU is equipped to handle the patient’s remaining care needs
Transfer Criteria | Neuro ICU to General ICU | General ICU to Neuro ICU |
Primary Reason | Patient no longer requires intensive neurological care | Patient requires specialized neurological care |
Key Factors | Clinical stability, reduced need for close monitoring | Severe neurological deficits, need for advanced monitoring |
Care Needs | Ongoing medical care without intensive neurological interventions | Advanced neurological care and monitoring |
By managing transfers carefully, we make sure patients get the right care. This helps improve their recovery and outcomes.
Conclusion
We’ve looked into the big differences between ICUs and neuro ICUs. We’ve seen how special care for brain issues is crucial. This care is key for patients with severe brain injuries or illnesses.
Neuro ICUs have the latest tech and teams with special training. They can handle the complex needs of brain patients. This helps patients get better faster.
Knowing the difference between ICUs and neuro ICUs is vital. It helps make sure patients get the right care. This leads to better health outcomes for them.
As medical tech and care methods get better, neuro ICUs will keep being important. They show the value of focused care for brain patients. This care improves lives for patients and their families.
FAQ
What is the main difference between an ICU and a neuro ICU?
ICUs handle patients with serious illnesses. Neuro ICUs focus on those with brain issues like stroke or brain injuries.
What kind of patients are typically treated in a general ICU?
General ICUs see patients with severe illnesses or injuries. This includes trauma, infections, and complications after surgery.
What specialized equipment is found in neuro ICUs?
Neuro ICUs have advanced tools for brain monitoring. They also have devices to check intracranial pressure and imaging for brain scans.
How does staff expertise differ between general ICUs and neuro ICUs?
Neuro ICU teams get special training in brain care. This lets them focus on complex brain conditions.
What are some common neurological conditions treated in neuro ICUs?
Neuro ICUs deal with stroke, brain injuries, seizures, and recovery from brain surgery.
How do treatment protocols differ between general ICUs and neuro ICUs?
General ICUs use a broad approach. Neuro ICUs have specific plans for brain injuries or disorders.
What are the unique challenges of managing intracranial pressure in neuro ICUs?
Managing brain pressure in neuro ICUs is complex. It involves monitoring and treatments to reduce swelling and improve brain flow.
How do ventilator management strategies differ in neuro ICUs compared to general ICUs?
Neuro ICUs use special ventilation methods. These methods aim to protect the brain while ensuring enough oxygen.
What guidelines and best practices are followed in neuro ICUs?
Neuro ICUs follow proven care plans and quality standards. This ensures top care for brain patients.
How are patient outcomes measured in neuro ICUs compared to general ICUs?
Neuro ICUs track brain recovery metrics. These are different from the measures used in general ICUs.
When is a patient transferred to a neuro ICU, and what are the criteria for transfer?
Patients go to neuro ICUs for brain-focused care. The criteria include needing brain monitoring, advanced treatments, and specialized care.
What happens when a patient is transitioned from a neuro ICU to a general ICU?
When a patient’s condition improves, they might move to a general ICU. This ensures they get the right care as their needs change.
References
National Center for Biotechnology Information. ICU versus Neuro ICU Critical Care Differences. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21519958/