Diabetes is a chronic disease that affects how our body uses sugar. It’s the fastest-growing global health issue. In the United States, 38.4 million people live with diabetes, which is 11.6 percent of the population. Finding it early is key.
Many Americans with diabetes don’t know they have it. Healthcare providers use proven methods to find it before symptoms show. This helps prevent serious damage.
The 3 P’s in diabetes – eating a lot, drinking a lot, and going to the bathroom a lot – are important signs. Knowing these symptoms and risk factors helps us give better care.
Key Takeaways
- Diabetes affects 11.6% of the US population.
- Early detection is critical for effective management.
- The 3 P’s (polyphagia, polydipsia, polyuria) are significant indicators.
- Trusted healthcare providers use evidence-based screening.
- Comprehensive care can prevent serious health complications.
The Diabetes Epidemic: Understanding the Scope
The global diabetes epidemic is a pressing concern that demands immediate attention from healthcare providers worldwide. Understanding the scope of this problem is key to developing effective management and treatment strategies.
Current Statistics in the United States
In the United States, diabetes affects a significant portion of the adult population. The statistics underscore the need for vigilant screening and early intervention to prevent long-term complications associated with diabetes.
We must recognize that diabetes is not just a personal health issue but also a public health concern. It requires a broad approach for prevention, diagnosis, and management.
Global Prevalence and Future Projections
Globally, about 537 million people between 20 and 79 years old live with diabetes. By 2045, this number is expected to rise to over 783 million. The growing prevalence is attributed to various factors, including rising obesity rates, sedentary lifestyles, and an aging population.
Understanding these trends is essential for healthcare providers to prepare for the increasing demand for diabetes care. They need to develop targeted interventions that address the root causes of the condition.
The Undiagnosed Population
A concerning aspect of the diabetes epidemic is the number of individuals who remain undiagnosed. It is estimated that 22.8 percent of adults with diabetes are unaware of their condition. This undiagnosed population is at risk of developing serious complications due to the lack of appropriate management and treatment.
We must emphasize the importance of awareness and screening programs. These programs help identify individuals with undiagnosed diabetes, ensuring they receive timely and appropriate care.
Why Early Detection is Critical for Client Outcomes
Early detection is key to managing diabetes well. It lets us start treatments early. These treatments can change the disease’s path and prevent serious problems.
Preventing Long-term Complications
Early detection helps avoid serious health issues. Diabetes can cause heart disease, kidney damage, eye problems, and nerve damage. Finding diabetes early means we can start treatments that lower these risks.
Studies show early treatment can cut the risk of diabetes complications by half. This is why finding diabetes early is so important.
“Early detection and treatment of diabetes can significantly reduce the risk of complications and improve quality of life for individuals with the disease.”
Economic and Quality of Life Impact
Early detection also saves money and improves life quality. Diabetes costs a lot, both in medical bills and lost work time. Managing diabetes well from the start can cut these costs and make life better for those affected.
Aspect | Early Detection | Late Detection |
Complication Rate | Lower | Higher |
Healthcare Costs | Reduced | Increased |
Quality of Life | Improved | Reduced |
The Asymptomatic Progression Challenge
Type 2 diabetes often goes unnoticed for years. It’s called asymptomatic progression. Many people don’t know they have it until they start showing symptoms or get checked for other reasons.
Waiting too long to find diabetes can lead to poor management and more serious problems. So, it’s vital to find and screen those at risk early.
By focusing on early detection and tackling the challenge of asymptomatic progression, we can help our clients better and reduce diabetes’s impact.
The Classic 3 P’s of Diabetes: Primary Indicators
The 3 P’s of diabetes – polyuria, polydipsia, and polyphagia – are key to diagnosing the condition. These signs are vital for doctors to spot diabetes early and start the right treatment.
Polyuria: Understanding Excessive Urination Patterns
Polyuria means going to the bathroom a lot or having too much urine. It happens when there’s too much sugar in the blood. This makes the kidneys make more urine, causing dehydration and thirst.
Characteristics of Polyuria:
- Frequent trips to the bathroom
- Large amounts of urine
- Nocturia (waking up at night to urinate)
Polydipsia: Recognizing Abnormal Thirst
Polydipsia is when you feel very thirsty and want to drink a lot. It’s linked to polyuria because the body tries to replace lost fluids. Drinking a lot can make polyuria worse.
Signs of Polydipsia:
- Constant feeling of thirst
- Drinking large amounts of fluids
- Dry mouth and dehydration
Polyphagia: Assessing Increased Appetite
Polyphagia is when you feel hungrier than usual. In diabetes, this happens because your cells can’t get the glucose they need. This makes you feel hungry all the time.
Indicators of Polyphagia:
- Increased hunger
- Eating more frequently or in larger quantities
- Feeling unsatisfied after eating
To better understand the relationship between the 3 P’s, let’s examine the following table:
Symptom | Description | Related Consequence |
Polyuria | Frequent or excessive urination | Dehydration, disrupted sleep |
Polydipsia | Excessive thirst and fluid intake | Consuming large quantities of fluids, potentially worsening polyuria |
Polyphagia | Increased appetite or hunger | Consuming more calories, potentially leading to weight changes |
Understanding the 3 P’s of diabetes is key for early detection and management. Recognizing polyuria, polydipsia, and polyphagia helps doctors start timely treatments to improve patient outcomes.
Beyond the 3 P’s: Secondary Symptoms to Monitor
The classic 3 P’s are known signs of diabetes. But, there are other important secondary symptoms to watch. These signs can help doctors spot diabetes, even when the usual symptoms are not there.
Unexplained Weight Loss Despite Increased Appetite
Unexplained weight loss is a key secondary symptom. It happens when the body can’t use glucose well. This leads to fat and muscle breakdown for energy. People might lose weight without feeling hungry, which can be confusing.
Fatigue and Energy Depletion
Fatigue is another sign of diabetes. When cells don’t get enough glucose, they feel tired. This tiredness can really affect someone’s life and daily activities.
- Feeling tired all the time
- Lack of energy for daily activities
- General malaise
Impaired Wound Healing and Recurrent Infections
Diabetes makes it hard for wounds to heal and for the body to fight infections. High blood sugar weakens white blood cells. This means injuries and infections take longer to heal, leading to recurrent infections.
Symptom | Description |
Impaired wound healing | Slow recovery from cuts and bruises |
Recurrent infections | Frequent occurrence of infections, mainly skin and urinary tract infections |
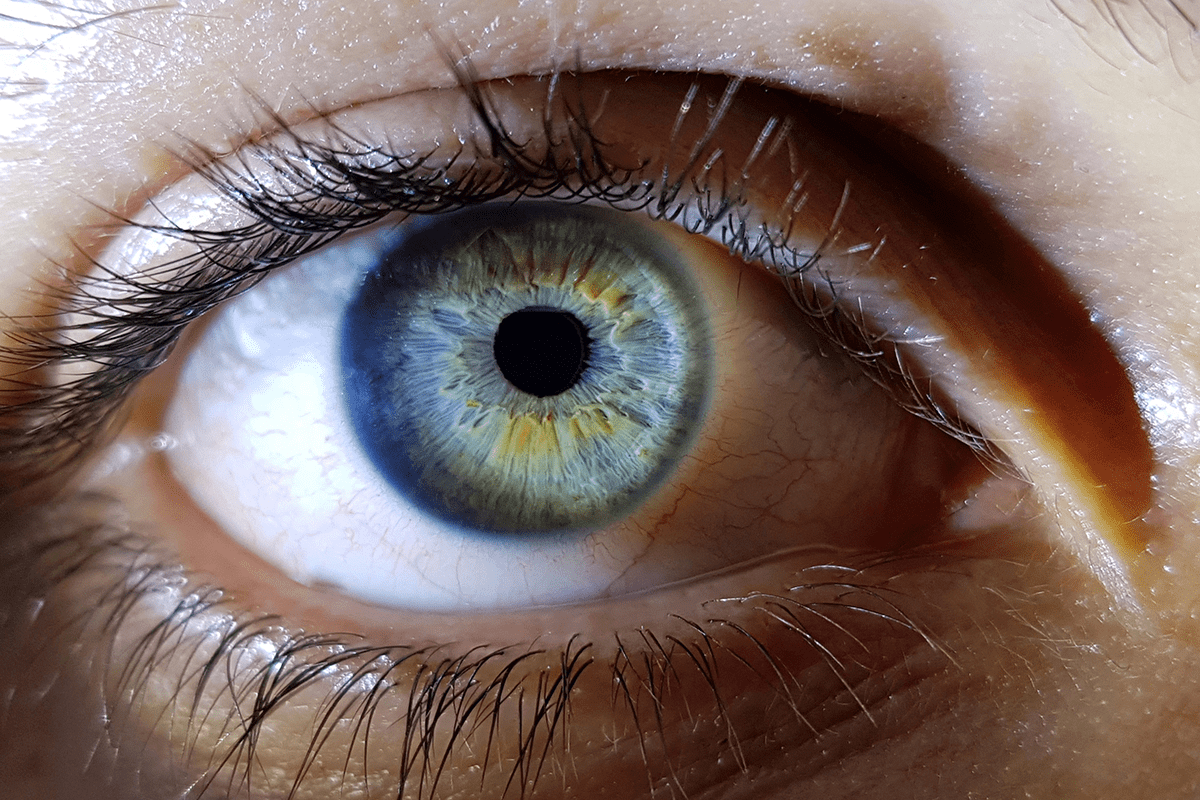
Blurred Vision and Other Sensory Changes
Blurred vision can happen when blood sugar is high. It affects the eye’s lens, causing vision problems. Other changes, like numbness in hands and feet, can also occur.
Spotting these secondary symptoms early is key to managing diabetes. Knowing these signs helps doctors act fast and improve patient care.
Subtle and Easily Missed Symptoms
Diabetes can show itself in ways that are not obvious. It’s important to notice these signs early to catch the disease before it gets worse.
Skin Manifestations: Acanthosis Nigricans and Skin Tags
Skin changes can signal diabetes. Acanthosis nigricans is dark, velvety skin patches in folds. It’s linked to insulin resistance, a sign of type 2 diabetes. Also, skin tags, small growths, can show up where skin rubs together.
These signs might seem small, but they’re important. If you’re at risk for diabetes, don’t ignore them.
Skin Condition | Description | Association with Diabetes |
Acanthosis Nigricans | Dark, velvety skin patches | Strongly associated with insulin resistance |
Skin Tags | Small, benign growths | May be more common in individuals with diabetes |
Neurological Symptoms: Tingling and Numbness
Diabetes can harm nerves, causing tingling and numbness in hands and feet. This is called diabetic neuropathy. It’s a sign that diabetes might be present.
Spotting these symptoms early is key. It helps manage the condition and stops more nerve damage.
Mood Changes and Cognitive Effects
Diabetes can affect your mood and brain function. You might feel mood swings, irritability, or trouble focusing. These signs are not always obvious.
It’s important to know how diabetes affects mental health. Doctors should look for these signs to help patients get the right care.
Identifying When a Client Has Diabetes: Clinical Assessment Strategies
To spot diabetes, we use history, physical checks, and specific questions. As doctors, we must watch for diabetes signs early.
Comprehensive History Taking Techniques
Getting a full history is key to diagnosing diabetes. We start by asking about family history of diabetes and medical history. We also look at lifestyle factors like diet and exercise.
- Assess the client’s family history of diabetes.
- Inquire about previous diagnoses of prediabetes or gestational diabetes.
- Evaluate lifestyle factors, including diet and physical activity.
Physical Examination Key Focus Areas
In the physical exam, we look for signs of diabetes. We check for obesity and skin signs like acanthosis nigricans. We also search for neurological problems like nerve damage.
- Assess for obesity, focusing on central obesity.
- Examine for skin signs linked to diabetes.
- Look for signs of nerve damage.
Effective Screening Questions for Healthcare Providers
Right questions help find diabetes risk. We ask about hyperglycemia symptoms like frequent urination. We also check for vascular disease history and glucose test results.
- Inquire about symptoms of hyperglycemia.
- Ask about history of vascular disease.
- Review any previous glucose testing results.
By using history, physical exams, and specific questions, we can better find diabetes. This helps us act fast to help our patients.
High-Risk Profiles: Who Needs Closer Monitoring
It’s key to spot high-risk profiles early to catch diabetes. Some people are more likely to get diabetes because of certain risk factors. We’ll look at these factors closely.
Age, Ethnicity, and Family History Considerations
Age is a big risk factor for diabetes, with risk going up after 45. Ethnicity also matters, with African Americans, Hispanics/Latinos, and American Indians at higher risk. A family history of diabetes also raises your risk.
- Age: Risk increases after 45 years.
- Ethnicity: Higher risk in African Americans, Hispanics/Latinos, and American Indians.
- Family History: Having a first-degree relative with diabetes increases risk.
Comorbid Conditions as Warning Signs
Certain health conditions can warn us of diabetes. These include high blood pressure, abnormal cholesterol levels, and polycystic ovary syndrome (PCOS). We need to watch people with these conditions for diabetes signs.
- Hypertension: High blood pressure can be a precursor to diabetes.
- Dyslipidemia: Abnormal lipid profiles are associated with increased diabetes risk.
- PCOS: Women with PCOS are at higher risk of developing insulin resistance and diabetes.
Lifestyle and Environmental Risk Factors
Lifestyle and environment also affect diabetes risk. A sedentary lifestyle, bad diet, and obesity are big risks. We should push people to live healthier to lower these risks.
- Sedentary Lifestyle: Lack of physical activity increases diabetes risk.
- Diet: Eating too much sugar and saturated fats raises risk.
- Obesity: Being overweight or obese is a major risk factor for type 2 diabetes.
Knowing these high-risk profiles helps us find people who need diabetes checks. Signs like polyuria, polydipsia, and polyphagia should prompt action. Early detection and regular checks can lead to better health outcomes.
Diagnostic Approaches and Interpretation
Getting a correct diabetes diagnosis is key for managing the disease well. We use a mix of doctor’s checks and lab tests to spot diabetes.
Fasting Plasma Glucose and Oral Glucose Tolerance Tests
Fasting Plasma Glucose (FPG) and Oral Glucose Tolerance Tests (OGTT) are key tools. FPG checks blood sugar after not eating for a night. OGTT looks at how well the body handles sugar after drinking a sweet drink.
These tests help find diabetes and prediabetes. For example, a fasting glucose of 126 mg/dL or more, or an OGTT of 200 mg/dL or more, means you have diabetes.
HbA1c Testing and Continuous Glucose Monitoring
HbA1c testing shows blood sugar levels over 2-3 months. This test is key for checking long-term sugar control. Continuous Glucose Monitoring (CGM) tracks sugar levels all day, showing trends and patterns.
HbA1c and CGM are great for diagnosing and managing diabetes. An HbA1c of 6.5% or higher means you have diabetes.
Differential Diagnosis: Conditions with Similar Presentations
When we diagnose diabetes, we must think of other conditions that might look similar. Differential diagnosis is key to make sure we get the right diagnosis and treatment.
- Urinary tract infections
- Kidney disease
- Other endocrine disorders
When to Refer to Endocrinology
It’s wise to see an endocrinologist for complex cases, like type 1 diabetes, or when we’re not sure about the diagnosis. Specialist care can offer more help in managing diabetes and related issues.
By knowing and using these diagnostic methods, we can make sure people get the right diagnosis and care for diabetes.
Special Population Considerations
We must consider the diverse needs of different populations when assessing for diabetes. Different populations require tailored approaches to diagnosis and management.
Pediatric Clients: Type 1 vs. Type 2 Presentation
In pediatric clients, diabetes assessment involves distinguishing between Type 1 and Type 2 diabetes. Type 1 diabetes is an autoimmune condition, while Type 2 is often associated with obesity and insulin resistance.
Type 1 Diabetes typically presents with rapid onset of symptoms, including polydipsia (excessive thirst), polyuria (frequent urination), and weight loss. In contrast, Type 2 Diabetes may have a more gradual onset and is often linked to lifestyle factors.
Characteristics | Type 1 Diabetes | Type 2 Diabetes |
Typical Age of Onset | Children and adolescents | Often in older children and adolescents |
Body Weight | Typically normal or underweight | Often overweight or obese |
Autoantibodies | Present | Usually absent |
Insulin Requirement | Immediate need | May not require insulin initially |
Geriatric Assessment Challenges
Geriatric patients present unique challenges in diabetes assessment due to comorbidities, polypharmacy, and age-related changes in glucose metabolism.
Healthcare providers must be vigilant for signs of diabetes in older adults, such as fatigue, cognitive impairment, and recurrent infections. A thorough geriatric assessment is key for early detection and management.
Pregnancy and Gestational Diabetes Screening
Pregnancy is a critical period for diabetes screening due to the risk of gestational diabetes mellitus (GDM). GDM increases the risk of complications for both mother and fetus.
Universal screening for GDM is recommended between 24 and 28 weeks of gestation. Early screening is advised for high-risk pregnancies.
Cultural Competence in Symptom Recognition
Cultural competence is essential in recognizing diabetes symptoms across diverse populations. Understanding cultural differences in health beliefs and behaviors can improve diabetes detection and management.
Healthcare providers should be aware of cultural nuances that may affect symptom reporting and healthcare-seeking behaviors.
Conclusion: Implementing Effective Screening Protocols
It’s key to have good screening methods to find diabetes early. This helps lower the chance of serious problems and makes clients’ lives better. By spotting the 3 P’s of high blood sugar – too much pee, thirst, and hunger – doctors can start helping sooner.
Good screening helps doctors catch diabetes early, even when there are no symptoms yet. This early action can prevent big problems later. It also makes life better for people with diabetes.
Following the advice in this article helps doctors spot and handle diabetes better. This leads to better health for their clients. Using effective screening is a big part of caring for diabetes well. It’s vital for giving top-notch care to patients.
FAQ
What are the classic 3 P’s of diabetes?
The classic 3 P’s of diabetes are polyuria (excessive urination), polydipsia (abnormal thirst), and polyphagia (increased appetite). These signs are key for doctors to spot diabetes early.
What is polyuria and polydipsia?
Polyuria means you pee a lot. Polydipsia is when you feel very thirsty. Both often happen together in people with diabetes.
Why is early detection of diabetes important?
Finding diabetes early is vital. It helps avoid serious problems, saves money, and improves life quality. Type 2 diabetes often goes unnoticed for years, making early detection key.
What are the secondary symptoms of diabetes beyond the classic 3 P’s?
Other signs of diabetes include unexplained weight loss, feeling tired, and wounds that won’t heal. You might also see blurred vision or other sensory changes.
Who is at high risk for developing diabetes?
People with a family history of diabetes, certain ethnicities, and obesity or high blood pressure are at higher risk. Age and lifestyle also play a big role in risk.
How is diabetes diagnosed?
Doctors use tests like fasting plasma glucose, oral glucose tolerance tests, and HbA1c testing to diagnose diabetes. Continuous glucose monitoring is also used in some cases.
Are there special considerations when assessing for diabetes in certain populations?
Yes, kids, older adults, pregnant women, and people from different cultures need special care. Healthcare providers must know these differences to give the best care.
What is the significance of acanthosis nigricans in diabetes?
Acanthosis nigricans is a skin issue linked to insulin resistance, a sign of type 2 diabetes risk. Seeing it means you might be at risk for diabetes.
How can healthcare providers improve their ability to identify and manage diabetes?
Healthcare providers can do better by following good screening methods, knowing the 3 P’s and other symptoms, and understanding who’s at risk. This helps them spot and manage diabetes better.
References
National Center for Biotechnology Information. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9810477/