
Medical imaging procedures are key in today’s healthcare. They help doctors make accurate diagnoses and plan treatments. At Liv Hospital, we know how important it is for patients to know about the benefits and risks of these tests. Learn 12 shocking facts aboutimaging radiation. Our guide covers the risks and safety of common medical imaging procedures.
Every year, about 4.2 billion medical imaging tests are done worldwide. This is according to the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) 2020/2021 report. Patients need to understand how radiation imaging helps in their care.
We use the latest technology to keep our patients safe. By knowing the facts about medical imaging radiation, patients can make better choices about their health.
Key Takeaways
- Medical imaging is a critical tool in modern healthcare.
- Approximately 4.2 billion medical imaging examinations are conducted worldwide each year.
- Understanding radiology facts is essential for patient safety.
- Radiation imaging plays a vital role in diagnosis and treatment planning.
- Staying informed about medical imaging procedures is critical for patients.
The Prevalence of Medical Imaging in Modern Healthcare
Diagnostic imaging exams are key in today’s medicine. They let doctors see inside the body. These exams are often done, and in many ways, show how vital they are for patient care.
Medical imaging is used more than ever. It’s estimated that 3.6 billion diagnostic imaging exams are done worldwide each year. This shows how important it is for health care.
Fact 1: 3.6 Billion Diagnostic Imaging Exams Performed Globally Each Year
The number of imaging exams shows how important they are in diagnosing and treating patients. This huge number shows imaging tech is used everywhere in health care.
How often imaging is done varies by age and health condition. For example, older people have more exams because they often have chronic diseases.
Fact 2: Radiography is the Most Common Imaging Procedure (783 Exams per 1,000 People)
Radiography is the most used imaging method, with about 783 exams per 1,000 people. It’s popular because it’s easy to get, not expensive, and works well for many health issues.
Radiography’s big role in imaging shows its value. Doctors trust it a lot for making diagnoses.
Understanding Imaging Radiation and How It Works
Knowing how imaging radiation works is key for both doctors and patients. It helps them make smart choices about tests. Medical imaging is a big part of today’s healthcare.
Different Types of Medical Radiation
Medical imaging uses two main types of radiation: ionizing and non-ionizing. Ionizing radiation, like X-rays and gamma rays, can remove electrons from atoms. This is used in many tests, including X-rays and CT scans.
Non-ionizing radiation, like ultrasound and MRI, doesn’t have enough energy to remove electrons. MRI is not traditional radiation, but it’s often talked about with other imaging methods because of its ability to show detailed images.
How Radiation Creates Diagnostic Images
Ionizing radiation makes images by going through the body. X-rays, for example, pass through soft tissue but are blocked by bone. This contrast helps doctors see inside the body.
In nuclear medicine, tiny amounts of radioactive material are used. These materials emit gamma rays that cameras detect. This helps create images of how the body works.
Measuring Radiation Exposure in Medical Procedures
Doctors measure radiation from tests in different ways. They use the dose area product (DAP), computed tomography dose index (CTDI), and effective dose. The effective dose is in millisieverts (mSv) and considers how different parts of the body react to radiation.
| Modality | Typical Effective Dose (mSv) | Equivalent Background Radiation |
| Chest X-ray | 0.1 | 10 days |
| CT Abdomen/Pelvis | 10 | 3 years |
| Bone Scan | 4.8 | 1.6 years |
Knowing about radiation risks is important for patient safety. Understanding imaging radiation is the first step in making good choices about medical tests.
Common Radiation-Based Imaging Procedures
We use different radiation-based imaging methods to find and treat health issues. These methods are key in today’s healthcare. They give us important info that helps us decide how to treat patients.
X-Rays: Applications and Typical Doses
X-rays are a common tool in medical imaging. They help us see bones, teeth, and other inside parts. X-rays are great for spotting breaks, finding objects inside the body, and checking the lungs.
The dose from one X-ray is usually low. But it can change based on where in the body it’s taken and the method used.
For example, a chest X-ray has a very low dose. But a CT scan of the belly and pelvis has a much higher dose. Knowing these differences helps doctors and patients make better choices about imaging.
CT Scans: When They’re Necessary
Computed Tomography (CT) scans give detailed images of the body. They’re good for finding tumors, vascular diseases, and internal injuries. CT scans are a big part of medical radiation, making up about 62.6% of it.
New tech like photon-counting CT (PCCT) makes CT scans safer. They give clearer images with less radiation. We use CT scans when we need detailed images for diagnosis and treatment, like in emergency cases.
Nuclear Medicine: Diagnostic and Therapeutic Applications
Nuclear medicine uses tiny amounts of radioactive materials to diagnose and treat diseases. It’s great for seeing how organs and tissues work. Techniques like Positron Emission Tomography (PET) scans help find cancers, brain disorders, and heart diseases.
Nuclear medicine is customized for each condition. It offers both diagnostic and treatment benefits. The radiation from these procedures is managed carefully to ensure the benefits are worth the risks.
Imaging Radiation: Comparing Exposure Levels Across Procedures
Medical imaging uses different amounts of radiation for each procedure. This is important to know the risks and benefits of each imaging method.
Relative Radiation Doses from Different Imaging Modalities
Various imaging methods give out different amounts of radiation. For example, a chest X-ray uses about 0.1 millisieverts (mSv). On the other hand, a CT scan of the abdomen and pelvis can expose a patient to around 10 mSv. Here’s a list of common imaging procedures and their radiation doses:
- X-ray: 0.01-0.1 mSv
- CT Scan (head): 1-2 mSv
- CT Scan (abdomen and pelvis): 10-20 mSv
- Positron Emission Tomography (PET) Scan: 5-7 mSv
Knowing these doses helps doctors pick the best imaging method for each patient. This way, they can reduce radiation exposure.
Comparing Medical Radiation to Natural Background Exposure
It’s useful to compare medical radiation to natural background radiation. The average person gets about 2.4 mSv of background radiation each year. A simple X-ray has a dose similar to a few days of background radiation. But, CT scans can have doses like several years of background radiation.
Cumulative Effects of Multiple Imaging Procedures
Getting multiple imaging procedures is a big concern. Studies show over 1% of patients get more than 100 mSv from repeated scans. Children are at higher risk of blood cancers from this radiation. So, it’s key to keep track of each patient’s total radiation dose.
We need to weigh the benefits of imaging against the risks of radiation. This way, we can make sure patients get the info they need without too much radiation.
Technological Advances Reducing Radiation Exposure
Medical imaging technology is key to keeping patients safe while getting accurate diagnoses. It’s important to lower radiation exposure as we use these technologies more.
Photon-Counting CT (PCCT) Technology Offers Higher Resolution at Lower Doses
Photon-counting CT (PCCT) is a big step forward in CT scanning. It counts each photon’s energy, unlike old CT scanners. This means better images with less radiation.
PCCT gives clearer images, less noise, and better tissue differentiation. It’s great for those needing many CT scans, as it cuts down radiation over time.
Digital Radiography vs. Traditional Film
Digital radiography has taken over from film in today’s medicine. It offers lower radiation, quicker images, and better storage and sharing.
| Feature | Digital Radiography | Traditional Film |
| Radiation Exposure | Lower doses possible | Fixed dose required |
| Image Acquisition Time | Instantaneous | Several minutes |
| Image Storage | Electronic, easily accessible | Physical storage required |
Dose Optimization Software and Techniques
Dose optimization software is vital for lowering radiation in imaging. It adjusts settings for patient size, age, and the needed scan.
Some key techniques include:
- Automatic exposure control (AEC)
- Iterative reconstruction algorithms
- Tube current modulation
These tools help doctors reduce radiation while keeping image quality high.
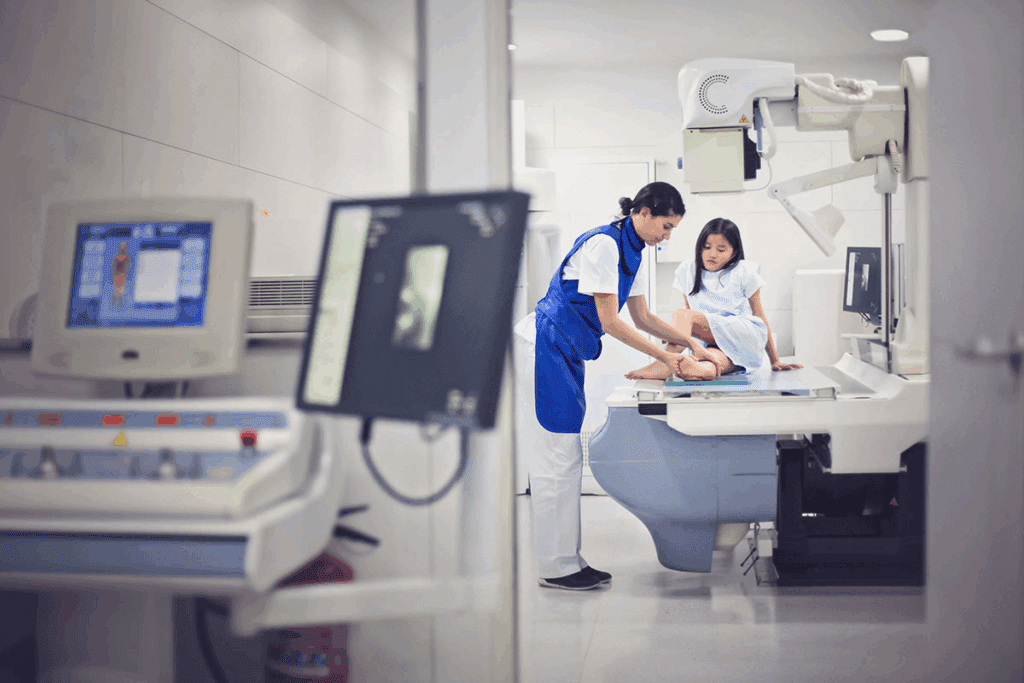
Special Considerations for Pediatric Imaging
Children are not just small adults. Their bodies are more sensitive to imaging radiation. This means we need special ways to handle medical imaging for kids.
Fact 6: Children Face Increased Risk from Imaging Radiation
Children’s bodies are more at risk from radiation because their cells are growing fast. They have a longer life ahead, which means any damage from radiation could show up later.
So, we must think carefully about the need for imaging tests in kids. We aim to get the most important information while keeping the radiation dose low.
Fact 7: Up to 10% of Hematologic Malignancies in Children May Be Preventable
Studies show that up to 10% of blood cancers in kids might be caused by radiation from medical tests. This highlights the need to use radiation wisely in kids’ care.
By using pediatric-specific protocols, we can cut down on radiation. This might help lower the chance of cancer caused by radiation.
Pediatric-Specific Protocols and Safety Measures
Healthcare teams are creating special plans for kids. They adjust radiation doses based on a child’s size and age. They also try to use other imaging methods when they can.
- Adjusting radiation doses based on patient size and age
- Using alternative imaging modalities like ultrasound or MRI when appropriate
- Ensuring that imaging procedures are justified and optimized
These steps help us get accurate images while keeping kids safe from too much radiation.
Non-Ionizing Alternatives to Radiation-Based Imaging
Non-ionizing imaging is safer and reduces radiation exposure. Techniques like ultrasound and MRI are key in our diagnostic tools.
Ultrasound and MRI Provide Radiation-Free Diagnostic Options
Ultrasound and MRI are leading non-ionizing imaging methods. Ultrasound uses sound waves to see inside the body. It’s great for checking organs and monitoring babies during pregnancy.
MRI (Magnetic Resonance Imaging) uses a magnetic field and radio waves. It’s best for soft tissue images, like the brain and joints.
- Ultrasound is portable, affordable, and doesn’t use ionizing radiation.
- MRI gives detailed images of soft tissues without radiation.
When to Choose Non-Ionizing Alternatives
Choosing non-ionizing imaging depends on the diagnosis needed, patient history, and clinical needs. Pregnant women and kids often get these scans to avoid radiation.
Non-ionizing alternatives are recommended in several situations:
- For conditions that don’t need ionizing imaging’s high detail.
- For patients at high risk from radiation, like kids and pregnant women.
- When frequent scans are needed, these methods can be used more safely.
Limitations of Non-Radiation Imaging Techniques
Non-ionizing imaging has many benefits but also some drawbacks. For example, ultrasound might not show as much detail as CT scans for some issues. MRI can’t be used by people with certain implants or pacemakers.
Some main limitations are:
- Ultrasound images depend on the skill of the operator.
- MRI is more expensive and less common than other scans.
- Some conditions are harder to diagnose with non-ionizing methods.
Knowing the pros and cons of non-ionizing imaging helps us make better choices. This improves patient care and safety.
Balancing Diagnostic Benefits Against Radiation Risks
Medical imaging is key in healthcare, but we must weigh its benefits against radiation risks. As we use imaging more for diagnosis and treatment, knowing this balance is vital.
The ALARA Principle in Medical Imaging
The ALARA principle means keeping radiation exposure as low as possible. It’s about getting the needed diagnostic info without too much radiation. This principle helps ensure patients get imaging benefits while reducing radiation exposure.
Implementing ALARA involves several key strategies:
- Using the lowest dose necessary for diagnostic-quality images
- Optimizing imaging protocols for different patient populations
- Regularly maintaining and updating imaging equipment
- Training personnel in dose optimization techniques
Risk-Benefit Analysis in Diagnostic Decision-Making
Healthcare providers must weigh imaging benefits against radiation risks. This is critical for vulnerable groups like children or pregnant women.
The decision to use imaging with ionizing radiation should be based on:
- The medical necessity of the procedure
- The availability of non-ionizing imaging methods
- The patient’s individual risk factors and medical history
Populations at Higher Risk from Radiation Exposure
Some groups face higher risks from radiation. Knowing these risks helps make better imaging decisions.
| Population | Risk Factors | Precautions |
| Children | Developing tissues, longer life expectancy | Use pediatric protocols, minimize dose |
| Pregnant Women | Risk to fetus, special risk in early pregnancy | Use alternative imaging when possible, shield the abdomen |
| Young Adults | Longer life expectancy, risk of cumulative dose | Justify each exam, use the lowest necessary dose |
By understanding these risks and taking precautions, healthcare providers can make sure imaging benefits outweigh risks for all patients.
Patient Advocacy and Radiation Safety
Patient advocacy is key to keeping us safe from radiation in medical imaging. We need to be able to make smart choices about our health care.
Questions to Ask Before Undergoing Imaging Procedures
It’s important to ask the right questions before any imaging test. We should know why it’s needed, what kind of radiation it uses, and the risks it might pose.
- Why is this imaging procedure necessary?
- What are the possible risks and benefits?
- Are there other imaging options that don’t use radiation?
- What dose of radiation will be used?
Tracking Your Personal Medical Imaging History
It’s vital to keep a record of our imaging history. This helps us manage our radiation exposure over time.
| Date | Procedure | Radiation Dose |
| 2022-01-01 | CT Scan | 10 mSv |
| 2023-02-01 | X-Ray | 0.1 mSv |
Patient Rights Regarding Radiation Information
We have the right to know about radiation risks in medical imaging. This includes the dose used and long-term effects.
Key Patient Rights:
- Right to informed consent
- Access to medical records
- Information about radiation risks
The Future of Medical Imaging
Medical imaging is on the verge of a new era. This is thanks to new technologies and a focus on keeping patients safe. These advancements will make diagnosing diseases better and help patients get better faster.
Artificial Intelligence in Radiation Dose Optimization
Artificial intelligence (AI) is changing how we use medical imaging. AI can look at lots of data to find the lowest dose needed for clear images. This means patients get less radiation.
Studies show AI can cut radiation doses by up to 50% in some cases. A top radiologist says AI is a game-changer. It makes diagnoses more accurate and cuts down on radiation.
Emerging Technologies with Improved Safety Profiles
New technologies are also making medical imaging safer and better. For example, compressed sensing and parallel imaging in MRI make scans faster and clearer.
- Photon-counting CT (PCCT) technology
- Advanced ultrasound techniques
- Hybrid imaging modalities
These new tools not only make imaging safer but also help doctors diagnose better. This leads to more accurate treatments for patients.
Personalized Imaging Approaches Based on Individual Risk Factors
The future of medical imaging is about tailoring it to each person. Doctors will use data on each patient to create the best imaging plans. This balances getting good images with keeping radiation low.
This is very important for people who are more sensitive to radiation, like kids and pregnant women. They need special care when they have imaging tests.
As we keep improving medical imaging, the future looks bright. With AI, new technologies, and personalized care, we’re moving towards better patient care. This makes medical imaging safer, more effective, and more focused on the patient.
Conclusion: Making Informed Decisions About Medical Imaging
Medical imaging is complex, and making smart choices is key to safety and care. Knowing about imaging radiation and options helps us reduce risks and get the most benefits.
We’ve looked at how common medical imaging is, the types of radiation procedures, and how tech is cutting down on radiation. We’ve also talked about weighing the good of imaging against the risks and the importance of patient safety.
Patients and doctors need to work together to make good choices about imaging. This means understanding radiation doses, knowing the effects of many scans, and picking safer options like ultrasound and MRI when possible.
By staying informed and teaming up, we can make sure imaging is safe and effective. This focuses on getting accurate diagnoses while keeping patients safe. As medical imaging keeps getting better, making smart choices will always be vital for top-notch healthcare.
FAQ
What is medical imaging, and why is it important in healthcare?
Medical imaging uses technology to see inside the body. It’s key for diagnosing and treating diseases. It helps doctors plan treatments and track how diseases progress.
How prevalent is medical imaging in modern healthcare?
Medical imaging is very common, with 3.6 billion exams done worldwide each year. Radiography, or X-rays, is the most used, with 783 exams per 1,000 people.
What are the different types of medical radiation used in imaging procedures?
We use X-rays, gamma rays, and other ionizing radiation in medical imaging. The type of radiation depends on the procedure and the body part being imaged.
How is radiation exposure measured in medical procedures?
We measure radiation exposure with the dose area product (DAP) and effective dose. These metrics help us understand how much radiation a patient gets.
What are the most common radiation-based imaging procedures?
Common procedures include X-rays, CT scans, and nuclear medicine exams. They help diagnose many conditions, from broken bones to cancer.
How do the radiation doses from different imaging modalities compare?
Radiation doses vary by imaging modality. For example, a chest X-ray has a lower dose than a CT scan. We compare these doses to natural background radiation to understand the risks.
What technological advances are reducing radiation exposure in medical imaging?
New technologies like photon-counting CT and digital radiography are reducing doses. We’re working to use these technologies to improve safety.
Why are pediatric patients at higher risk from imaging radiation?
Kids are more sensitive to radiation because their bodies are developing. We use special protocols and safety measures to protect them.
What are the non-ionizing alternatives to radiation-based imaging?
Alternatives include ultrasound and MRI. We use these when possible, for patients at high risk or when benefits outweigh risks.
What is the ALARA principle in medical imaging?
The ALARA principle aims to minimize radiation exposure while achieving diagnostic goals. We balance the benefits of imaging against the risks of radiation.
How can patients advocate for their radiation safety?
Patients can ask questions before imaging, track their imaging history, and know their rights to radiation information. This helps ensure their safety.
What is the future of medical imaging, and how will it impact radiation safety?
Future advancements include artificial intelligence and safer technologies. We aim to use these to improve safety and effectiveness in medical imaging.
References
- World Health Organization. (2022, November 28). Use of radiation in medicine. https://www.who.int/activities/use-of-radiation-in-medicine



































