What is In Vitro Fertilization (IVF)
In vitro fertilization (IVF) is a fertility treatment where eggs are taken from the ovaries and combined with sperm in a lab. The embryo that forms is placed into the uterus to try for pregnancy. If you’re searching for a clear, patient focused explanation, IVF is the most widely used assisted reproductive technology (ART) to help with many fertility challenges.
Who may benefit from IVF includes patients with blocked fallopian tubes, male factor infertility (such as low sperm count or motility), endometriosis, ovulation disorders, unexplained infertility, or those considering genetic testing of embryos. IVF is also used for fertility preservation (egg or embryo freezing) and is an option for single parents and LGBTQ+ family building.
Success depends on factors such as age, egg and sperm quality, uterine health, and the expertise of IVF clinics and embryology labs. While IVF offers high success potential per cycle, it is not a guarantee; a personalized plan tailored to your diagnosis, timeline, and goals provides the best path forward.
In Vitro Fertilization (IVF) Procedure: Step by Step Process, Reasons, and What to Expect
- Initial consultation and testing: Your fertility specialist reviews your history and orders testing such as ovarian reserve labs (AMH), ultrasound, uterine evaluation, and semen analysis. This allows an individualized protocol and timeline.
- Ovarian stimulation: Daily fertility medications help several follicles grow. You will have multiple monitoring visits, including blood tests and ultrasounds, over about 10 to 14 days. When the follicles are ready, a trigger shot finishes egg maturation.
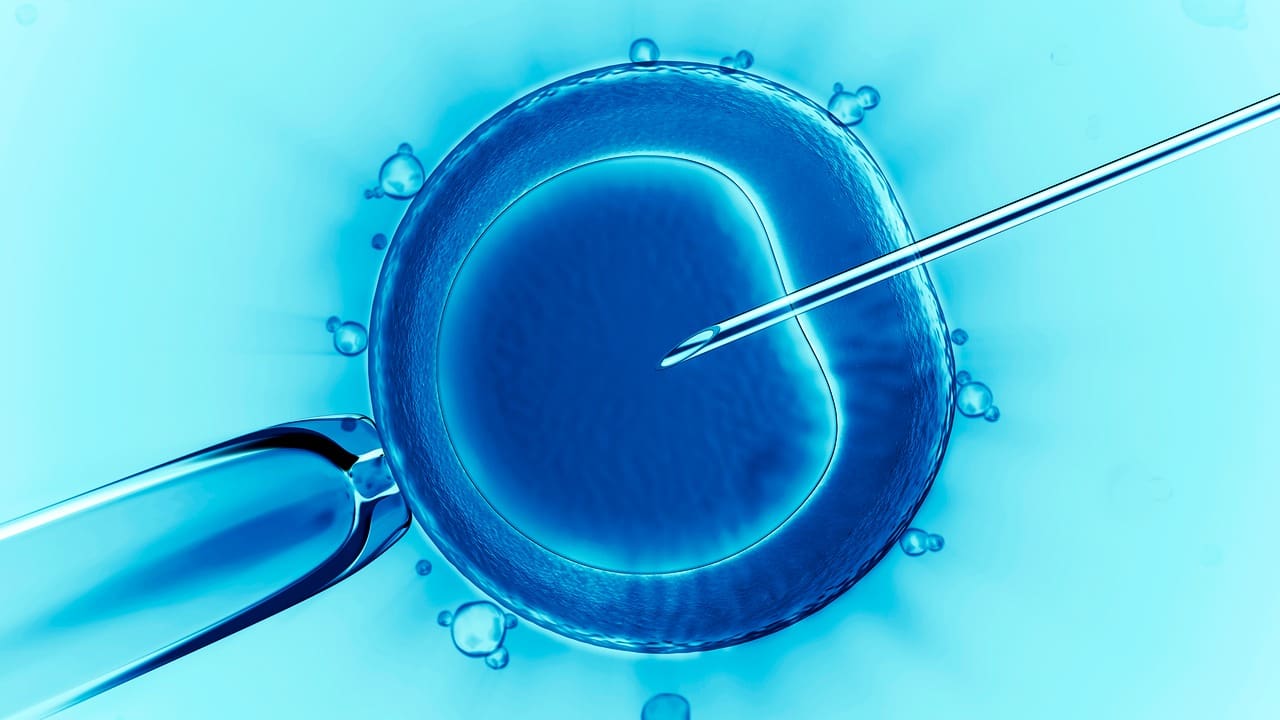
- Egg retrieval: Under light sedation, eggs are collected through a thin needle guided by ultrasound. This is an outpatient procedure and typically takes under 30 minutes. You go home the same day.
- Fertilization and embryo culture: In the lab, eggs are combined with sperm using conventional IVF or ICSI (intracytoplasmic sperm injection) depending on sperm quality. Embryos grow in culture for 3–6 days, often to the blastocyst stage.
- Embryo transfer: A selected embryo is placed into the uterus via a soft catheter (fresh transfer the same cycle or a frozen embryo transfer in a later cycle). The procedure is quick and usually painless.
- Two week wait and pregnancy test: A blood test (hCG) about 9–14 days after transfer confirms whether implantation occurred.
Reasons for IVF include bypassing blocked tubes or severe male factor infertility, maximizing chances when time matters (e.g., advanced maternal age), enabling genetic screening of embryos (PGT), and preserving fertility for future family building.
In Vitro Fertilization (IVF) Cost: How Much IVF Costs, What Affects Price, and Ways to Plan
- Medications and monitoring: Medication doses differ by patient and are a major cost driver.
- Lab procedures: ICSI, assisted hatching, and embryo freezing add fees.
- Genetic testing (PGT): Additional costs for biopsy and analysis.
- Number of cycles and transfers: Fresh versus frozen embryo transfer and future FETs influence the overall budget.
- Donor options: Donor eggs or sperm and gestational carrier services increase the total cost.
- Storage: Ongoing embryo freezing and storage fees.
- Location: Geographic differences in pricing and insurance coverage.
Planning tips: Request an itemized estimate including monitoring, retrieval, anesthesia, lab work, transfer, and pregnancy testing. Ask about medication discount programs, shared risk or refund plans, and financing options. Review your insurance benefits; some plans cover diagnostics or medications even if they don’t cover a full IVF cycle. If you’re comparing regions (for example, in vitro fertilization IVF cost in India), consider travel, time off work, and continuity of care alongside pricing.

IVF Side Effects and Risks: What Patients Should Know Before Treatment
Common, short term effects: Bloating, mood changes, breast tenderness, injection site bruising, temporary fatigue, and minor pelvic pressure.
After egg retrieval: Mild cramping and spotting are typical for 1–3 days; plan light activity and follow discharge instructions.
Less common risks: Ovarian hyperstimulation syndrome (OHSS) is now less frequent with modern protocols and careful monitoring. Symptoms can include significant bloating, rapid weight gain, nausea, or shortness of breath. Contact your clinic if you notice any of these. Egg retrieval also carries small risks of bleeding, infection, or injury, but these are rare with ultrasound guided techniques.
Multiple pregnancy: Transferring more than one embryo increases the risk of twins or higher order multiples; single embryo transfer reduces this risk while maintaining strong success rates in many patients.
Long term considerations: Most data show no overall increase in congenital anomalies after adjusting for parental factors; some risks relate to underlying infertility rather than IVF itself. Emotional and financial stress are real; proactive support and transparent planning help.
Disadvantages of IVF (In Vitro Fertilization): Realistic Expectations and How to Prepare
Patients often search for the disadvantages of IVF in vitro fertilization to understand potential downsides. Key realities include:
- No guaranteed success: Success varies by age and diagnosis; multiple cycles may be needed to reach a live birth.
- Emotional burden: The two week wait and uncertainty can be stressful. Counseling, support groups, and open communication with your care team can help.
- Time commitment: Frequent monitoring visits and self injections require scheduling and support at home and work.
- Cost: IVF can be expensive; add ons like PGT and embryo banking increase total costs. Financial counseling and staged planning can reduce stress.
- Physical discomfort: Injections and retrieval can cause temporary discomfort; most patients recover quickly with standard aftercare.
Preparing with a clear plan, timelines, and expectations helps you navigate treatment with confidence.
What Is the Process of In Vitro Fertilization (IVF)? From Consultation to Pregnancy Test

Before starting: Optimize health with prenatal vitamins (including folic acid), balanced nutrition, moderate exercise, and stopping smoking. Address medical conditions like thyroid disease or diabetes, and complete recommended vaccines if needed.
Baseline visit: On cycle day 1 or 2, your clinic confirms readiness with ultrasound and labs. Medication instructions and timing are reviewed carefully.
Stimulation days: You’ll administer daily injections for 8–14 days and attend monitoring appointments for dose adjustments.
Trigger and retrieval: The trigger shot is precisely timed; egg retrieval occurs about 34–36 hours later under light sedation. Plan a ride home and a restful day.
Lab updates: The clinic updates you on fertilization (the next day) and embryo development on days 3–6.
Transfer or freeze: Based on your uterine lining, hormone levels, and risk of OHSS, your doctor may suggest either a fresh transfer or freezing all embryos for a later frozen embryo transfer.
Luteal support and testing: You’ll take progesterone (and sometimes estrogen) and return for a blood pregnancy test about 9–14 days after transfer.
Special scenarios include donor eggs or sperm for specific indications and PGT for genetic conditions or aneuploidy risk. Your doctor will tailor recommendations to your goals and medical history.
Discharge Instructions for In Vitro Fertilization (IVF): Aftercare and Next Steps

After egg retrieval:
- Expect mild cramping, bloating, and light spotting for 24–72 hours.
- Rest the day of retrieval; avoid driving or alcohol for 24 hours due to sedation.
- Stay hydrated, eat light meals, and use approved pain relief as directed.
- Avoid strenuous exercise, intercourse, swimming, or hot tubs for several days.
- Call your clinic if you develop fever, severe pain, heavy bleeding, rapid weight gain, worsening bloating, or shortness of breath.
After embryo transfer:
- Resume light activities; gentle walking is okay.
- Continue progesterone and other medications as prescribed.
- Avoid high impact exercise, intercourse, and hot tubs/saunas until testing.
- Manage stress during the two week wait with rest, hydration, and support.
- Attend your scheduled blood pregnancy test; early home tests can be misleading.
If positive: Continue medications as advised and schedule an early ultrasound. If negative: Book a follow up to review the cycle, lab findings, and next steps such as protocol adjustments, timing, or considering PGT or donor options.
For more information about our academic and training initiatives, visit Liv Hospital Academy.
Frequently Asked Questions for In Vitro Fertilization (IVF)
Which statement concerning in vitro fertilization (IVF) is true?
Single embryo transfer helps reduce the risk of twins or multiples while maintaining strong success rates when high quality embryos are available.
Which statement about IVF (in vitro fertilization) is correct?
IVF success is not guaranteed in one cycle; age, egg and sperm quality, and uterine health strongly influence outcomes.
What is IVF (in vitro fertilization) compared to other treatments?
IVF typically offers higher per cycle success than intrauterine insemination (IUI), especially for blocked tubes, severe male factor, or when time is a priority.
How much is in vitro fertilization (IVF) with add ons?
The total increases with add ons such as ICSI, PGT, assisted hatching, donor gametes, and embryo storage. Request separate pricing for each component.
How much does in vitro fertilization (IVF) cost?
Costs vary based on medications, lab procedures (ICSI, PGT), the number of transfers, donor options, and storage. Ask for an itemized estimate and review insurance and financing options.
How does in vitro fertilization (IVF) work?
IVF works by stimulating the ovaries to produce multiple eggs, retrieving them, fertilizing them with sperm in a controlled lab, growing embryos, and transferring a selected embryo into the uterus for implantation.
What is the process of in vitro fertilization (IVF)?
The process includes evaluation and testing, ovarian stimulation with medications, egg retrieval, lab fertilization (IVF or ICSI), embryo culture, embryo transfer (fresh or frozen), and a blood pregnancy test.