Last Updated on November 27, 2025 by Bilal Hasdemir

Robotic hysterectomy is a common procedure for many gynecological issues. Many women are concerned about potential changes in bladder function following surgery, including incontinence after hysterectomy.
Understanding incontinence after hysterectomy is important for patients considering robotic hysterectomy. Some women may experience temporary urinary leakage, while others could face longer-term bladder control issues. Knowing the risks helps in planning post-operative care and recovery.
Doctors advise patients to discuss incontinence after hysterectomy with their healthcare provider before surgery. This ensures appropriate preventive measures, exercises, and monitoring are in place to minimize complications.
By being informed about incontinence after hysterectomy, women can better manage expectations, follow recovery guidelines, and seek timely interventions if urinary symptoms occur. Awareness and proactive care are key to reducing the impact of incontinence after hysterectomy.
Key Takeaways
- Robotic hysterectomy can potentially affect bladder function.
- Understanding the risks and complications is essential for patients.
- Patients should discuss their concerns with their healthcare provider.
- Informed decisions about health are key for overall well-being.
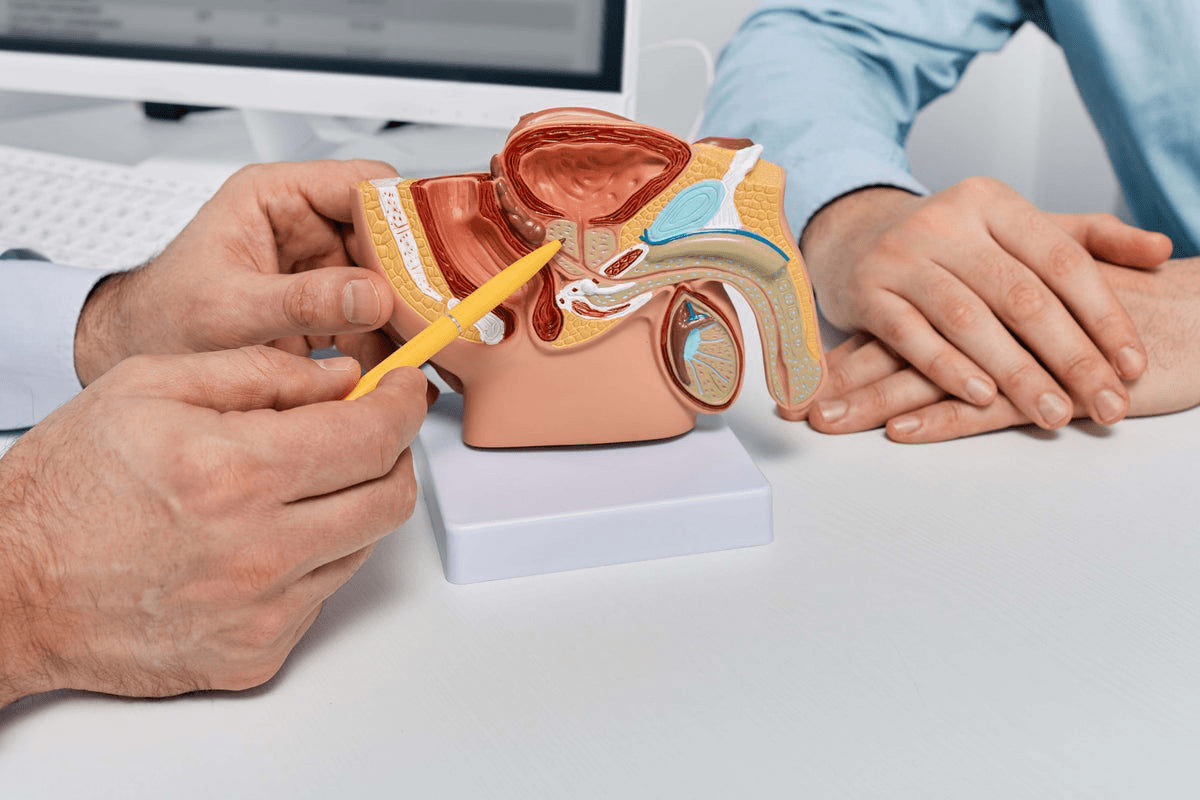
Understanding Bladder Function and Pelvic Anatomy
The bladder works closely with the pelvic anatomy. This complex system can change after surgeries like robotic hysterectomy. Knowing how the bladder and pelvic organs work normally is key.
Normal Bladder Anatomy and Function
The bladder stores urine and is in the pelvis, behind the pubic bone. It’s supported by muscles and ligaments. Normal bladder function means it stores urine until it’s time to empty, then empties completely. The detrusor muscle in the bladder wall helps with this process.
Relationship Between Uterus and Bladder
The bladder and uterus are close together. The bladder is in front of the uterus, separated by tissue. This closeness means surgeries on the uterus can affect the bladder. The supportive structures for the bladder can change after such surgeries.
How Pelvic Organs Support Each Other
Pelvic organs like the bladder, uterus, and rectum have a complex support system. This system is vital for their proper function and position. The pelvic floor muscles are key in supporting these organs.
Weakness or damage to these muscles, which can happen during a hysterectomy, can cause urinary issues.
Key aspects of pelvic organ support include:
- The pelvic floor muscles, which provide the base support.
- Ligaments that connect the organs to the pelvic wall.
- Fascia, a layer of tissue that supports the organs and helps maintain their position.
Understanding these elements is vital for seeing how a robotic hysterectomy might affect bladder function and pelvic health.
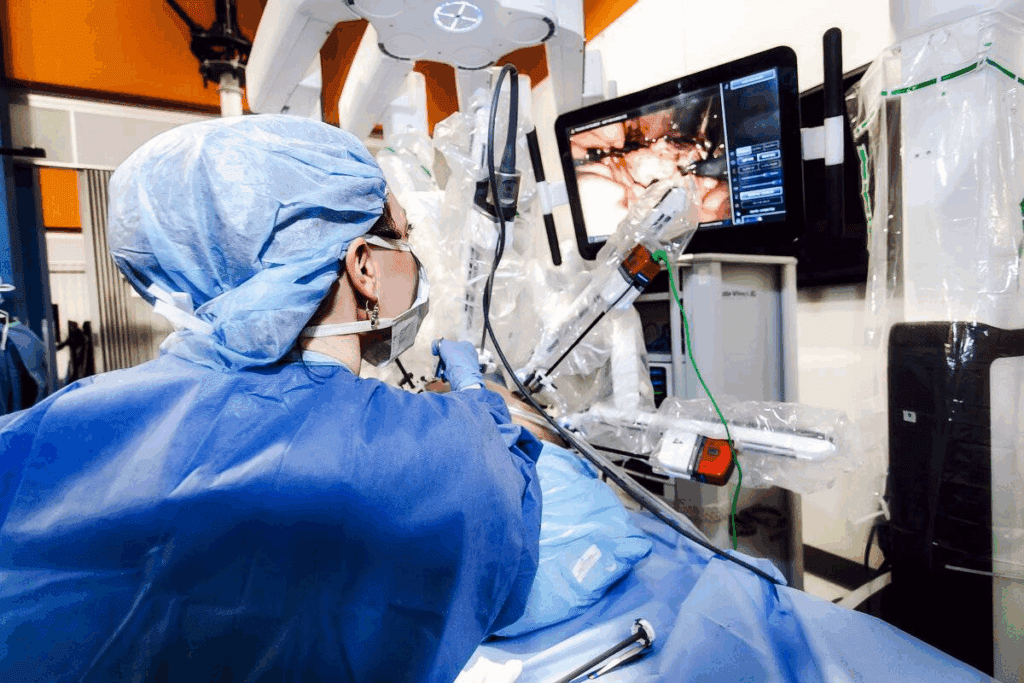
Robotic Hysterectomy: Surgical Approach and Bladder Considerations
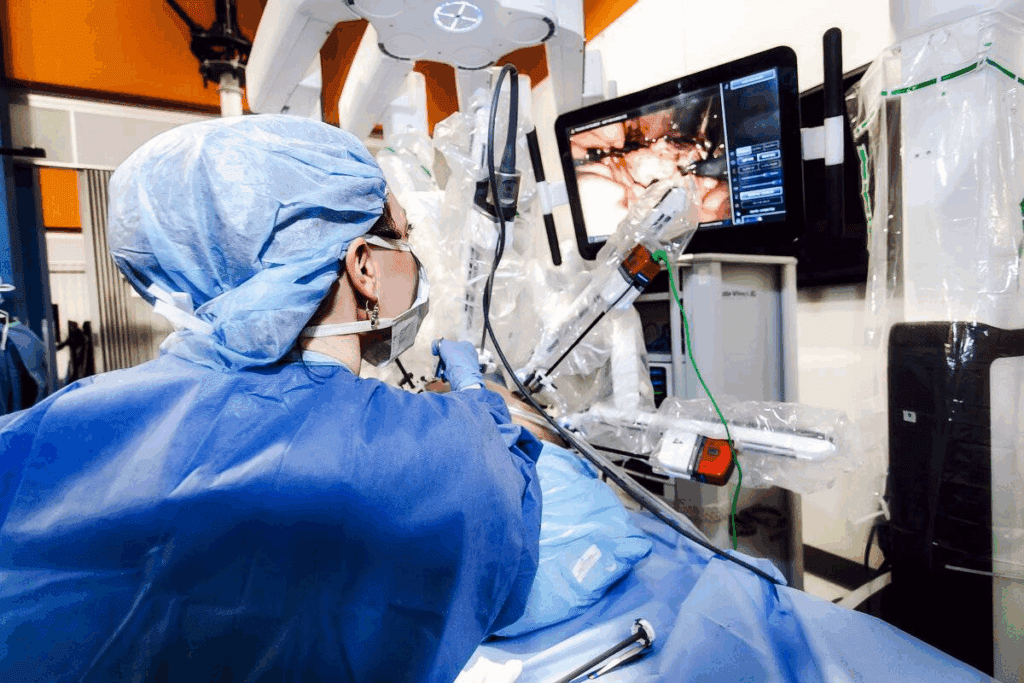
Robotic hysterectomy has changed gynecological surgery for the better. It’s a precise and less invasive method compared to old ways. This new technique uses a robotic system to help surgeons, leading to better results for patients.
How Robotic Surgery Differs from Traditional Approaches
Robotic surgery is different from old methods like open or laparoscopic hysterectomy. The robotic system gives a clear, 3D view of the area being operated on. This makes dissection more precise and reduces blood loss. The robotic tools also move more freely, making complex tasks easier for surgeons.
Studies show robotic hysterectomy leads to shorter hospital stays and less pain after surgery. This is because it’s less invasive, causing less damage to tissues and helping patients heal faster.
Potential Benefits for Bladder Preservation
Robotic hysterectomy offers a significant advantage by helping preserve bladder integrity. The robotic system’s clear view and precision help surgeons avoid harming the bladder’s nerves and tissues. This reduces the risk of bladder injury and long-term urinary problems.
Research shows patients who have robotic hysterectomy often face fewer bladder issues after surgery. This is because the robotic system allows for careful handling of tissues and less dissection near the bladder.
| Benefits | Robotic Hysterectomy | Traditional Hysterectomy |
| Precision | High-definition, 3D visualization | Limited by surgeon’s direct vision |
| Blood Loss | Reduced due to precise dissection | Potential for greater blood loss |
| Recovery Time | Generally quicker | Often longer |
| Bladder Preservation | Enhanced nerve and tissue preservation | More challenging due to less precise techniques |
Surgical Steps That Affect the Bladder
During robotic hysterectomy, several surgical steps can affect the bladder. These include the initial entry into the pelvic cavity, dissection of the uterus from surrounding structures, and the removal of the uterus. The robotic system’s precision helps minimize bladder risk, but surgeons must be careful.
The steps around the uterine arteries and cardinal ligaments are key. Here, the bladder is at risk. The robotic system’s clear view helps surgeons navigate these areas safely.
Immediate Post-Surgical Bladder Changes
Understanding bladder changes after a robotic hysterectomy is key to recovery. After surgery, patients often see changes in how their bladder works.
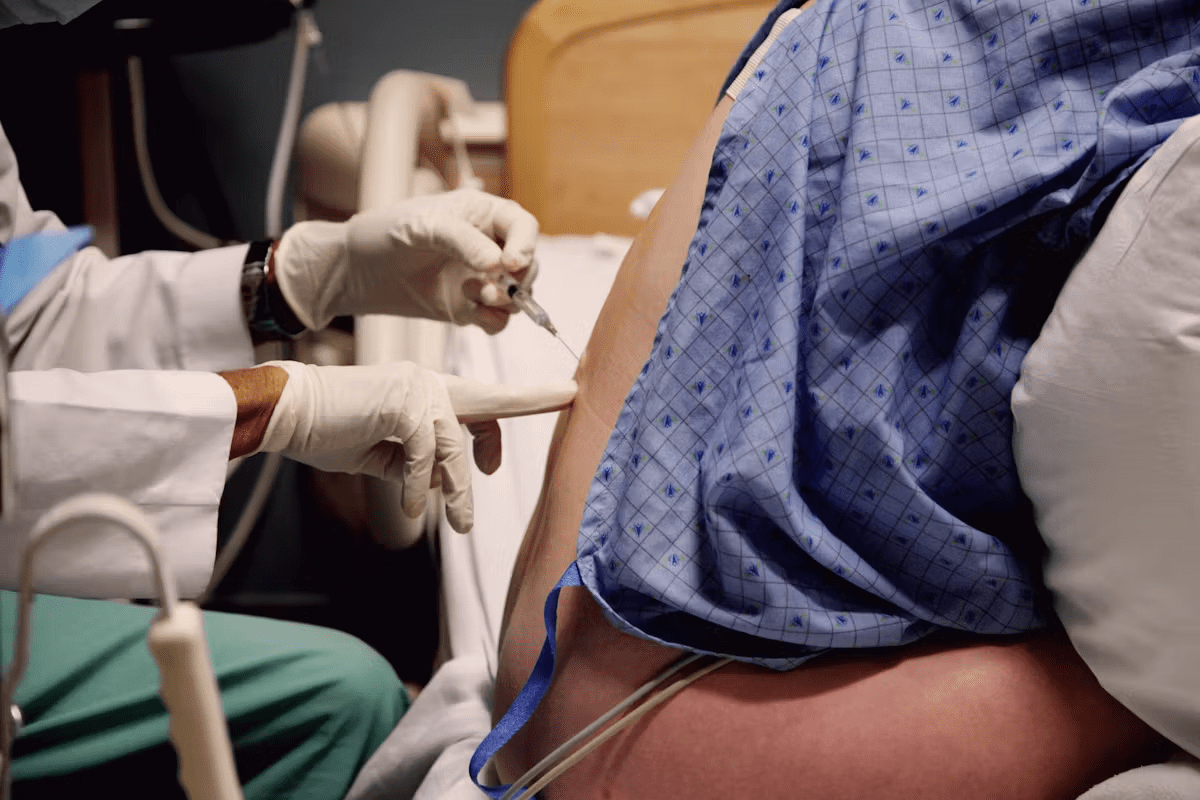
Catheterization After Surgery
A catheter is used to drain urine after a robotic hysterectomy. It helps the bladder rest and heal. The catheter stays in for a few days.
Studies show catheter use lowers the risk of urinary issues and pain right after surgery. Patients usually get the catheter out in 1-3 days, based on how they’re doing.
First Days of Urination After Catheter Removal
Removing the catheter can cause some discomfort or trouble urinating. This is usually short-term and can be helped with drinking water and, if needed, medicine.
It’s important for patients to watch their urine patterns and tell their doctor about any big problems or pain. Common issues include:
- Weak urine flow
- Pain or burning sensation while urinating
- Frequent urination
Normal vs. Concerning Symptoms
Some bladder changes are normal after a hysterectomy, but others need attention. Symptoms to watch for and report include:
| Symptom | Normal | Concerning |
| Urinary Frequency | Mild increase | Severe or persistent |
| Pain While Urinating | Mild discomfort | Severe pain or burning |
| Blood in Urine | Trace amounts | Significant or persistent bleeding |
Knowing the difference between normal and concerning symptoms can greatly affect recovery. If unsure, patients should talk to their doctor.
Recovery Timeline: What to Expect for Your Bladder
After a robotic hysterectomy, many wonder about bladder recovery. The recovery time varies, but knowing the general stages helps. We’ll cover the typical stages of bladder recovery, from right after surgery to long-term healing.
First Week After Surgery
In the first week, the bladder adjusts to the hysterectomy changes. Catheterization is common during this time to help the bladder heal. You might feel some discomfort and have trouble with urination. It’s key to follow your doctor’s post-operative care instructions for healing.
Weeks 2-6 Post-Operation
By 2-6 weeks, bladder function starts to improve. Some may feel more frequent or urgent urination, but these symptoms lessen. Keep following your doctor’s care plan and report any issues.
Long-term Recovery (2-12 Months)
Bladder recovery can take months. Most see big improvements in 2-12 months after surgery. Your health, any complications, and following care instructions affect recovery. Pelvic floor exercises, like Kegels, help during this time.
Knowing the recovery timeline helps patients navigate their journey. It leads to better bladder health.
Temporary Bladder Issues Following Surgery
After a robotic hysterectomy, patients often face temporary bladder problems. These issues come from the surgery’s effect on the pelvic area and bladder. We’ll look at common problems like more frequent urination, bladder spasms, sensitivity, and blood in urine.
Urinary Frequency and Urgency
One common issue is needing to urinate more often. Patients might feel a sudden, strong urge to go.
Key factors contributing to urinary frequency and urgency include:
- Temporary irritation of the bladder during surgery
- Swelling or inflammation in the pelvic area
- Changes in bladder function due to the removal of the uterus
Bladder Spasms and Discomfort
Bladder spasms are another issue. They feel like sharp pains or cramps in the bladder area. These spasms can be uncomfortable and may make you feel like you need to urinate right away.
Management strategies for bladder spasms include:
- Pelvic floor exercises to strengthen the muscles around the bladder
- Medications to reduce spasm frequency and severity
- Avoiding irritants like caffeine and spicy foods
Sensitivity and Burning Sensations
Some patients may feel sensitivity or burning while urinating. This can be due to the catheter used during surgery or temporary changes in the urinary tract.
To alleviate these symptoms, patients can:
- Stay well-hydrated to dilute urine and reduce irritation
- Avoid using harsh soaps or douches that can irritate the genital area
- Use warm compresses to help soothe the area
Blood in Urine: When It’s Normal vs. Concerning
Seeing blood in the urine after surgery can be scary, but it’s not rare. Small amounts of blood can come from the surgery itself.
It’s essential to distinguish between normal and concerning instances of hematuria:
- Normal: Small amounts of blood that clear up within a few days
- Concerning: Heavy bleeding, persistent blood in urine beyond a week, or accompanied by pain and fever
Incontinence After Hysterectomy: Causes and Types
After a hysterectomy, some women may face incontinence, which can really affect their life. This condition can take many forms, each with its own causes. We’ll look at the types of incontinence, what causes them, and how hysterectomy might lead to urinary issues.
Stress Incontinence: Leakage with Physical Activity
Stress incontinence happens when you leak urine during effort, sneezing, or coughing. It’s due to weakened muscles that support the bladder, often from surgery.
Urge Incontinence: Sudden Need to Urinate
Urge incontinence is when you suddenly feel the need to urinate and can’t hold it. It’s often linked to an overactive bladder.
Mixed Incontinence
Mixed incontinence combines stress and urge incontinence symptoms. It’s tough to manage and might need a detailed treatment plan.
Why Hysterectomy Increases Risk of Urinary Problems
Hysterectomy can lead to urinary issues because it changes the pelvic anatomy. It might also harm the nerves around the bladder.
To understand the different incontinence types better, here’s a table:
| Type of Incontinence | Characteristics | Common Causes |
| Stress Incontinence | Leakage with physical activity | Weakened pelvic muscles, surgery |
| Urge Incontinence | Sudden need to urinate | Overactive bladder, neurological issues |
| Mixed Incontinence | Combination of stress and urge symptoms | Multiple factors, including weakened muscles and overactive bladder |
Structural Changes Affecting the Bladder
After a robotic hysterectomy, the bladder and its support can change a lot. These changes might cause problems like a weakened pelvic floor, bladder prolapse, and changes in how the bladder is supported.
Pelvic Floor Weakening
The pelvic floor muscles are key in holding up the bladder and other organs. After a robotic hysterectomy, some women might find these muscles weaker. This can lead to less bladder support and might cause issues like leaking urine or trouble controlling the bladder. Doing Kegel exercises can help make these muscles stronger and improve bladder control.
Bladder Prolapse (Cystocele)
A bladder prolapse happens when the bladder bulges into the vagina because the pelvic floor muscles and ligaments are weak. This can make it hard to pee, cause pain, and make you feel like you need to pee all the time. We will look into the symptoms and how to treat bladder prolapse.
The table below shows the symptoms and effects of bladder prolapse:
| Symptoms | Effects |
| Pelvic pressure or discomfort | Discomfort during daily activities |
| Visible bulge in the vagina | A feeling of something being “dropped” |
| Urinary frequency or urgency | Increased risk of urinary tract infections |
Changes in Bladder Position and Support
Removing the uterus can change where the bladder sits and how it’s supported. The bladder might move or not sit right, leading to pee problems or pain. We will talk about how to handle and treat these changes.
In summary, changes after a robotic hysterectomy can really affect the bladder and pelvic health. Knowing about these changes and their effects is key to managing and treating any problems.
Urinary Tract Infections Following Hysterectomy
After a hysterectomy, the risk of urinary tract infections (UTIs) goes up. It’s important to know why, the signs, and how to treat them. UTIs are a common problem after pelvic surgeries, like a hysterectomy.
Why UTI Risk Increases After Surgery
Several things can make UTIs more likely after a hysterectomy. The surgery can hurt the tissues around the bladder. Also, using catheters can bring bacteria into the urinary tract. Plus, changes in the pelvic area after surgery can mess with urine flow, raising infection risk.
Key Risk Factors:
- Catheter use during and after surgery
- Surgical trauma to the urinary tract
- Changes in pelvic anatomy
- Pre-existing urinary tract conditions
Recognizing UTI Symptoms Post-Hysterectomy
It’s key to spot UTI symptoms early for quick treatment. Common signs include:
- Burning sensation while urinating
- Frequent urination
- Urgent need to urinate
- Cloudy or strong-smelling urine
- Blood in the urine
If you notice any of these signs, reach out to your doctor right away.
Treatment Approaches
UTIs are usually treated with antibiotics. The kind and how long you take them depends on the infection’s severity and your health.
| Treatment Aspect | Description |
| Antibiotic Therapy | Targeted antibiotics to combat the infection |
| Hydration | Increased fluid intake to help flush out bacteria |
| Follow-Up Care | Monitoring to ensure the infection is fully cleared |
Prevention Strategies
Preventing UTIs requires good hygiene, lifestyle changes, and sometimes, antibiotics.
Prevention Tips:
- Drink plenty of water to stay hydrated
- Urinate when you feel the need, and avoid holding urine
- Practice good hygiene, wiping from front to back
- Avoid irritating feminine products
Knowing the risks, spotting symptoms early, and using prevention tips can help lower UTI chances after a hysterectomy.
Serious Bladder Complications to Be Aware Of
Serious bladder problems can happen after robotic hysterectomy. It’s key to know about them. This knowledge helps patients prepare for their recovery.
Bladder Injury During Surgery
Bladder injury during surgery is a serious issue. The risk is low, but it’s something patients should know. Promptly fixing such injuries is vital to avoid long-term problems.
Fistula Formation
Fistula formation is another complication. A fistula is an abnormal connection between the bladder and another organ or the skin. Fistulas can cause significant urinary incontinence and may need more surgery to fix. It’s important to watch for signs of fistula after surgery.
Chronic Retention Issues
Chronic retention issues can occur after robotic hysterectomy. This means the bladder can’t empty fully. It can cause urinary tract infections and other problems. Managing chronic retention often needs medical and lifestyle changes.
When to Seek Immediate Medical Attention
Knowing when to seek urgent care is vital. Look out for severe abdominal pain, heavy vaginal bleeding, fever, and trouble urinating. If you have these symptoms, call your healthcare provider right away.
Knowing about these serious bladder issues helps patients take care of themselves during recovery. We suggest talking to your healthcare provider about any worries to get the best results.
Managing Urinary Symptoms at Home
Managing urinary symptoms after a hysterectomy can make recovery easier. Dealing with these issues can be tough, but there are ways to help at home.
Hydration Strategies
Staying hydrated is key, but it can be hard with urinary symptoms. Drinking the right amount of fluid helps prevent infections and reduces urine concentration. This can lessen bladder irritation.
- Drink at least 8-10 glasses of fluid per day, unless your doctor advises differently.
- Avoid caffeinated and carbonated drinks that can bother the bladder.
- Watch your urine color; it should be pale yellow, showing you’re drinking enough.
Bladder Training Techniques
Bladder training can improve bladder control and reduce symptoms. By slowly increasing the time between bathroom visits, you can train your bladder to hold more urine.
- Begin by keeping a bladder diary to track your urination.
- Slowly increase the time between bathroom visits by 15 minutes every few days.
- Try deep breathing exercises to manage urgency.
Lifestyle Modifications
Changing your lifestyle can also help manage urinary symptoms. Maintaining a healthy weight reduces bladder pressure. Avoiding heavy lifting helps prevent strain on the pelvic floor muscles.
- Do gentle exercises like walking or pelvic floor exercises (Kegels) as your doctor suggests.
- Stop smoking to avoid chronic coughing, which strains the pelvic floor.
- Use absorbent products if you leak to protect your clothes and feel more confident.
By adding these strategies to your daily life, you can manage urinary symptoms at home. This will improve your recovery after a robotic hysterectomy.
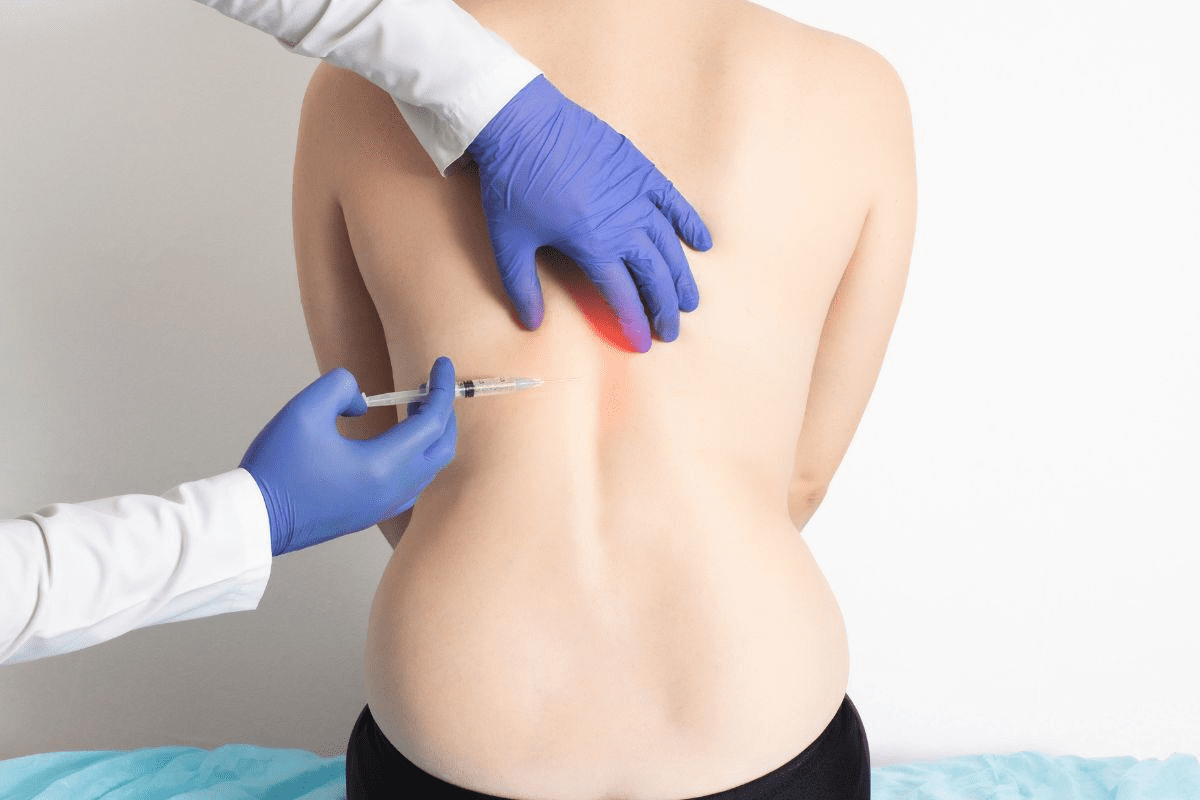
Pelvic Floor Rehabilitation for Bladder Control
Effective pelvic floor rehabilitation can greatly improve bladder control and life quality after a hysterectomy. This approach includes various methods to strengthen muscles that support bladder function.
Kegel Exercises: Proper Technique and Frequency
Kegel exercises are key in pelvic floor rehabilitation. They involve contracting and releasing muscles to stop urine flow. To do Kegel exercises right, find the right muscles by stopping urine mid-stream.
Once you find them, squeeze for 5-10 seconds, then relax for the same time. Do this 10-15 times, three times a day.
Physical Therapy Options
Physical therapy is essential in pelvic floor rehabilitation. A specialized therapist can create exercises tailored to your needs. They may use manual therapy, stretching, and strengthening exercises.
Biofeedback and Electrical Stimulation
Biofeedback and electrical stimulation are advanced methods used in pelvic floor rehab. Biofeedback uses sensors to show muscle activity in real-time. This helps patients better control their pelvic floor muscles.
Electrical stimulation uses gentle currents to strengthen muscles. It helps improve function and strength.
Vaginal Weights and Devices
Vaginal weights and devices are tools used in pelvic floor rehab. They provide resistance to strengthen muscles. They’re helpful for women who find it hard to contract their pelvic floor muscles.
Using these techniques in a rehab program can greatly enhance bladder control and pelvic health after a robotic hysterectomy. It’s vital to work with healthcare professionals to create a personalized plan.
Medical and Surgical Interventions for Persistent Problems
If bladder control issues last after a robotic hysterectomy, there are many options. Finding the right treatment can be tough. It’s important to try different approaches to find relief.
Medications for Bladder Control
Medicines can help manage bladder problems for some women. These include:
- Anticholinergics: to reduce bladder spasms and urgency
- Beta-3 adrenergic agonists: to relax the bladder muscle and increase capacity
Talking to your doctor about these medicines is key. They can explain the good and bad sides.
Bladder Sling Procedures
Bladder sling procedures are a surgical choice for stress urinary incontinence. They place a sling under the urethra to improve control. Your doctor will choose the best sling for you.
Combined Hysterectomy and Bladder Support Surgery
Some women might need surgery that fixes both the hysterectomy and bladder support. This is good for those with weak pelvic floors or prolapse.
Botox and Other Minimally Invasive Options
Botox injections can help with urgency and frequency. Other small treatments might also work for you. These are considered when other methods don’t help enough.
Talking to a healthcare professional is a good first step. They can help find the best treatment for you.
Conclusion
It’s important for women to understand how robotic hysterectomy affects bladder health. We’ve talked about how the uterus and bladder are connected. Changes during and after surgery can impact bladder function.
Women might face issues like needing to urinate often, leaking urine, or feeling sensitive. It’s vital to know how to handle these problems for a smooth recovery. Pelvic floor exercises, changing your lifestyle, and sometimes medical help can improve bladder health after surgery.
Being informed and proactive helps women deal with robotic hysterectomy’s challenges. We stress the need for full care and support during recovery. This ensures the best results for bladder health.
FAQ
What are the common bladder changes after a robotic hysterectomy?
After a robotic hysterectomy, you might notice changes in your bladder. These can include needing to urinate more often, feeling a strong urge to go, leaking urine, and experiencing bladder spasms. These symptoms are usually temporary but can last longer for some people.
How long does it take for bladder function to recover after robotic hysterectomy?
The time it takes for your bladder to recover can vary. Most people see big improvements in 2-6 weeks. But, it can take up to 12 months for full recovery in some cases.
What is the risk of urinary incontinence after hysterectomy?
Hysterectomy can raise your risk of urinary incontinence. This is because the surgery changes the pelvic area and its support structures. The risk depends on your individual situation and the type of hysterectomy you had.
How can I manage urinary symptoms at home after robotic hysterectomy?
To manage urinary symptoms at home, try drinking lots of water and avoiding things that can irritate your bladder. Also, do pelvic floor exercises regularly. These steps can help a lot.
What are the signs of a urinary tract infection (UTI) after hysterectomy?
Signs of a UTI after hysterectomy include pain when you pee, needing to pee a lot, urine that looks cloudy or smells bad, and pain in your pelvis. If you notice these symptoms, you should see a doctor right away.
Can pelvic floor rehabilitation help with bladder control after hysterectomy?
Yes, pelvic floor rehabilitation can help a lot with bladder control after hysterectomy. This includes Kegel exercises, physical therapy, and biofeedback. These methods can make a big difference.
What are the treatment options for persistent bladder problems after hysterectomy?
If you have ongoing bladder problems after hysterectomy, there are treatments available. These include medicines for bladder control, bladder sling procedures, and even Botox injections. Your doctor can help you find the best option.
Is it normal to experience bladder spasms after robotic hysterectomy?
Bladder spasms are a common issue after robotic hysterectomy. They can be uncomfortable but usually go away on their own in a few weeks.
How can I prevent UTIs after hysterectomy?
To prevent UTIs, stay hydrated, practice good hygiene, pee when you need to, and avoid things that can irritate your bladder. Your doctor might also have specific advice for you.
What are the serious bladder complications that can occur after hysterectomy?
Serious bladder complications after hysterectomy include bladder injury during surgery, fistula formation, and chronic retention issues. It’s important to know about these risks and seek medical help if you have severe symptoms.
Can I stillexperience urinary leakage after having a bladder sling procedure?
Bladder sling procedures can help with stress incontinence, but some people might experience occasional leakage. The success rate varies, and you might need more treatments in some cases.
Reference:
Cambridge University Hospitals: Bladder care and management
https://www.cuh.nhs.uk/patient-information/bladder-care-and-management
National Institutes of Health (NCBI) on urologic surgery outcomes