Pulmonary hypertension is a serious heart and lung issue. It means elevated pressure in the lung’s blood vessels. Sadly, many cases go unnoticed until it’s too late.
At Liv Hospital, we understand the importance of early detection. We use a patient-focused approach. This combines top medical standards with caring for you. We help spot the signs of pulmonary hypertension and high blood pressure early.
It’s key to know how pulmonary hypertension and high blood pressure are linked. This knowledge helps manage symptoms and improve health. We aim to provide top-notch healthcare and support for patients from around the world.
Listing five crucial warning signs of severe heart and lung conditions, like pulmonary hypertension.
Key Takeaways
- Understanding pulmonary hypertension is key for early detection.
- Pulmonary hypertension is high blood pressure in the lung arteries.
- Symptoms include shortness of breath, dizziness, and fatigue.
- Early diagnosis and treatment can greatly improve outcomes.
- A patient-centered approach is vital for managing the condition.
What You Need to Know About Pulmonary Hypertension

We will dive into the key points about pulmonary hypertension. This condition is a high blood pressure issue that affects the lungs and the heart’s right side. It’s called pulmonary arterial hypertension (PAH) when the lung’s blood vessels get narrowed or blocked.
Defining Pulmonary Hypertension of the Lungs
Pulmonary arterial hypertension is a disease that blocks blood flow in the lungs. This leads to heart failure and can be deadly if not treated. It’s caused by elevated pulmonary artery pressure due to genetics, environment, or other health issues.
2024-2025 Epidemiological Data
Recent data from 2024-2025 shows pulmonary hypertension is a big health problem worldwide. The condition’s prevalence varies among different groups. The table below highlights some key findings.
Population | Prevalence of PH |
General Population | 0.5-1% |
Patients with Heart Disease | 5-10% |
Patients with Lung Disease | 10-20% |
Why This Condition Remains Underrecognized
Pulmonary hypertension is often missed because of its vague symptoms. It’s also because not everyone knows about it, and some places don’t have the right tools to diagnose it. Early detection is key for better treatment and outcomes.
It’s vital for both healthcare professionals and patients to understand pulmonary hypertension. Recognizing its signs early can lead to better care and a better life for those affected.
The Critical Difference Between Pulmonary and Systemic Hypertension

It’s important to know the difference between pulmonary and systemic hypertension. Both involve high blood pressure, but they affect different parts of the body. This difference is key for the right treatment.
Understanding Elevated Pulmonary Artery Pressure
Pulmonary hypertension means high blood pressure in the arteries leading to the lungs. This happens when the lung arteries get narrow and stiff. It makes it hard for blood to flow, causing symptoms like shortness of breath and heart palpitations.
A mean pulmonary artery pressure above 20 mm Hg is considered high. This can lead to breathlessness. We’ll see how it’s different from systemic hypertension and what happens when they both occur.
How Systemic High Blood Pressure Differs
Systemic hypertension is high blood pressure in the arteries outside the lungs. It’s a big risk for heart disease and stroke. It often doesn’t show symptoms, making it a silent killer.
Managing systemic hypertension is well-known, with lifestyle changes and medicines. But pulmonary hypertension needs a different approach. It focuses on improving lung blood flow and easing right heart strain.
When Both Conditions Coexist
Some patients have both pulmonary and systemic hypertension. This makes diagnosis and treatment harder. Systemic hypertension can make pulmonary hypertension symptoms worse, and vice versa.
When treating both, we need a detailed plan. We must tackle both high blood pressure and lung artery pressure. Understanding these conditions and their interaction helps us care for our patients better.
The WHO Classification System for Pulmonary Hypertension
The World Health Organization (WHO) has created a system to classify pulmonary hypertension. It groups the condition based on causes and how it affects the heart. This system helps doctors understand and treat pulmonary hypertension better.
Group 1: Pulmonary Arterial Hypertension (PAH)
Pulmonary Arterial Hypertension (PAH) means high blood pressure in the lungs’ arteries. It’s a serious condition that can cause heart failure. PAH can happen on its own or with other diseases like HIV or certain medicines.
Key characteristics of PAH include:
- Elevated pulmonary artery pressure
- Normal or low pulmonary capillary wedge pressure
- Absence of other causes of pulmonary hypertension
Group 2: PH Due to Left Heart Disease
Pulmonary hypertension from left heart disease happens when the left heart has problems. This can be due to weak heart muscles or faulty valves. It’s important to treat these heart issues to manage pulmonary hypertension.
Group 3: PH Due to Lung Diseases and Hypoxia
Lung diseases like COPD or interstitial lung disease can cause pulmonary hypertension. This is because of long-term lack of oxygen and lung damage. Treating the lung disease is key to managing pulmonary hypertension.
Group 4: Chronic Thromboembolic PH (CTEPH)
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is caused by blood clots in the lungs’ arteries. It’s a treatable form of pulmonary hypertension if caught early. Surgery is often used to treat it.
Knowing the WHO classification system is vital for doctors to diagnose and treat pulmonary hypertension. By grouping it into specific categories, doctors can create better treatment plans. This helps improve patient care and outcomes.
Sign #1: Progressive Shortness of Breath During Activity
Shortness of breath during activity is a key sign of pulmonary hypertension. It often starts during exercise and can get worse over time. Even sitting can become hard to breathe.
This symptom makes daily life tough. It’s important to know why it happens and how it relates to high blood pressure. This knowledge helps in early detection and treatment.
Why Breathlessness Occurs in Pulmonary Hypertension
Pulmonary hypertension makes the pulmonary arteries narrow and stiff. This raises the pressure against the heart’s right side. The heart then works harder, leading to right heart failure and trouble breathing.
Breathlessness in pulmonary hypertension comes from several factors. It’s not just the high pressure in the arteries. It also involves gas exchange issues and the body’s efforts to compensate.
High Blood Pressure and Breathlessness Connection
High blood pressure and pulmonary hypertension are different but can both cause breathing problems. High blood pressure makes the left side of the heart work harder. This can lead to left ventricular hypertrophy and heart failure, causing breathlessness.
The link between high blood pressure and breathing issues is complex. It affects the heart directly and the lungs and circulation indirectly.
When Everyday Activities Become Challenging
As pulmonary hypertension gets worse, simple tasks like walking or climbing stairs become hard. This not only affects physical health but also has emotional and social impacts. People may feel isolated because they can’t do as much.
Recognizing these symptoms early and understanding their link to pulmonary hypertension is key. It helps in getting medical help sooner, which can improve outcomes and quality of life.
Sign #2: Persistent Fatigue and Weakness
Persistent fatigue and weakness are key signs that can really affect someone’s life. These symptoms are not just about feeling tired. They are complex and touch every part of a person’s life.
The Physiological Basis of Fatigue in PHTN
Fatigue in pulmonary hypertension (PHTN) happens because the heart can’t pump enough blood. This means less oxygen gets to the body’s cells. As a result, increased fatigue and weakness occur because the body’s cells can’t work right.
The changes in PHTN, like elevated pulmonary artery pressure, make the heart work even harder. This leads to feeling very tired.
Impact on Daily Functioning
Fatigue greatly affects daily life. Even simple tasks like grocery shopping or cooking can be hard. It limits a person’s ability to do things they love, affecting their well-being and mental health.
- Reduced productivity at work or home
- Difficulty maintaining social relationships
- Increased reliance on others for daily tasks
When Fatigue Signals Worsening Disease
Fatigue is common in PHTN, but getting worse can mean the disease is getting worse. It’s important for patients to watch their energy levels and tell their doctor if they notice big changes. Early detection of worsening symptoms can help improve outcomes.
Understanding how fatigue relates to PHTN helps patients and doctors manage symptoms better. This improves quality of life.
Sign #3: Heart Palpitations and Chest Discomfort
Heart palpitations can be a concerning symptom for individuals with pulmonary hypertension, indicating heart strain. A fast pulse or pounding heartbeat can be alarming and disrupt daily life. We will explore the causes of heart palpitations in pulmonary hypertension, their relationship with high blood pressure, and the types of chest pain associated with this condition.
Understanding Lung Palpitations in Pulmonary Hypertension
Lung palpitations, more accurately described as heart palpitations, occur when there is an abnormal awareness of the heartbeat. In pulmonary hypertension, this can be due to the increased strain on the right side of the heart as it works against the elevated pulmonary artery pressure. The right ventricle hypertrophies (thickens) in response to the increased workload, which can lead to palpitations.
As Dr. Experts note, “The sensation of heart palpitations can be unsettling, but it is a critical symptom that requires evaluation.”
High Blood Pressure and Heart Palpitations
High blood pressure, or systemic hypertension, can coexist with pulmonary hypertension and further complicate the clinical picture. When both conditions are present, the heart faces a double burden: pumping blood through the high resistance in the systemic circulation and against the elevated pulmonary artery pressure. This can exacerbate symptoms like heart palpitations.
“Hypertension is a significant risk factor for cardiovascular disease, and its presence alongside pulmonary hypertension necessitates careful management.”
Types of Chest Pain Associated with PHT Heart
Chest pain or discomfort in pulmonary hypertension can manifest in various forms. It may be related to the strain on the heart, ischemia (reduced blood flow to the heart muscle), or other factors. Common descriptions include:
- A tight or heavy sensation in the chest
- Sharp, stabbing pains that may worsen with deep breathing
- A feeling of pressure or discomfort that may radiate to the arms, back, or jaw
Understanding these symptoms is key for diagnosing and managing pulmonary hypertension effectively. We will continue to explore the remaining signs and their implications in subsequent sections.
Sign #4: Swelling in the Ankles, Legs, and Abdomen
Swelling in the ankles, legs, and abdomen is a warning sign of pulmonary hypertension. It happens because of fluid buildup, a common problem with this condition. We will look into why this swelling occurs, how it gets worse, and how it’s different from other swelling causes.
The Mechanism of Edema in Pulmonary Hypertension
Swelling in pulmonary hypertension is mainly because the heart can’t pump blood well. This makes fluid build up in the body. The right side of the heart gets tired, causing fluid to leak into tissues. This leads to swelling, mostly in the legs and belly.
Progressive Nature of Fluid Retention
Fluid buildup in pulmonary hypertension gets worse over time if not treated. As the heart struggles to pump blood, more fluid builds up. It’s important to watch and manage fluid retention to slow down the disease and reduce swelling.
Differentiating from Other Causes of Swelling
Swelling in the ankles, legs, and abdomen can also mean other health issues like heart failure or kidney disease. To figure out the cause, doctors need to look at your medical history, do a physical check, and run tests. Knowing the real cause is key to the right treatment.
Sign #5: Dizziness, Fainting, and Bluish Lips or Skin
As pulmonary hypertension gets worse, people might feel dizzy, faint, or notice their skin turning bluish. These signs show the disease is serious and need quick doctor visits.
Syncope as a Warning Sign in PA HTN
Syncope, or fainting, is a big warning sign for those with pulmonary arterial hypertension (PAH). It happens when the brain doesn’t get enough blood flow. This is often because the heart can’t pump enough blood.
Fainting spells are scary for patients and their families. It’s important to know that fainting in PAH patients is more than just a simple faint. It can mean the disease is getting worse.
Oxygen Deprivation and Skin Color Changes
Oxygen problems in pulmonary hypertension can make skin color change, often to a bluish tint called cyanosis. This happens when there’s not enough oxygen in the blood. The skin might look blue or gray, depending on the person’s skin tone.
In severe cases, cyanosis can show up in lips, fingers, or toes. This is a clear sign that the body is struggling to get enough oxygen.
The Neurological Impact of Reduced Cardiac Output
When the heart pumps less in pulmonary hypertension, it can affect the brain. Dizziness and fainting are direct results of the brain not getting enough blood. Patients might also have other brain symptoms because of less oxygen to important organs.
Healthcare providers need to watch these signs closely. They show the disease is getting worse. Understanding how less blood flow affects the brain helps us manage the disease better and improve patient results.
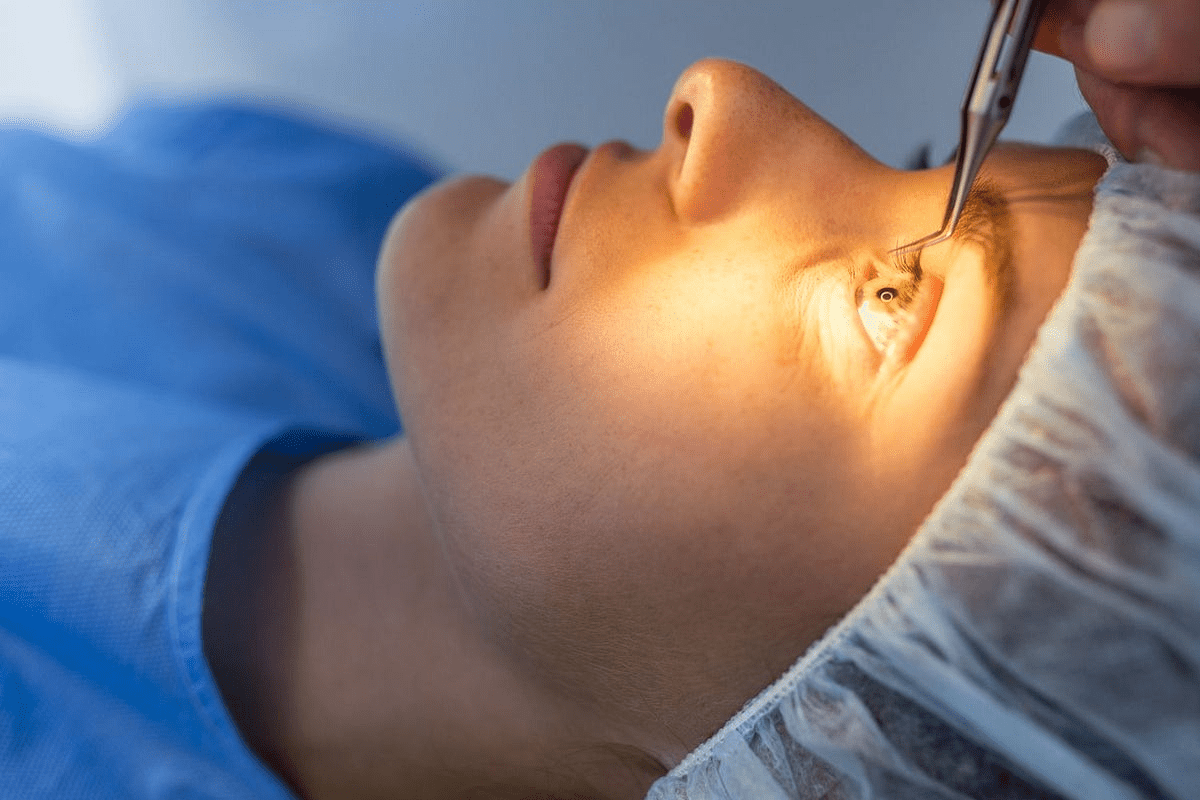
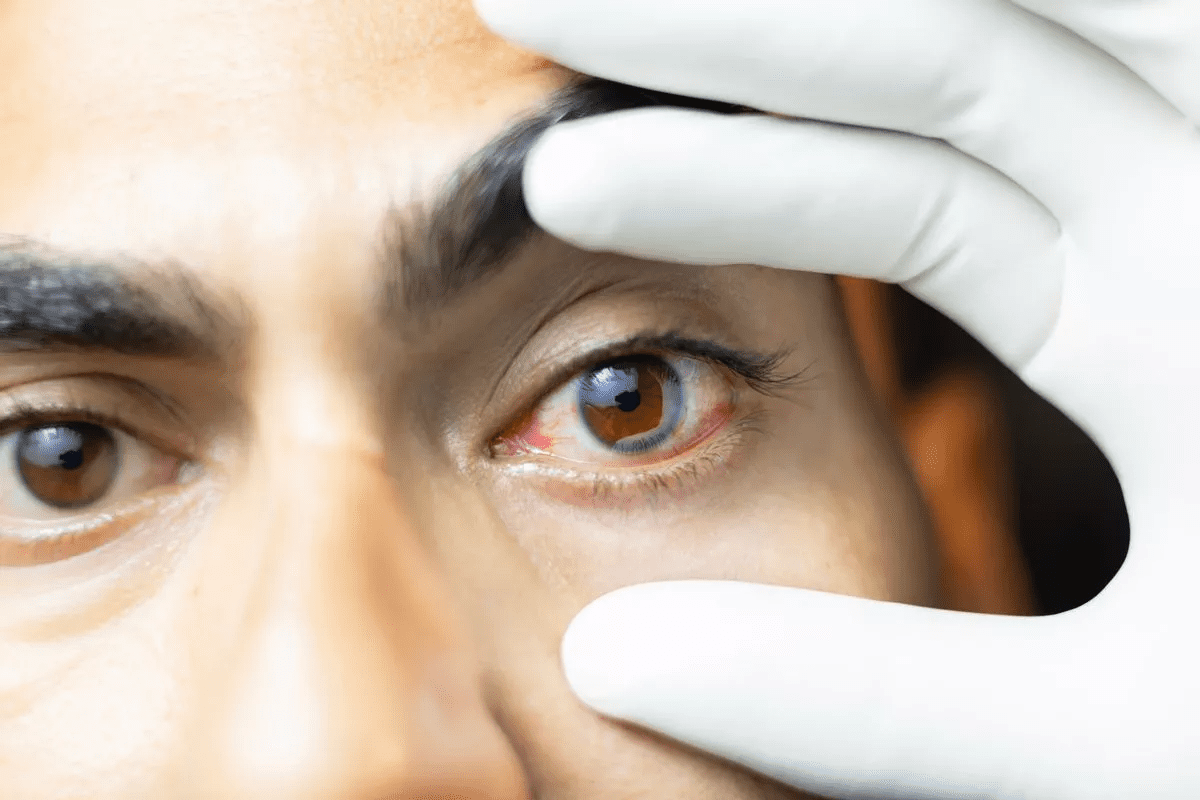
Diagnosis and Management of Heart and Lung Conditions
Diagnosing pulmonary hypertension needs a detailed approach with various tests. Accurate diagnosis is key for effective management and better patient outcomes.
Essential Diagnostic Tests
Several tests are vital for diagnosing pulmonary hypertension. These include:
- Echocardiogram to assess heart function and structure
- Right heart catheterization to measure the pressure in the pulmonary arteries
- VQ scan to evaluate lung function and detect any blockages
- Pulmonary function test to assess lung capacity and function
- Blood tests to check for biomarkers and other related conditions
Right heart catheterization is the gold standard for diagnosing pulmonary hypertension. It directly measures the pressure in the pulmonary arteries.
Treatment Approaches for Different PH Groups
Treatment for pulmonary hypertension varies based on the condition’s classification. The World Health Organization (WHO) classification system guides treatment approaches:
- Group 1: Pulmonary Arterial Hypertension (PAH) – Treatment includes vasodilators, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors.
- Group 2: PH Due to Left Heart Disease – Management focuses on treating the underlying left heart disease.
- Group 3: PH Due to Lung Diseases and Hypoxia – Treatment involves addressing the underlying lung condition and oxygen therapy.
- Group 4: Chronic Thromboembolic PH (CTEPH) – Treatment may include anticoagulation and surgical intervention such as pulmonary endarterectomy.
Managing Coexisting Hypertension and Pulmonary Hypertension
Managing patients with both hypertension and pulmonary hypertension requires a detailed strategy. It’s essential to monitor both conditions closely and adjust treatments as needed to prevent complications.
“The management of pulmonary hypertension in patients with coexisting systemic hypertension necessitates a careful balance between treating both conditions effectively.” – Expert Opinion
Latest Therapeutic Advances for Elevated Lung Pressure
Recent advances in therapeutic options have improved pulmonary hypertension management. New drugs and treatment protocols target different disease pathways.
Emerging therapies include gene therapy, new pharmacological agents, and innovative delivery methods. These offer hope for better outcomes for patients with pulmonary hypertension.
Conclusion: Living with Pulmonary Hypertension
Living with pulmonary hypertension means you need a full plan to manage symptoms and improve your life. We know managing PH well is key to better health outcomes. Thanks to new treatments, there’s hope for patients to handle their symptoms and live longer.
At our institution, we’re dedicated to top-notch healthcare for international patients. Our team works closely with patients to create care plans tailored just for them. This ensures they get the best treatment. We also keep up with the latest in PH treatment to help patients manage their condition.
Managing PH well means using medicine, making lifestyle changes, and getting ongoing support. We focus on teaching patients and empowering them to be part of their care. Together, we can make a big difference in the lives of those with pulmonary hypertension.
FAQ
What is pulmonary hypertension?
Pulmonary hypertension is a serious condition. It happens when blood pressure in the lungs’ arteries gets too high. This makes it hard for blood to flow and forces the heart to work too hard.
How is pulmonary hypertension classified?
The World Health Organization groups pulmonary hypertension into five categories. These categories are based on how the condition affects the body.
What is the difference between pulmonary hypertension and systemic hypertension?
Pulmonary hypertension is high blood pressure in the lungs’ arteries. Systemic hypertension is high blood pressure in the whole body. They can both happen at the same time and affect health differently.
What are the key signs of pulmonary hypertension?
Signs include getting breathless easily, feeling very tired, and having heart palpitations. You might also notice swelling in your legs and feel dizzy or faint. Bluish lips or skin are also warning signs.
How is pulmonary hypertension diagnosed?
Doctors use tests to check the blood pressure in the lungs’ arteries. They look for a pressure above 20 mm Hg to diagnose it.
Can pulmonary hypertension cause high blood pressure?
Pulmonary hypertension is about high blood pressure in the lungs. It can happen with high blood pressure in the body, but they are different conditions.
What is the impact of pulmonary hypertension on daily life?
It can make everyday life hard. Symptoms like breathlessness, tiredness, and swelling can really affect your quality of life.
How is pulmonary hypertension managed?
Management depends on the type of pulmonary hypertension. It includes treating other conditions like high blood pressure and using new treatments.
What is the significance of the WHO classification system for pulmonary hypertension?
The WHO system is key for choosing the right treatment. It groups pulmonary hypertension into different types to guide treatment.
How does elevated pulmonary artery pressure manifest?
High blood pressure in the lungs can cause breathlessness. It’s a sign of elevated pulmonary artery pressure.
What are the latest therapeutic advances for elevated lung pressure?
New treatments aim to lower blood pressure in the lungs. They also help manage symptoms of pulmonary hypertension.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5329977/