Getting a positive ANCA test result can be scary. But knowing what it means is key to getting better. At Liv Hospital, we take anti neutrophil cytoplasmic antibodies test results very seriously. They are linked to autoimmune diseases like granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA).cytoplasmic ancaTop 5 Worst Autoimmune Diseases: Fatal Risks, Symptoms & Deadliest Types
A positive ANCA test shows you have certain antibodies. These can help doctors diagnose and treat autoimmune vasculitis. Our team is here to give you the care and support you need.

To understand a positive ANCA test, knowing what ANCAs are and why doctors test for them is key. ANCA blood testing finds anti-neutrophil cytoplasmic antibodies. These are linked to certain autoimmune diseases.
Anti-neutrophil cytoplasmic antibodies (ANCAs) target proteins in neutrophils, a white blood cell type. They are linked to autoimmune vasculitis, where the immune system attacks blood vessels. There are two main types: cytoplasmic ANCA (c-ANCA) and perinuclear ANCA (p-ANCA). Each is tied to different diseases and symptoms.
Doctors test for ANCAs to diagnose and track autoimmune vasculitis. This includes diseases like Granulomatosis with Polyangiitis (GPA) and Microscopic Polyangiitis (MPA). The test shows ANCA levels, helps decide treatment, and checks disease progress.
Knowing about c-ANCA is key for diagnosing and treating diseases linked to anti-neutrophil cytoplasmic antibodies. Cytoplasmic ANCA, or c-ANCA, targets the inside of neutrophils, a type of white blood cell. It’s a big deal in diagnosing certain autoimmune diseases.
c-ANCA attacks Proteinase 3 (PR3), an enzyme in neutrophils. The fight between c-ANCA and PR3 plays a big role in some vasculitides, like Granulomatosis with Polyangiitis (GPA). So, testing for c-ANCA is a big help in diagnosing GPA.
There are two main ANCA types: c-ANCA and perinuclear ANCA (p-ANCA). c-ANCA goes after PR3, while p-ANCA targets myeloperoxidase (MPO). Knowing which ANCA you have is important because it can change how you treat your disease. For example, c-ANCA is often linked to GPA, while p-ANCA is more common in Microscopic Polyangiitis (MPA) and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
|
Characteristics |
c-ANCA |
p-ANCA |
|---|---|---|
|
Primary Target |
Proteinase 3 (PR3) |
Myeloperoxidase (MPO) |
|
Associated Conditions |
GPA (Granulomatosis with Polyangiitis) |
MPA (Microscopic Polyangiitis), EGPA (Eosinophilic Granulomatosis with Polyangiitis) |
|
Clinical Significance |
Diagnostic marker for GPA |
Associated with MPA and EGPA |
In short, getting the details on c-ANCA, like its target PR3 and how it differs from p-ANCA, is key for right diagnosis and treatment of ANCA-related diseases. The role of c-ANCA, mainly in GPA, shows why it’s so important to get ANCA tests right.
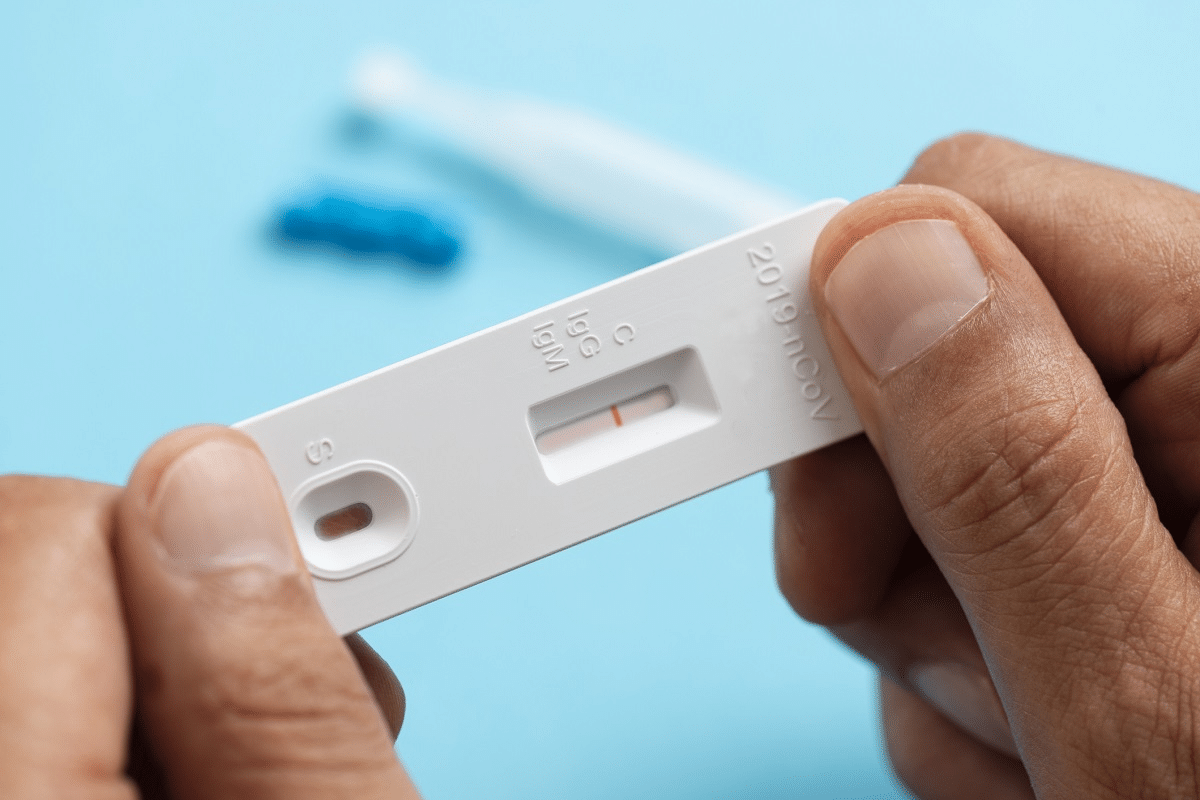
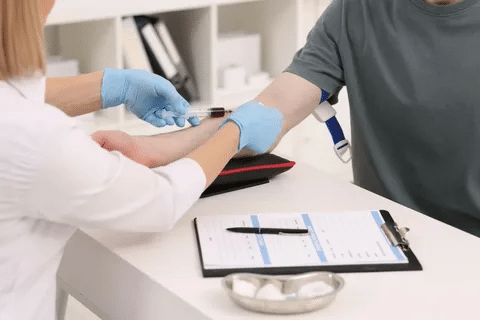
ANCA testing starts with a simple blood draw. It’s key for finding autoimmune diseases, like vasculitis. Knowing the steps can ease worries and prepare patients.
The first step is getting a blood sample. This happens in a place like a hospital or lab. A healthcare worker will clean the area and draw blood with a sterile needle.
The blood goes to an ANCA lab for testing. It’s important the sample is handled right to get accurate results.
At the lab, the blood is checked for anti-neutrophil cytoplasmic antibodies (ANCA). There are two main tests: indirect immunofluorescence (IIF) and enzyme-linked immunosorbent assay (ELISA).
|
Testing Method |
Description |
Use in ANCA Testing |
|---|---|---|
|
Indirect Immunofluorescence (IIF) |
Detects ANCA by looking at the fluorescence on neutrophils. |
First test for ANCA. |
|
Enzyme-Linked Immunosorbent Assay (ELISA) |
Measures specific ANCA levels, like PR3-ANCA and MPO-ANCA. |
Used for confirming and tracking ANCA levels. |
Learning about the neutrophil cytoplasmic ab blood test helps understand the process. IIF and ELISA together help doctors diagnose and treat ANCA-related diseases.
It’s important for patients and doctors to understand what a positive ANCA test means. This test shows the presence of anti-neutrophil cytoplasmic antibodies. These antibodies are linked to autoimmune vasculitis conditions.
The titer level is key when looking at positive ANCA test results. Higher titers often mean active disease or more severe inflammation. For example, a high c-ANCA titer is often seen in Granulomatosis with Polyangiitis (GPA). On the other hand, p-ANCA is more common in Microscopic Polyangiitis (MPA) or Eosinophilic Granulomatosis with Polyangiitis (EGPA).
Knowing the type of ANCA and its titer helps doctors understand the disease’s activity. It also guides treatment decisions.
The accuracy of ANCA testing comes from its sensitivity and specificity. Test sensitivity is about correctly identifying those with the disease. Specificity is about correctly identifying those without the disease. For c-ANCA, the sensitivity for GPA can range from 80% to 90%, depending on the disease activity and the assay used.
But, it’s important to look at these results with clinical symptoms and other diagnostic findings in mind.
Titer levels give valuable insights into the disease’s activity. A rising titer may show a flare or relapse. A decreasing titer suggests a response to treatment.
By watching titer levels over time, doctors can adjust treatment plans. This helps manage patient expectations and improves their quality of life.
In conclusion, understanding positive ANCA test results involves knowing about titer levels, test sensitivity, and specificity. By considering these, doctors can make better decisions for patient care and treatment.
ANCA-associated vasculitis includes three main conditions: Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA). These conditions are marked by the presence of anti-neutrophil cytoplasmic antibodies (ANCA). They cause inflammation in blood vessels, which can harm organs.
Granulomatosis with Polyangiitis, also known as Wegener’s granulomatosis, affects small- and medium-sized vessels. It is known for granulomas in the respiratory tract and is linked to c-ANCA or PR3-ANCA. GPA can damage organs like the lungs, kidneys, and upper respiratory tract.
Key features of GPA include:
Microscopic Polyangiitis mainly affects small vessels. It lacks granulomas and is linked to p-ANCA or MPO-ANCA. MPA often damages the kidneys and lungs, causing rapid kidney failure and lung bleeding.
Key features of MPA include:
Eosinophilic Granulomatosis with Polyangiitis, formerly known as Churg-Strauss syndrome, is rare. It is marked by eosinophilia, asthma, and granulomatous inflammation. It is less commonly linked to ANCA compared to GPA and MPA.
Key features of EGPA include:
Knowing about these conditions is key for correct diagnosis and treatment. Each vasculitis has unique signs and needs a specific treatment plan.
Studies have found a strong link between c-ANCA and certain diseases, like GPA. The presence of c-ANCA, mainly with antibodies against proteinase 3 (PR3), points to GPA.
About 75 to 90 percent of GPA patients have c-ANCA with PR3 antibodies. This shows how useful c-ANCA testing is in diagnosing GPA. It’s not just for diagnosis but also for tracking disease activity and treatment success.
Many studies have looked into ANCA test sensitivity and specificity, focusing on c-ANCA. They found c-ANCA, and PR3 antibodies in particular, are very specific for GPA. Below is a table with key findings from these studies.
|
Study |
Sensitivity (%) |
Specificity (%) |
|---|---|---|
|
Study A |
85 |
95 |
|
Study B |
80 |
98 |
|
Study C |
88 |
92 |
Interpretation: The data confirms c-ANCA testing is both sensitive and specific for GPA. This makes it a key diagnostic tool.
In conclusion, the link between c-ANCA and GPA diagnosis is well-supported by research. Healthcare providers need to understand this to make better decisions on diagnosis and treatment.
ANCA tests are useful for diagnosing diseases, but they can sometimes give wrong results. It’s important to know when this might happen to ensure accurate diagnosis and treatment.
Some medicines can make ANCA tests show false positives. For example, propylthiouracil, used for hyperthyroidism, can lead to ANCA-associated vasculitis (AAV) and positive ANCA tests. Other drugs like hydralazine for high blood pressure and minocycline, an antibiotic, can also cause false positives. Doctors need to look at a patient’s medication history when reading ANCA test results.
ANCA tests are not just for vasculitic diseases. Many non-vasculitic conditions can also show positive ANCA results. For instance, inflammatory bowel disease (IBD), like Crohn’s disease and ulcerative colitis, can sometimes show positive p-ANCA. Also, some infections and autoimmune diseases can lead to positive ANCA results, making diagnosis harder.
Borderline ANCA results are tricky to deal with. In these cases, clinical correlation is key. Doctors must look at the patient’s symptoms, medical history, and other test results to understand borderline ANCA results. Sometimes, repeating the test or doing more tests is needed to make a clear diagnosis.
In summary, ANCA tests are valuable but need careful interpretation. They can lead to false positives, show up in non-vasculitic conditions, and have borderline results. A thorough approach to diagnosis, including clinical findings and other tests, is vital for proper patient care.
Getting a positive ANCA test result can feel overwhelming. But knowing what to do next can help clear things up. A positive result means you have anti-neutrophil cytoplasmic antibodies. These are linked to certain autoimmune diseases, like vasculitis.
After a positive ANCA result, seeing a specialist is the first step. You might see a rheumatologist or a nephrologist. Rheumatologists deal with musculoskeletal diseases and autoimmune conditions. Nephrologists focus on kidney diseases.
Your doctor will decide who to refer you to. If your kidneys are affected, a nephrologist might be best. But if you have systemic symptoms, a rheumatologist could be a better fit.
After a positive ANCA result, more blood tests are usually needed. These tests help understand your condition better. They might include:
These tests help see how far the disease has spread. They also help track how your body is responding to treatment.
Talking about your symptoms with your doctor is very important. Share when your symptoms started, how bad they are, and what makes them better or worse. Symptoms of ANCA-associated vasculitis can be different for everyone. They might include:
Telling your doctor about your symptoms helps them figure out what you have. It also helps them plan the right treatment for you.
To confirm ANCA-associated vasculitis, we need more than just ANCA testing. ANCA tests give us clues, but we must do more to understand the disease fully.
A tissue biopsy is key in diagnosing ANCA-associated vasculitis. It takes a tissue sample from the affected area. This sample is then checked for inflammation and damage. The biopsy helps us see how much of the organ is affected and guides treatment.
For example, a kidney biopsy is important for those with suspected Granulomatosis with Polyangiitis (GPA) or Microscopic Polyangiitis (MPA). Sometimes, a biopsy isn’t possible. But when it is, it’s the best way to diagnose vasculitis and check its activity.
Imaging studies are vital for seeing how much of the body is affected by ANCA-associated vasculitis. Tools like CT scans, MRI, and PET scans show inflammation and damage.
For instance, a CT scan of the chest can spot lung problems in GPA. An MRI can show inflammation in blood vessels and tissues. These studies help in diagnosing and tracking how the disease is doing.
Lab tests and imaging are not enough for a definitive diagnosis. We also need to look at the patient’s symptoms, medical history, and physical exam.
Doctors use established criteria, like those from the American College of Rheumatology, to diagnose. These criteria look at ANCA antibodies, symptoms, and biopsy results.
By combining lab and imaging results with clinical evaluation, doctors can accurately diagnose. They can then create a treatment plan that fits the patient’s needs.
ANCA-associated vasculitis treatment involves several steps. These include induction therapy, maintenance strategies, and monitoring. Each step is tailored to the patient’s needs for effective management.
The first step, induction therapy, aims to control the disease. Immunosuppressants are key, reducing inflammation and preventing organ damage. Cyclophosphamide and rituximab are often used.
After the disease is in remission, maintenance treatment starts. This phase uses less intense treatments like azathioprine or methotrexate. The aim is to keep the disease under control while reducing side effects.
Monitoring ANCA levels is vital in managing ANCA-associated vasculitis. Regular blood tests check disease activity and guide treatment. Rising ANCA levels may signal a higher risk of relapse, leading to closer monitoring or treatment changes.
Combining induction therapy, maintenance strategies, and monitoring helps manage ANCA-associated vasculitis. This approach improves patient outcomes and quality of life.
Long-term care for patients with ANCA-associated vasculitis is key to better outcomes and quality of life. It involves several strategies. These aim to keep the disease in remission, watch for relapse, and care for the patient’s overall well-being.
The main goal in treating ANCA-associated vasculitis is to achieve remission. Remission means no disease activity and often lower or normal ANCA levels. But, it doesn’t mean the disease is completely gone, as relapses can happen.
How often a patient relapses can vary. Some may have many relapses, while others stay in remission for a long time. The initial ANCA type, disease severity at diagnosis, and treatment used can affect relapse risk.
|
Factor |
Influence on Relapse |
|---|---|
|
Initial ANCA Type |
PR3-ANCA associated with higher relapse rates |
|
Disease Severity at Diagnosis |
More severe disease may have higher relapse risk |
|
Treatment Regimen |
Immunosuppressive therapy can reduce relapse risk |
Regular checks are vital to catch early signs of relapse and adjust treatment. This includes blood tests for ANCA levels, inflammation, and organ function. Clinical assessments also help evaluate disease activity.
Monitoring plans can differ based on the patient’s risk factors and disease details. For instance, those with a history of many relapses might need more frequent checks.
Managing ANCA-associated vasculitis goes beyond just controlling the disease. It’s also about improving the patient’s quality of life. This includes managing symptoms, side effects of treatment, and supporting the physical and emotional challenges of chronic illness.
Improving quality of life might involve referrals to specialists like rheumatologists or mental health professionals. It may also include lifestyle changes and supportive care services.
By focusing on long-term management, we can better the lives of patients with ANCA-associated vasculitis. This approach enhances their overall quality of life.
Knowing what a positive ANCA test means is key to treating autoimmune vasculitis. We’ve looked at why ANCA tests are important, what conditions they can show, and what to do after a positive result.
Managing ANCA-associated vasculitis well needs a team effort. This includes seeing specialists, doing more tests, and finding treatments that work for each person. Understanding ANCA tests helps doctors give better care, leading to better health for patients.
In summary, getting the right diagnosis from an ANCA test is essential for treating ANCA vasculitis. Also, new research and teaching patients more about their conditions are vital. They help improve care quality.
ANCAs are autoantibodies that target neutrophils, a type of white blood cell. They are linked to autoimmune diseases affecting blood vessels.
c-ANCA targets proteinase 3 (PR3), while p-ANCA targets myeloperoxidase (MPO). These differences help doctors diagnose and manage diseases like GPA and MPA.
Doctors use ANCA tests to find and track autoimmune diseases like GPA, MPA, and EGPA.
A positive test might show an autoimmune disease. But, it needs more checks, like a biopsy, to be sure.
To test for ANCAs, a blood sample is taken. It’s then checked in a lab using special methods.
The main conditions are GPA, MPA, and EGPA. Each has its own signs and needs special care.
Yes, some medicines can make ANCA tests show false positives. Always tell your doctor about your meds.
After a positive test, see specialists and get more tests. Talk to your doctor about your symptoms for the best care.
Treatment starts with strong medicines to stop the disease. Then, ongoing treatment keeps it from coming back. Watching ANCA levels is also key.
Titer levels show how much ANCA is in your blood. High levels mean active disease. Watching these levels helps see how well treatment is working.
Yes, tests can be wrong in some cases. This includes false positives from medicines or other conditions. Borderline results need careful thought.
Doctors confirm diagnosis with ANCA tests, biopsies, imaging, and clinical checks. They use set criteria for this.
Long-term care aims for remission and watching for relapse. It also focuses on improving quality of life for better outcomes.
National Center for Biotechnology Information. Positive ANCA Test: Meaning and Next Steps. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7527567/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!