Last Updated on December 2, 2025 by Bilal Hasdemir

Nearly 40% of adults in the United States have obesity. Many are looking into weight loss injections as a solution. But, these injections can be very expensive. This makes insurance coverage very important for access.
Some health insurance plans do cover weight loss injections. But, the amount of coverage options can vary a lot. It depends on the provider and plan. Understanding Insurance Coverage for Weight Loss Injections and common restrictions for these treatments.
It’s key to understand your coverage options for weight loss treatments. In this article, we’ll look at the types of weight loss injections covered by insurance. We’ll also guide you on how to check your coverage.
Key Takeaways
- The extent of insurance coverage for weight loss injections varies by provider and plan.
- Some health insurance plans cover certain types of weight loss injections.
- Understanding your coverage options is key for making informed decisions.
- The cost of weight loss injections can be a big issue for those without good coverage.
- Reviewing your health insurance plan’s coverage policy is essential.
Understanding Weight Loss Injections
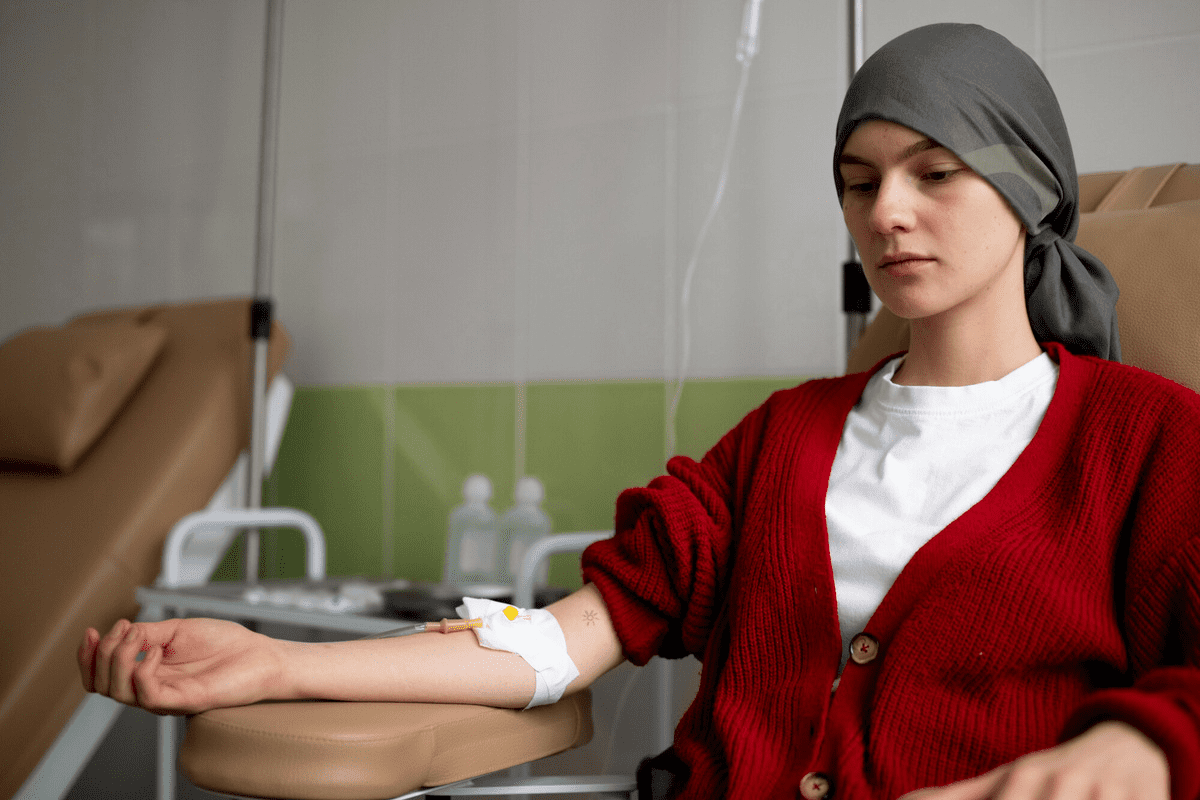
GLP-1 receptor agonists in weight loss injections mimic a natural hormone. This hormone helps reduce hunger. These injections are known for their effectiveness in managing obesity.
What Are Weight Loss Injections?
Weight loss injections are medications given through an injection to help lose weight. They contain ingredients like GLP-1 receptor agonists. These are found in medications like Wegovy and Ozempic.
Key characteristics of weight loss injections include:
- Prescription-only medication
- Administered via injection, usually once a week
- Contain active ingredients like GLP-1 receptor agonists
- Designed to help reduce hunger and increase feelings of fullness
How Weight Loss Injections Work
Weight loss injections mimic a natural hormone in the body. This hormone controls appetite and food intake. GLP-1 receptor agonists, for example, work by:
- Slowing gastric emptying, making you feel fuller for longer
- Reducing appetite by acting on the brain’s appetite centers
- Improving insulin sensitivity, which helps regulate blood sugar levels
The effectiveness of weight loss injections varies. It depends on the individual, the medication type, and health factors. Always consult a healthcare provider to find the best treatment.
Types of Weight Loss Injections Potentially Covered by Insurance
There are many weight loss injections available, each with its own insurance coverage. It’s important for patients to know about these options when looking for weight loss treatments.
GLP-1 Receptor Agonists
GLP-1 receptor agonists are popular for weight loss. They work by mimicking a hormone that controls hunger and food intake. Examples include semaglutide (Wegovy) and liraglutide (Saxenda).
Insurance coverage for these injections varies. Many plans cover them for people with a BMI of 30 or higher. Or for those with a BMI of 27 or higher and a weight-related condition.
A study in a Journal showed semaglutide helps with weight loss. “Semaglutide helps with weight loss, improves heart health, and lowers diabetes risk.”
“The use of GLP-1 receptor agonists represents a significant advancement in the treatment of obesity, providing a new option for those struggling with diet and exercise.”
N Engl J Med
Vitamin B12 and Lipotropic Injections
Vitamin B12 and lipotropic injections are another weight loss option. They contain vitamins, minerals, and amino acids to boost fat metabolism and energy. Insurance coverage for these injections is limited and often requires proof of a vitamin deficiency.
Injection Type | Common Ingredients | Insurance Coverage |
Vitamin B12 | Vitamin B12, saline solution | Limited coverage; may require proof of deficiency |
Lipotropic | Methionine, inositol, choline, vitamin B12 | Variable coverage; often considered cosmetic |
HCG Injections and Coverage Limitations
HCG injections are used with a very low-calorie diet for weight loss. But, insurance coverage for HCG injections is limited. This is due to concerns about their effectiveness and misuse. Many plans see HCG injections as cosmetic and don’t cover them.
In conclusion, insurance coverage for weight loss injections varies widely. Patients should talk to their healthcare provider and insurance company. This will help them understand their options and find the best treatment.
Insurance Coverage for Weight Loss Injections: The Basics
Whether insurance covers weight loss injections depends on a few key things. These include if the treatment is medically necessary and if it has FDA approval. Knowing these basics helps you understand insurance coverage better.
Medical Necessity vs. Cosmetic Procedures
Insurance coverage for weight loss injections depends on if it’s medically necessary or cosmetic. Medically necessary treatments are for diagnosing or treating a medical condition. Cosmetic procedures are for improving looks and are not needed.
Weight loss injections might be medically necessary for people with obesity-related health problems. For example, some GLP-1 receptor agonists help with weight loss and also improve heart health and manage type 2 diabetes.
FDA Approval and Insurance Recognition
FDA approval is key in deciding if insurance covers weight loss injections. Insurance providers are more likely to cover treatments with FDA approval. For example, semaglutide (Wegovy) is approved for weight management in some patients.
FDA-Approved Weight Loss Injections | Insurance Coverage Likelihood |
Semaglutide (Wegovy) | High |
Liraglutide (Saxenda) | High |
Off-label use of GLP-1 receptor agonists | Variable |
Pre-authorization requirements also affect insurance coverage. Many insurance providers need a pre-authorization before prescribing weight loss injections. This adds another step to the approval process.
Criteria for Insurance Approval of Weight Loss Treatments
It’s important to know what insurance looks for when approving weight loss treatments. They check several things before saying yes to coverage for injections or other treatments.
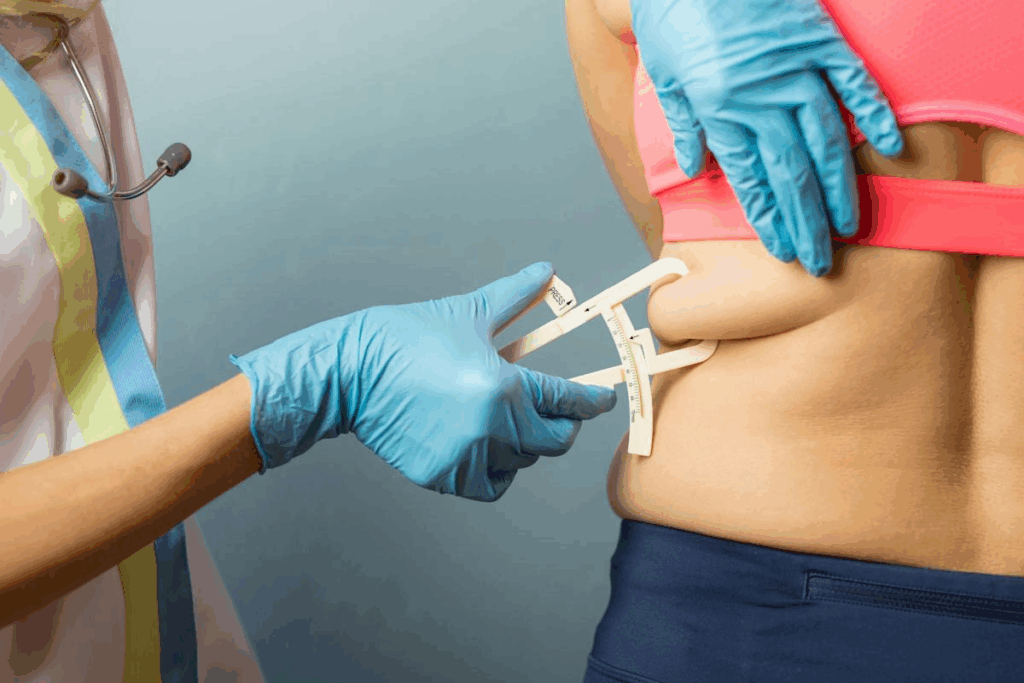
BMI Requirements and Classification
Insurance first looks at your Body Mass Index (BMI). BMI helps figure out if you’re at a healthy weight or not. To get coverage, your BMI usually needs to be 30 or higher.
The World Health Organization has a way to classify BMI:
BMI Category | BMI Range |
Underweight | Less than 18.5 |
Normal weight | 18.5-24.9 |
Overweight | 25-29.9 |
Obese | 30 or greater |
Comorbidity Considerations
Insurance also looks at other health issues you might have. These are called comorbidities. They can include:
- Diabetes
- Hypertension
- Cardiovascular disease
- Sleep apnea
Having these conditions can help your case for getting treatment. For example, someone with a BMI of 35 and diabetes might get approved faster.
“The presence of comorbidities can significantly influence insurance coverage decisions for weight loss treatments.”
Prior Weight Loss Attempt Documentation
Insurance also wants to see if you’ve tried to lose weight before. They might ask for:
- Records of diets or weight loss programs
- Proof of exercise
- Info on any weight loss meds or surgery
Insurance companies look at your health and past weight loss efforts carefully. They want to make sure you really need the treatment.
Pre-Authorization Requirements for Weight Loss Injections
Before starting weight loss injections, it’s important to know the pre-authorization rules from your insurance. Pre-authorization checks if the treatment is needed and fits the insurance’s rules.
Understanding the Pre-Authorization Process
The pre-authorization process for weight loss injections has several steps. First, your doctor must ask your insurance for approval. They need to share your medical history, the treatment plan, and why you need weight loss injections.
Key components of the pre-authorization request typically include:
- Patient medical history and current health status
- Details of the prescribed weight loss injection
- Rationale for the treatment, including previous weight loss attempts
- Expected outcomes and treatment plan
Insurance companies check this info to see if the treatment is covered. This can take a few days to weeks, depending on the case and the insurer’s work.
Common Reasons for Pre-Authorization Denial
Knowing why pre-authorization is denied helps patients and doctors prepare better. Common reasons include:
Reason for Denial | Description |
Lack of Medical Necessity | The insurer may deny coverage if they think the weight loss injection is not needed based on your health. |
Insufficient Documentation | Not having enough medical records and weight loss history can lead to denial. |
Non-FDA Approved Use | Using weight loss injections for reasons not approved by the FDA can be denied, as insurers only cover FDA-approved treatments. |
By knowing the pre-authorization process and common denials, patients and doctors can better get coverage for weight loss injections.
Documentation Needed for Insurance Coverage
To get insurance for weight loss injections, you need to know what documents are required. Insurance companies want to see your medical history and records. They use this to decide if the treatment is needed.
Medical Records and History
Your medical records are key to getting insurance approval. They should show your weight loss history, any past attempts, and health conditions. Comprehensive medical records help insurers see why you need the injections.
Here’s what your medical history should include:
- Previous weight loss attempts and their results
- Your current weight and BMI
- Any health conditions or related issues
- Previous weight loss treatments or medications
Physician Statements and Recommendations
Physician statements are also very important. They should explain why you need the injections. They should talk about the expected results and how it fits into your health plan.
A good physician statement should:
- Explain why the injections are medically necessary
- Describe your current health and medical history
- Discuss the treatment’s duration and follow-up plans
Proof of Previous Weight Loss Attempts
Showing you’ve tried other weight loss methods is also important. This can include diet plans, exercise, or other treatments. Detailed documentation shows you’ve tried other options before injections.
Documentation Type | Description | Importance Level |
Medical Records | Detailed patient medical history | High |
Physician Statements | Physician’s recommendation and justification | High |
Proof of Previous Attempts | Records of previous weight loss attempts | Medium |
Having all the right documents can help you get insurance for weight loss injections. It’s smart to work with your healthcare team. They can help make sure everything is correct and submitted properly.
Medicare and Medicaid Policies on Weight Loss Treatments
Understanding public insurance for weight loss injections is complex. Medicare and Medicaid are key, covering millions of Americans. Yet, their weight loss treatment policies differ.
Medicare Coverage Guidelines
Medicare mainly helps those 65 and older. It has rules for weight loss treatments. Medicare covers some services, but only for those with high BMI or obesity-related health issues.
Key factors influencing Medicare coverage include:
- Medical necessity, as determined by a healthcare provider
- FDA approval of the weight loss treatment
- Presence of comorbidities that could be improved with weight loss
Medicaid Variations by State
Medicaid helps low-income families and individuals. Its weight loss treatment policies vary by state. Some states cover more services, like injections, while others are more restrictive.
Factors contributing to state variations include:
- State-specific Medicaid eligibility criteria
- Differences in covered services and treatments
- Prior authorization requirements and processes
It’s vital to know these differences for Medicaid weight loss treatments. Check with state Medicaid offices or healthcare providers for specific coverage.
Private and Employer-Sponsored Insurance Plans
It’s important to know how private and employer-sponsored insurance plans work for weight loss injections. These plans help decide if treatments are affordable for many people.
Common Coverage Policies Among Major Insurers
Big insurance companies have different rules for weight loss injections. For example, UnitedHealthcare and Aetna might cover some injections but not others. This depends on the treatment’s need and the patient’s health.
Insurance companies need proof that the treatment is needed. They look at past weight loss efforts and health problems to decide.
Self-Insured Employer Plan Considerations
Self-insured plans, paid by employers, can be more flexible. They might cover weight loss injections better if the employer thinks it’s good for employees.
But, what’s covered can really vary. It’s key for people to check their plan details or talk to HR to know what’s included.
Insurance Plan Type | Coverage for Weight Loss Injections | Typical Requirements |
Fully Insured Plans | Varies by insurer | Medical necessity, previous weight loss attempts |
Self-Insured Employer Plans | Depends on employer’s policy | May require additional documentation or justification |
Knowing your insurance plan well helps you get weight loss injections covered.
Consultation with Insurance Representatives
Talking to insurance reps is key when dealing with weight loss injections. It helps clear up what’s covered and what you need to get approved.
Questions to Ask Your Insurance Provider
It’s important to ask the right questions to fully understand your coverage. You might want to ask about:
- The specific criteria for coverage of weight loss injections
- Any pre-authorization requirements or documentation needed
- The process for appealing a denied claim
- Any out-of-pocket costs associated with the treatment
Documenting Conversations and Commitments
It’s important to write down what’s said during your talk with insurance reps. This includes:
- Recording the date and time of the conversation
- Noting the representative’s name and contact information
- Detailing the information provided and any agreements or next steps discussed
This way, you have a clear record of your talks. You can look back at them when you need to.
Good communication with your insurance provider is essential to know your coverage options. By asking the right questions and keeping a record of your talks, you can go through the process with confidence.
Out-of-Pocket Costs When Insurance Doesn’t Cover
When insurance doesn’t cover weight loss injections, patients face high costs. This can be a big financial challenge. It’s important to know the costs and look for help.
Average Costs of Different Weight Loss Injections
The price of weight loss injections changes based on the medication, dosage, and how often you get them. On average, you might pay $300 to $1,000 a month. Here’s a look at the average costs for different injections:
Weight Loss Injection | Average Monthly Cost |
Saxenda | $1,200 – $1,500 |
Wegovy | $1,300 – $1,600 |
Contrave | $300 – $500 |
Manufacturer Assistance Programs and Discounts
Manufacturers help make weight loss injections more affordable. They offer programs and discounts. For example, Wegovy’s savings card can cut the monthly cost by up to $300 for those with commercial insurance.
There are different kinds of help available:
- Co-pay savings cards
- Patient assistance programs (PAPs)
- Discount cards
Patients should talk to their doctor or check the manufacturer’s website. This way, they can find out about available help and if they qualify.
Regional Variations in Weight Loss Injection Coverage
The world of insurance for weight loss injections shows big regional variations. These changes greatly affect how easy it is for people to get these treatments. It all depends on where you live in the United States.
State-by-State Coverage Differences
Insurance for weight loss injections changes a lot from state to state. Some places offer more coverage, while others have strict rules or no coverage at all.
For example, states with more obesity might cover weight loss treatments better. But, other states might have less coverage because of their insurance rules or health issues.
Urban vs. Rural Access Disparities
There’s also a big difference in getting weight loss injections between cities and rural areas. Cities usually have more doctors and treatment choices.
Rural areas, though, have fewer doctors and it’s harder to get to them. They also might have less insurance options. This makes it harder for people in these areas to get the help they need.
It’s important for doctors and patients to know about these regional variations. It helps plan care and fight for fair insurance rules everywhere.
Impact of Comorbidities on Insurance Coverage Decisions
Knowing how comorbidities affect insurance for weight loss injections is key. These conditions can change how insurance decides to cover treatments. Comorbidities are extra health issues that often come with a main condition. They are important in deciding if weight loss treatments are needed.
Diabetes and Coverage Implications
Diabetes is a big comorbidity that can affect insurance for weight loss injections. People with diabetes are at higher risk for obesity problems. So, insurance might cover weight loss injections more easily for them.
For example, some GLP-1 receptor agonists help manage diabetes and aid in weight loss. Insurance might cover these more because they serve two purposes.
Cardiovascular Disease Considerations
Cardiovascular disease also affects insurance for weight loss injections. It makes weight loss a key part of treatment for those at risk. Insurance might see weight loss injections as a necessary treatment for these patients.
This could lead to better insurance coverage for them.
Other Qualifying Health Conditions
Other health issues can also influence insurance for weight loss injections. This includes sleep apnea, mental health conditions, and other obesity-related problems.
Having these conditions can show why weight loss treatments are needed. This might make insurance more likely to cover them.
In summary, comorbidities are very important in insurance decisions for weight loss injections. Understanding how diabetes and heart disease affect these decisions helps people better understand insurance for weight loss treatments.
Monitoring and Follow-Up Requirements for Continued Coverage
Keeping up with ongoing monitoring and documentation is key for keeping insurance coverage for weight loss injections. Insurance companies want regular updates and progress reports. They check if the treatment is working and safe.
Required Check-Ins and Progress Documentation
Patients must stick to a schedule of follow-up appointments with their healthcare provider. These visits help track weight loss, check for side effects, and adjust treatment plans if needed.
Key components of follow-up care may include:
- Regular weight checks
- Blood work to monitor metabolic changes
- Assessment of overall health and well-being
- Adjustments to dosage or treatment regimen
Keeping records of these visits is very important. Insurance providers might ask for this information to decide if coverage should continue.
Coverage Limitations Based on Treatment Response
How much insurance covers for weight loss injections can depend on how well the treatment works. Insurance companies have their own rules for what counts as a successful outcome.
Treatment Outcome | Coverage Implications |
Significant weight loss (>5% body weight) | Continued coverage likely |
Moderate weight loss (2-5% body weight) | Coverage may be continued with additional documentation |
Minimal weight loss ( | Coverage may be discontinued or alternative treatments considered |
In some cases, insurance providers might compare weight loss injections to other treatments, like surgery, to decide on coverage.
It’s essential for patients to work closely with their healthcare providers to ensure that all necessary documentation is in place to support continued coverage.
Appealing Denied Claims for Weight Loss Treatments
It’s important for patients to know how to appeal denied insurance claims for weight loss treatments. Insurance companies might deny claims for many reasons. But, patients can appeal these decisions.
Step-by-Step Appeal Process
The appeal process has several steps that patients need to follow. Here’s what you need to do:
- Review the denial letter: Understand why your claim was denied and the policy or guideline used.
- Gather supporting documentation: Collect medical records, doctor statements, and any other important information.
- Submit a formal appeal: Write a clear, concise appeal letter explaining why the treatment is needed.
- Follow up: Make sure the insurance company gets your appeal and track its progress.
Step | Description | Key Documents |
1 | Review denial letter | Denial letter, insurance policy |
2 | Gather supporting docs | Medical records, physician statements |
3 | Submit formal appeal | Appeal letter, supporting docs |
Success Rates and Strategies
The success of an appeal depends on the quality of the appeal and the case’s specifics. Effective strategies include showing the medical need for the treatment and how it fits the insurance policy.
Patients might also want to get help from patient advocacy groups or work with their healthcare provider. This can make their appeal stronger.
Patient Advocacy for Weight Loss Treatment Coverage
Getting insurance to cover weight loss injections can be tough. It takes a lot of effort from both patients and healthcare providers. Advocacy is more than just dealing with the healthcare system. It’s about making sure people get the care they need, with support from their insurance.
Working with Your Healthcare Provider
Healthcare providers are key in fighting for weight loss treatment coverage. By teaming up with your doctor, you can make a strong case for insurance coverage. This partnership involves:
- Keeping a record of your medical history and past weight loss efforts
- Learning why weight loss injections are medically necessary for you
- Getting a doctor’s letter explaining why you need these injections
A healthcare expert says, “A good relationship between patient and provider can really help with insurance claims for weight loss treatments.”
“The success of patient advocacy depends on the details of the case and the patient’s bond with their healthcare provider.”
An Endocrinologist
Utilizing Patient Advocacy Organizations
Using patient advocacy groups can also help a lot. These groups are experts at helping patients get insurance for treatments like weight loss injections.
Organization | Services Offered | Contact Information |
National Patient Advocate Foundation | Case management, insurance appeals assistance | www.npaf.org |
Patient Access Network Foundation | Insurance coverage assistance, patient assistance programs | www.panfoundation.org |
By using these resources and working with your doctor, you can boost your chances of getting insurance for weight loss treatments.
Conclusion: Navigating Insurance Coverage for Weight Loss Injections
Understanding insurance for weight loss injections is complex. It involves knowing about insurance policies, what’s medically necessary, and how to appeal. Insurance plans for these injections vary a lot.
It’s key to know what insurance looks for, like your BMI and health conditions. Also, knowing what documents you need can make things easier.
Weight loss injections can really help with keeping weight off over time. Knowing about insurance can help you choose the right treatment. Working with your doctor and insurance can make things clearer.
Getting to know how insurance works for weight loss injections helps you make better choices. This leads to better weight management in the long run.
FAQ
What are weight loss injections and how do they work?
Weight loss injections are medicines given through an injection to help with weight loss. They work by reducing hunger, making you feel full, or boosting your metabolism. Examples include GLP-1 receptor agonists like semaglutide (Wegovy) and liraglutide (Saxenda).
What types of weight loss injections are potentially covered by insurance?
Insurance might cover GLP-1 receptor agonists, vitamin B12, and lipotropic injections. But HCG injections are usually not covered because they’re not FDA-approved for weight loss.
How do insurance companies determine medical necessity for weight loss injections?
Insurance companies look at your BMI and health conditions. They need a BMI of 30 or higher, or 27 with health issues. They also check if you’ve tried to lose weight before and if the medication is FDA-approved for weight loss.
What is the pre-authorization process for weight loss injections, and why is it important?
Pre-authorization means your doctor asks the insurance company to approve the treatment. It’s key for weight loss injections because it decides if insurance will pay for it. Reasons for denial include not being medically necessary or lacking proper documentation.
What documentation is needed for insurance coverage of weight loss injections?
You’ll need medical records, doctor’s statements, and proof of previous weight loss efforts. Good documentation is key to show the treatment is needed.
Does Medicare or Medicaid cover weight loss injections?
Medicare might cover weight loss injections like Wegovy under certain conditions. Medicaid coverage varies by state, with some states covering weight loss treatments under specific circumstances.
How do private and employer-sponsored insurance plans cover weight loss injections?
Coverage policies differ among major insurers, but some might cover weight loss injections if deemed necessary. Self-insured employer plans can have different rules, so it’s important to check your plan details.
What are the out-of-pocket costs for weight loss injections if insurance doesn’t cover them?
Costs depend on the medication and dosage. You might find discounts or assistance programs to help. Prices can range from $500 to over $1,000 per month for some GLP-1 receptor agonists.
How do comorbidities impact insurance coverage for weight loss injections?
Conditions like diabetes or heart disease can help show why you need weight loss injections. This can increase your chances of getting insurance to cover them.
What are the monitoring and follow-up requirements for continued insurance coverage?
Insurance companies often want regular updates and progress reports to keep coverage. They also look at how well the treatment is working. If it’s not effective, coverage might be limited or stopped.
How can I appeal a denied claim for weight loss treatment coverage?
To appeal, you’ll need to provide more information, like medical records or a doctor’s letter. This supports the need for the treatment. A well-prepared appeal can improve your chances of success.
What role does patient advocacy play in obtaining insurance coverage for weight loss treatments?
Patient advocacy is very important. Working with your doctor and using patient advocacy groups can help you navigate insurance and appeal denied claims.
Are there regional variations in insurance coverage for weight loss injections?
Yes, coverage can differ by state and even within areas. State Medicaid policies and access to healthcare can affect coverage.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/obesity/data/adult.html