Last Updated on December 1, 2025 by Bilal Hasdemir
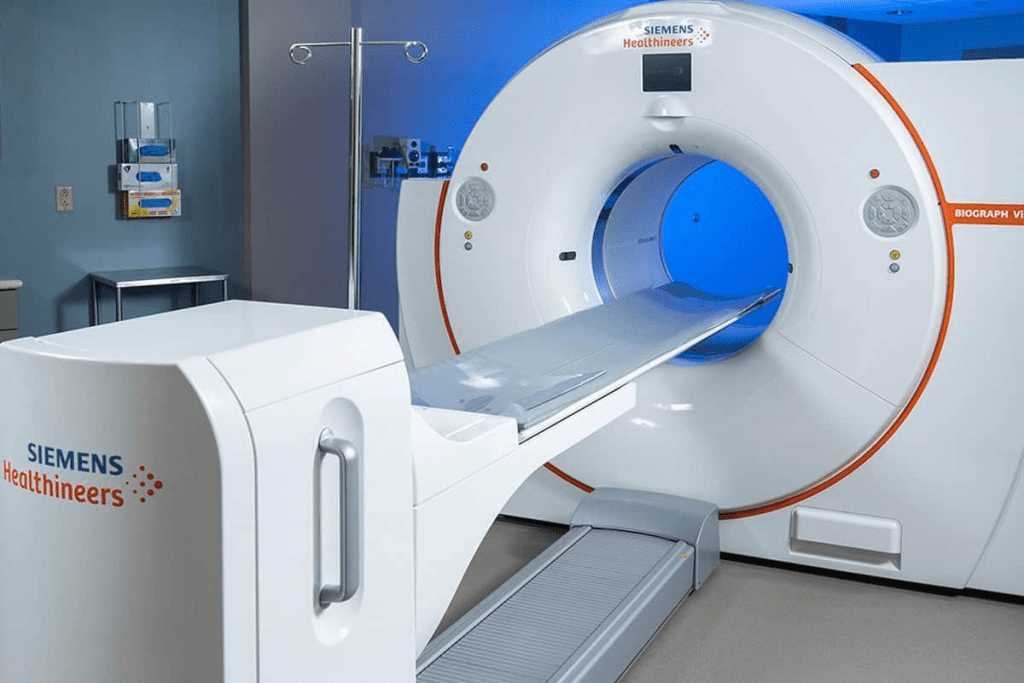
Nearly 1 in 5 medical imaging procedures, like PET scans, face insurance denials. This leaves patients and healthcare providers in a tough spot. PET scans are key for diagnosing health issues, like cancer, neurological problems, and heart disease.
When insurance denies coverage for these scans, it can slow down diagnosis and treatment. This delay can affect patient outcomes. It’s important to know why these denials happen, like for lack of prior authorization or not being medically necessary. This knowledge helps navigate the complex healthcare system.
Key Takeaways
- PET scan denials can significantly impact patient care and treatment timelines.
- Lack of prior authorization is a common reason for insurance denial.
- Understanding insurance policies can help reduce denial rates.
- Healthcare providers play a critical role in advocating for patients.
- Appealing denied claims can be an effective strategy.
Understanding PET Scans and Their Medical Importance

PET scans are key in modern medicine. They show how the body’s cells work. This is important for finding and treating diseases like cancer and brain disorders.
What is a PET scan?
A PET scan uses a special sugar molecule to see how the body works. It spots areas where cells are using a lot of sugar, This helps doctors find problems in organs and tissues.
Common medical uses for PET scans
In cancer care, PET scans help find and track tumors. They also help doctors see how well treatments are working. For brain diseases, like Alzheimer’s and Parkinson’s, PET scans are very helpful. They can also check for heart disease.
The diagnostic value of PET imaging
PET scans give doctors a detailed look at how the body functions. They work with other imaging tests like CT and MRI. This helps doctors understand a patient’s health better. It makes PET scans a vital tool in diagnosing and treating diseases.
Insurance deny PET scan reasons: An Overview
Insurance companies often deny coverage for PET scans. This is a common problem. PET scans are key for diagnosing diseases, but insurers have many reasons to deny them. Insurance Deny PET Scan Reasons
Many patients face frustration when insurance deny PET scan reasons seem unclear. Insurance providers often reject PET scans due to high costs, lack of medical necessity, or insufficient documentation from physicians. Some policies only approve PET scans for specific cancers or advanced stages. Denials may also occur if prior authorization isn’t obtained. Understanding the common insurance deny PET scan reasons helps patients prepare stronger claims, provide supporting medical records, and appeal effectively. Clear communication with your doctor and insurer can improve approval chances.
Most Common Reasons for Denial
There are several reasons why insurance denies PET scan claims. The main ones are:
- Lack of medical necessity
- Insufficient documentation
- Use of PET scans for non-approved indications
- Experimental or investigational indications
Lack of medical necessity is a big reason for denial. Insurers need to see that PET scans are really needed for diagnosis or treatment. Insufficient documentation is another issue. If medical records don’t fully support the need for a PET scan, it can be denied.
Statistics on PET Scan Denials
Many PET scan claims are denied. About 20% of claims are denied at first, but many of these are overturned on appeal.
“The denial of PET scans can significantly delay diagnosis and treatment, impacting patient outcomes.”
Medical Professional
Impact of Denials on Patient Care
PET scan denials can really affect patient care. Delayed diagnosis and treatment can lead to worse outcomes. It also means higher healthcare costs and more stress for patients and their families.
It’s important to understand why PET scans are denied. This helps healthcare providers and patients deal with appeals better. By knowing the common reasons and making sure documentation is good, claims are more likely to be approved.
Medical Necessity Requirements

To get insurance for a PET scan, it’s key to show it’s medically necessary. Insurance companies have certain rules to decide if a PET scan is needed.
Defining Medical Necessity
Insurers define medical necessity by looking at guidelines, clinical criteria, and the patient’s condition. This is important to know if a PET scan is covered.
The rules for medical necessity can differ among insurance companies. But, it usually means PET scans are needed for conditions where they help a lot in diagnosis or predicting outcomes.
Conditions Typically Considered Necessary for PET Scans
PET scans are often seen as medically necessary for a few conditions, like:
- Cancer staging and restaging
- Monitoring treatment response in cancer patients
- Diagnosing and managing certain neurological disorders
These conditions are backed by guidelines that show PET scans are key in managing patients.
Documentation Proving Medical Necessity
Healthcare providers must show the need for PET scans with detailed clinical info and evidence. This is vital for insurance claims to be handled right.
The needed documents might include:
- Detailed patient medical history
- Clinical notes explaining why a PET scan is needed
- Results of previous tests
- Physician’s reason for the PET scan
Having all the right documents can make the insurance claims process smoother.
Prior Authorization Process for PET Scans
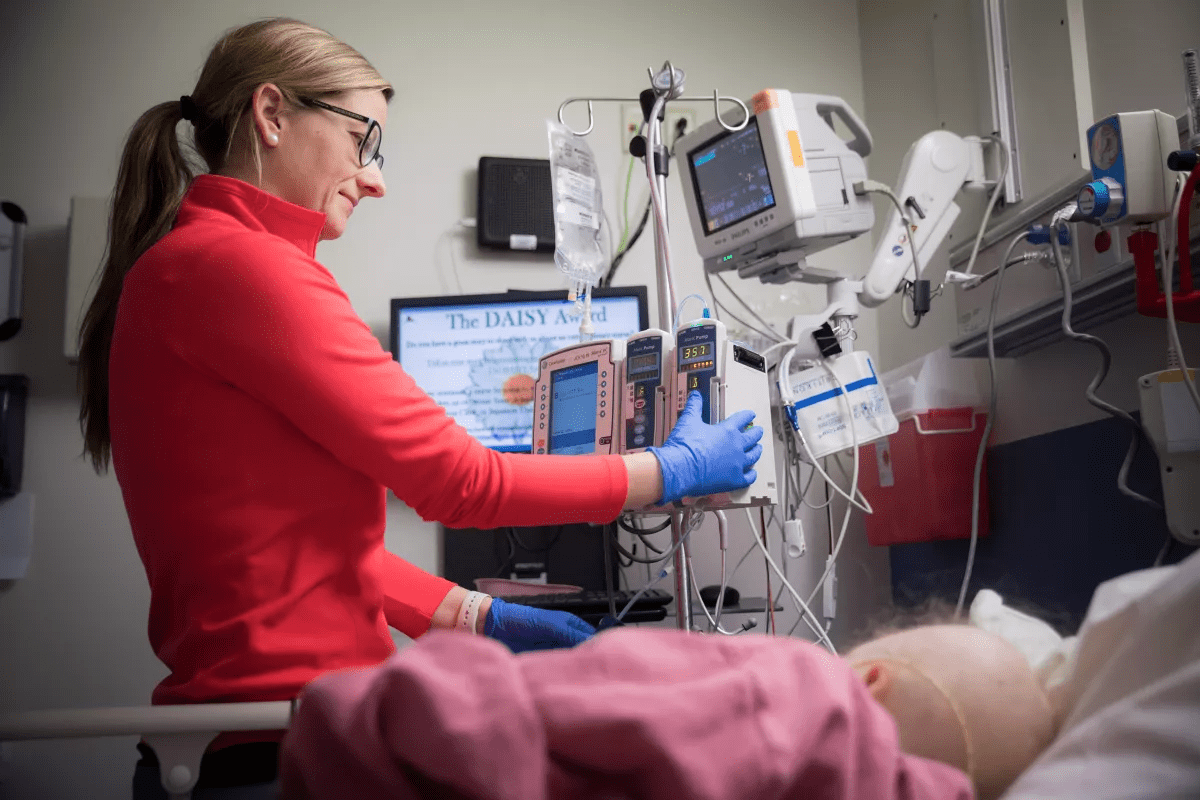
The prior authorization process is key to getting insurance approval for a PET scan. Healthcare providers must get approval from insurers before they can do the test.
What is Prior Authorization?
Prior authorization helps insurance companies manage healthcare costs. It makes sure medical services, like PET scans, are really needed. Insurers ask for detailed clinical info to support the need for the scan.
Timeline for Authorization Requests
The time it takes for prior authorization can vary. It usually takes a few days to a few weeks. Healthcare providers need to send in the needed info quickly to avoid delays in care.
To manage the timeline well, healthcare providers should:
- Check the insurer’s prior authorization needs.
- Send in all the right and correct info.
- Keep in touch with the insurer to make sure it’s processed on time.
Information Required for Submission
The info needed for prior authorization includes:
- The patient’s diagnosis and medical history.
- The treatment plan and any important clinical notes.
- Why the PET scan is needed and how it will help the patient.
Understanding the prior authorization process and sending in the right info helps healthcare providers get approval for PET scans quickly. This ensures patients get the care they need.
Lack of Proper Documentation
Not having the right documents is a big problem for getting PET scans approved. Insurers need detailed medical info to handle claims well.
Essential Medical Records for Approval
Healthcare providers must give comprehensive medical records for PET scan claims. These records should have the patient’s diagnosis, treatment plan, and medical history. This info helps show why the PET scan is needed.
Important medical records usually include:
- Patient’s medical history
- Current diagnosis and staging
- Treatment plans and previous therapies
- Relevant laboratory and imaging results
Physician Justification Requirements
Physician justification is key for PET scan claims. The doctor must explain why a PET scan is needed. This should match medical guidelines and the patient’s needs.
Common Documentation Errors
Common mistakes in documents can cause delays or denials in PET scan claims. These mistakes are:
- Incomplete or wrong patient info
- Missing detailed treatment plans
- Not enough reason for the PET scan
- Missing important medical history
To fix these problems, healthcare providers need to make sure documents are complete, correct, and sent on time. This helps claims get processed faster and avoids denials because of missing documents.
Alternative Imaging Preferences by Insurance Companies
Insurance providers often choose alternative imaging techniques for initial diagnoses. This choice can greatly affect the tests patients undergo.
CT Scans as First-Line Alternatives
Computed Tomography (CT) scans are often the first choice by insurance companies. CT scans provide detailed images that help diagnose many conditions, from injuries to complex diseases like cancer.
Insurance companies prefer CT scans because they are widely available, quick, and give a lot of information. But, the choice can change based on the condition and the patient’s history.
MRI Preference Policies
Magnetic Resonance Imaging (MRI) is also a preferred choice for certain conditions by insurance companies. MRI is great for soft tissue imaging and is used for brain, spine, and joint issues.
Insurance companies have specific rules for MRI use, like needing prior approval and proof of medical need.
Step Therapy Requirements for Imaging
Step therapy is a strategy by insurance companies. It requires patients to try less expensive treatments first before more expensive ones like PET scans.
In imaging, step therapy means using CT or MRI scans before a PET scan. This is to use the most cost-effective tools first, saving advanced imaging for when it’s really needed.
| Imaging Modality | Typical Use | Insurance Preference |
| CT Scan | Initial diagnosis for various conditions | Often preferred as first-line |
| MRI | Soft tissue imaging, brain, spine, and joints | Preferred for specific conditions |
| PET Scan | Cancer diagnosis, staging, and monitoring | Reserved for specific indications |
Evidence-Based Guidelines and Insurance Policies
Insurance policies for PET scans are now guided by evidence-based guidelines. These guidelines come from trusted medical organizations. They help decide when PET scans are the right choice for different health issues.
National Comprehensive Cancer Network Guidelines
The National Comprehensive Cancer Network (NCCN) sets guidelines that doctors and patients trust. These guidelines cover many cancers. They suggest when to use PET scans for diagnosis, staging, and checking how treatments are working.
Key aspects of NCCN guidelines include:
- Evidence-based recommendations for PET scan use in oncology
- Specific criteria for the appropriate timing of PET scans during cancer treatment
- Guidance on the use of PET scans in monitoring treatment response
American College of Radiology Appropriateness Criteria
The American College of Radiology (ACR) offers Appropriateness Criteria for imaging, including PET scans. These criteria are based on solid evidence and expert opinions.
The ACR Appropriateness Criteria cover a wide range of topics, including:
- Use of PET scans in cancer diagnosis and staging
- Appropriateness of PET scans for certain clinical scenarios
- Comparison of PET scans with other imaging modalities
How Insurers Interpret Clinical Guidelines
Insurance companies use guidelines from the NCCN and ACR to decide on PET scan coverage. They look at these guidelines to figure out which PET scan uses are covered and when.
It’s important for healthcare providers to know how insurers use these guidelines. This helps them understand insurance policies for PET scans better. By keeping up with guidelines and policies, providers can fight for their patients’ needs.
Frequency Limitations and Repeat Scan Denials
Insurance companies have strict rules about how often PET scans can be done. These rules help control costs and make sure tests are used wisely. But, they can also mean saying no to scans that are really needed.
Time Restrictions Between Scans
Insurance often sets a time limit between PET scans. For example, they might say you can’t have a scan too soon after the last one. This can be tough for patients who need scans more often because of their health. Doctors need to know about these rules to help their patients and fight for what they need.
Multiple Scan Limitations
Some insurance also puts a cap on how many PET scans you can have in a certain time. This is really hard for people with long-term health issues. For instance, someone with cancer might need many scans to check if treatment is working. Limits on scans can make it hard to give the best care.
Surveillance Scan Policies
Insurance also has rules for surveillance scans. These scans keep an eye on patients, often those with cancer or other ongoing health issues. Insurance might say how often these scans can happen, and deny them if you ask for more. Doctors need to know these rules to help their patients get the care they need.
In summary, limits on how often scans can be done and denials for more scans are big worries for patients and doctors. Knowing the insurance rules about PET scans helps doctors fight for their patients’ care.
Medicare Coverage Criteria for PET Scans
The Centers for Medicare & Medicaid Services (CMS) sets rules for PET scan coverage under Medicare. These rules help make sure PET scans are used right for diagnosing and treating medical conditions, like cancer.
Approved Indications
Medicare pays for PET scans for specific reasons, mainly for cancer diagnosis, staging, and treatment tracking. Approved indications include finding and staging different cancers, checking how well cancer treatment works, and spotting cancer coming back.
- Cancer diagnosis and staging
- Treatment monitoring and assessment
- Detection of cancer recurrence
National Coverage Determination Policies
National Coverage Determination (NCD) policies give more details on Medicare coverage for PET scans. These policies say when PET scans are covered, making sure they’re needed and used right.
NCD policies are based on solid medical evidence. They help make sure coverage decisions are the same everywhere, across different Medicare Administrative Contractors (MACs).
Medicare Advantage vs. Original Medicare Differences
It’s important to know the differences between Medicare Advantage and Original Medicare for PET scan coverage. While Original Medicare sticks to NCD policies, Medicare Advantage plans might have their own rules.
Key differences between Medicare Advantage and Original Medicare include:
| Coverage Aspect | Original Medicare | Medicare Advantage |
| NCD Policies | Follows CMS NCD policies | May have additional coverage criteria |
| Prior Authorization | Required for certain PET scans | May require prior authorization; varies by plan |
| Out-of-Pocket Costs | Standard deductibles and coinsurance | Varies by plan; may have different cost-sharing |
Medicaid PET Scan Approval Guidelines
Understanding Medicaid’s PET scan coverage is key for healthcare providers. It helps them meet the complex rules for PET scans. Medicaid’s rules for PET scans differ from state to state, with each having its own policies.
Coverage Variation Across States
Medicaid’s rules for PET scans vary across the U.S. Each state has its own rules, so providers need to know their state’s specific guidelines.
Required Prior Treatments
The treatments needed before a Medicaid PET scan approval also change by state. Some states might ask for certain treatments or tests before approving a PET scan.
Documentation Standards
Medicaid’s rules for PET scan approval are strict and vary by state. Providers must make sure all needed documents are complete and correct. This helps avoid coverage denials.
| State | Coverage Policy | Required Prior Treatments | Documentation Standards |
| California | Covers PET scans for cancer diagnosis | Biopsy or CT scan | Detailed medical records, physician justification |
| New York | Covers PET scans for neurological disorders | MRI or EEG | Comprehensive treatment history, specialist referral |
| Texas | Covers PET scans for cancer staging | CT scan or MRI | Physician order, relevant medical history |
Healthcare providers need to keep up with their state’s Medicaid PET scan rules. This ensures they follow the rules and help patients get the care they need.
Private Insurance PET Scan Coverage Policies
Private insurers have different rules for PET scan coverage. This affects how patients get access to these scans. It’s important for healthcare providers and patients to understand these rules.
Differences Among Major Insurers
Big private insurers have different rules for PET scans. Some may cover scans for cancer staging, while others might not. This can really affect patient care and treatment plans.
In-Network vs. Out-of-Network Considerations
Being in-network or out-of-network matters a lot for PET scan coverage. In-network providers usually have deals with insurers, so patients pay less. Out-of-network providers might charge more, making costs higher for patients.
Patients should know if their insurance covers in-network or out-of-network care. Healthcare providers can help by talking about these options.
Policy Exclusions to Watch For
Private insurance policies often have exclusions that can affect PET scan coverage. These might include things like experimental treatments or cosmetic procedures. Knowing these exclusions can help avoid surprises.
Patients and healthcare providers should check insurance policies for exclusions. This can help avoid problems with coverage and make sure patients get the care they need.
Experimental or Investigational Classification
It’s important to know how insurers decide if PET scans are experimental or investigational. This affects insurance coverage and who can get these scans. It’s key for both patients and healthcare providers.
How Insurers Determine “Experimental” Status
Insurers check if PET scans are experimental or not. They look at clinical evidence, guidelines, and their own policies. They review data and research to see if the scan works well for certain health issues.
Criteria Used for Determination
The criteria for deciding if a PET scan is experimental include:
- Clinical trial results and evidence-based medicine
- Guidelines from professional medical organizations
- Technology assessments and health outcomes research
- Peer-reviewed literature and expert opinions
Table: Factors Influencing Experimental Classification
| Factor | Description | Impact on Classification |
| Clinical Evidence | Results from clinical trials and observational studies | Strong evidence supports non-experimental status |
| Professional Guidelines | Recommendations from medical societies and organizations | Guideline endorsement supports medical necessity |
| Technology Assessments | Evaluations of the technology’s efficacy and safety | Positive assessments support coverage |
Clinical Trial Coverage Options
If a PET scan is seen as experimental, there might be a way to get it through clinical trials. Insurers might cover it if the trial is relevant to the patient’s condition. This can help patients get scans that might not be approved yet.
“Coverage for PET scans in clinical trials can be a critical option for patients who may benefit from these diagnostic tools, even if they are not yet widely approved for standard use.”
” Expert in Medical Imaging
Emerging PET Applications Often Denied
New PET scan uses that don’t have a lot of evidence are often not covered by insurers. These might be new ways to use PET scans or for conditions not yet proven. Patients and doctors have to deal with the denial process or find other ways to diagnose.
Cost Considerations and Utilization Management
Understanding the cost of PET scans is key for good healthcare management. These scans are very useful for diagnosis but can be pricey. This affects insurance and how patients get access to them.
Cost-Effectiveness Evaluations by Insurers
Insurers check how cost-effective PET scans are. They look at how accurate they are, how they affect treatment, and patient outcomes. They compare this to other imaging options.
Cost-effectiveness is important for insurance coverage of PET scans. Insurers use this info to decide what to cover and how to keep costs down.
Utilization Management Strategies
Insurers use strategies to manage PET scan use and costs. These include needing approval before a scan, limiting how often scans can be done, and following certain treatment steps.
Prior authorization is a common strategy. It means doctors need approval from the insurer before doing a PET scan. This helps make sure scans are used right and follow the best guidelines.
Specialist Referral and Consultation Requirements
Getting a specialist referral is key to getting a PET scan covered by insurance. Insurance companies need a specialist’s say-so to approve advanced tests like PET scans.
Oncologist Recommendations
For cancer diagnosis or treatment, oncologists often have to give their okay for PET scans. They look at the patient’s health and decide if a PET scan is needed for treatment planning.
- Oncologists check the patient’s medical history and current health.
- They figure out if a PET scan is needed for diagnosis or tracking treatment.
- Their advice comes from proven guidelines and their own experience.
Multidisciplinary Team Input
For complex cases, a team of specialists is often needed. This team might include oncologists, radiologists, and surgeons.
The team’s input is valuable because it:
- Looks at the patient’s condition fully.
- Helps decide if a PET scan is right.
- Creates a treatment plan that fits the patient.
Tumor Board Recommendations
Tumor boards are groups of experts who discuss tough cases. They help decide the best tests and treatments, including PET scans.
Tumor board recommendations can:
- Confirm the need for PET scans based on guidelines.
- Give a united view on the best care for the patient.
- Guide through the insurance process.
Appealing a PET Scan Denial
Appealing a PET scan denial means knowing the steps and what documents are needed. If an insurance company says no to a PET scan, you and your doctor can appeal. This is your chance to show why the scan is really needed.
Initial Appeal Process Steps
The first step is to ask the insurance company to look at it again. This is key because it lets them see more information. This might change their mind about saying no.
- Read the denial letter to know why they said no.
- Get all your medical records and documents ready.
- Send in a formal appeal with your documents.
Documentation to Include in Appeals
Documents are very important when you appeal. You need to show why the PET scan is needed for your health.
| Documentation Type | Description | Importance |
| Medical Records | Your medical history, diagnosis, and treatment plans. | High |
| Physician’s Letter | A detailed letter from your doctor on why the PET scan is needed. | High |
| Clinical Guidelines | References to guidelines that support using PET scans. | Medium |
Second-Level and External Appeals
If the first appeal is turned down, you can try again. Second-level appeals are done by the insurance company itself. External appeals go to independent groups for a fair review.
Knowing about all the appeal levels and what each needs can really help. It can make your appeal more likely to succeed.
Working with Your Healthcare Provider
Learning how to work with your healthcare provider can greatly help in getting a PET scan approved. They are not just medical experts but also your advocate. They help you through the insurance approval process.
Advocating for Approval
Your healthcare provider plays a key role in getting a PET scan approved. They first check if the scan is medically necessary based on your health and history. Documentation is key, and they must submit all needed medical records.
They also need to talk clearly with the insurance company. They explain why the PET scan is needed, showing it fits with medical guidelines and your health needs.
Peer-to-Peer Reviews
If the insurance denies the scan, a peer-to-peer review can help. This is a direct talk between your doctor and the insurance’s medical expert. They discuss the scan’s medical need and any insurance concerns.
This review lets your doctor fully explain the scan’s importance. It’s a chance for both sides to understand each other better.
Alternative Diagnostic Pathways
If the PET scan is denied, your doctor might look into other tests. This could be CT scans or MRI, depending on your condition and what’s needed for diagnosis or treatment.
| Diagnostic Test | Typical Use | Insurance Considerations |
| PET Scan | Cancer staging, neurological disorders | Often requires prior authorization |
| CT Scan | Trauma, cancer, vascular diseases | Generally covered, but may have limitations |
| MRI | Soft tissue injuries, neurological conditions | May require prior authorization for certain conditions |
By teaming up with your healthcare provider, you can better handle diagnostic tests and insurance approvals. Whether it’s fighting for a PET scan or looking at other tests, your doctor is a vital partner in your health care.
Conclusion
Insurance denials for PET scans are complex, influenced by many factors. These include medical necessity, documentation, and coverage policies. It’s important for healthcare providers, patients, and insurers to understand these reasons.
Common reasons for denials include missing documentation, preferring other imaging, and limits on how often scans can be done. Knowing the appeals process and how healthcare providers can help is key. This way, patients can get the care they need.
Getting insurance to cover PET scans requires a deep understanding of many things. This includes medical need, policy rules, and doctor’s opinions. This article aims to help readers understand these complexities. It’s all about getting the right care through insurance.
FAQ
Why does insurance deny a PET scan?
Insurance companies deny PET scans for many reasons. These include if the scan is not medically necessary, if it’s for experimental use, or if the documentation is not enough.
What is considered “medically necessary” for a PET scan?
Insurers check if a PET scan is needed based on guidelines and the patient’s condition. This includes for cancer staging, checking how well treatments work, and some neurological issues.
What documentation is required to support a PET scan claim?
To support a PET scan claim, you need certain medical records. These include the patient’s diagnosis, treatment plan, and medical history. Also, a doctor’s note explaining why the scan is needed.
Can insurance companies deny a PET scan if alternative imaging modalities are available?
Yes, they might. Insurance companies often prefer other scans like CT and MRI for some conditions. This could mean they deny PET scans for those cases.
How do insurers determine the experimental or investigational status of a PET scan?
Insurers look at clinical evidence and guidelines to decide if a PET scan is experimental or investigational. This affects coverage for new or untested uses of the scan.
What are the frequency limitations for PET scans under insurance coverage?
Insurance companies might limit how often PET scans can be done. This could mean they deny scans if they’re done too soon after another one.
How does Medicare coverage for PET scans differ from private insurance?
Medicare has clear rules for when PET scans are covered, like for cancer diagnosis and treatment. But private insurance can vary a lot between different companies.
Can Medicaid coverage for PET scans vary by state?
Yes, Medicaid coverage for PET scans can change a lot from state to state. Each state has its own rules and requirements for coverage.
What is the appeals process for a denied PET scan claim?
If a PET scan claim is denied, you can appeal. You’ll need to provide detailed medical information and evidence to show why the scan is necessary. There are several levels of appeal you can try.
What are the average costs of PET scans, and how do insurers evaluate cost-effectiveness?
The cost of PET scans can vary a lot. It depends on the reason for the scan, where it’s done, and other factors. Insurers look at these costs to decide if the scan is worth covering, based on its value in different situations.
References
- Diagnostic Imaging Staff. (2012, April 25). Report: Most imaging insurance denials are due to prior authorization. Diagnostic Imaging. Retrieved from https://www.diagnosticimaging.com/view/report-most-imaging-insurance-denials-due-prior-authorization Diagnostic Imaging
- “Patterns of Unnecessary Insurer Prior Authorization Denials in a Complex Surgical Oncology Practice. (2022). Journal Article (PubMed). Retrieved from https://pubmed.ncbi.nlm.nih.gov/37037166/
- Coffta, S. (2016, October 6). How to avoid radiology claim denials: Medical necessity. AuntMinnie Practice Management. Retrieved fromhttps://www.auntminnie.com/practice-management/administration/economics/article/15615879/how-to-avoid-radiology-claim-denials-medical-necessity