
We are seeing big steps forward in cancer treatment, thanks to internal radiotherapy, or brachytherapy. This method puts radioactive materials right into or near the tumor. It lets doctors give high doses of radiation to cancer cells without harming nearby healthy tissues.Understand internal radiotherapy treatment, key isotopes, and cancer therapy approaches for improved outcomes.
Hospitals like Liv Hospital are using radioactive isotopes to make cancer care safer and more effective. They focus on what’s best for the patient and follow global standards. This helps them offer top-notch care to people from all over the world.
Key Takeaways
- Internal radiotherapy treatment precisely targets cancer cells, sparing healthy tissues.
- Radioactive materials are used to deliver high doses of radiation directly to tumors.
- This technique minimizes exposure to surrounding healthy tissues, reducing side effects.
- Hospitals like Liv Hospital are at the forefront of delivering advanced cancer care.
- The focus is on patient-centered outcomes and global standards in cancer treatment.
The Fundamental Principles of Internal Radiotherapy Treatment
Internal radiotherapy is a complex cancer treatment. It uses radioactive materials to kill cancer cells. This method sends radiation directly to the tumor, protecting healthy tissues nearby.
Definition and Core Mechanisms
Internal radiotherapy, also known as brachytherapy, places radioactive materials close to the tumor. This method delivers a high dose of radiation locally. It makes the treatment more effective and reduces side effects.
Small radioactive sources, like seeds or capsules, are used in this treatment. These sources emit radiation that kills cancer cells. The choice of radioactive material depends on the cancer type, location, and stage.
How Radioactive Materials Target Cancer Cells
Radioactive materials in internal radiotherapy target specific cancer cells. For example, iodine-131 is used for thyroid cancer because the thyroid gland naturally takes up iodine. Other isotopes, like lutetium-177 and radium-223, are used for different types of cancer.
These radioactive substances are given through various methods, such as intravenous injection or direct implantation. Once in the body, they go to the cancer cells. There, they emit radiation that damages the DNA of the cancer cells, stopping them from growing and dividing.
| Method | Description | Common Applications |
| Intravenous Radiotherapy | Administration of radioactive substances through a vein. | Thyroid cancer, neuroendocrine tumors. |
| Interstitial Implantation | Direct placement of radioactive sources into or near tumors. | Prostate cancer, breast cancer. |
| Cavity Insertion | Placement of radioactive materials into body cavities. | Gynecological cancers, certain types of brain tumors. |
Key Fact 1: How Internal Radiotherapy Treatment Works
Internal radiotherapy sends radiation straight to cancer spots, protecting healthy tissues nearby. This method is a big step forward in fighting cancer. It means treatments can be more focused and have fewer side effects.
Radiation Delivery Directly to Cancer Sites
Internal radiotherapy puts a radioactive source inside or close to the tumor. This way, the radiation hits the tumor right on, with less harm to other tissues. We use implants, capsules, or liquids with radioactive isotopes to do this.
Key benefits of this approach include:
- High doses of radiation can be delivered directly to the tumor.
- Damage to surrounding healthy tissues is minimized.
- Treatment is highly localized, reducing systemic side effects.
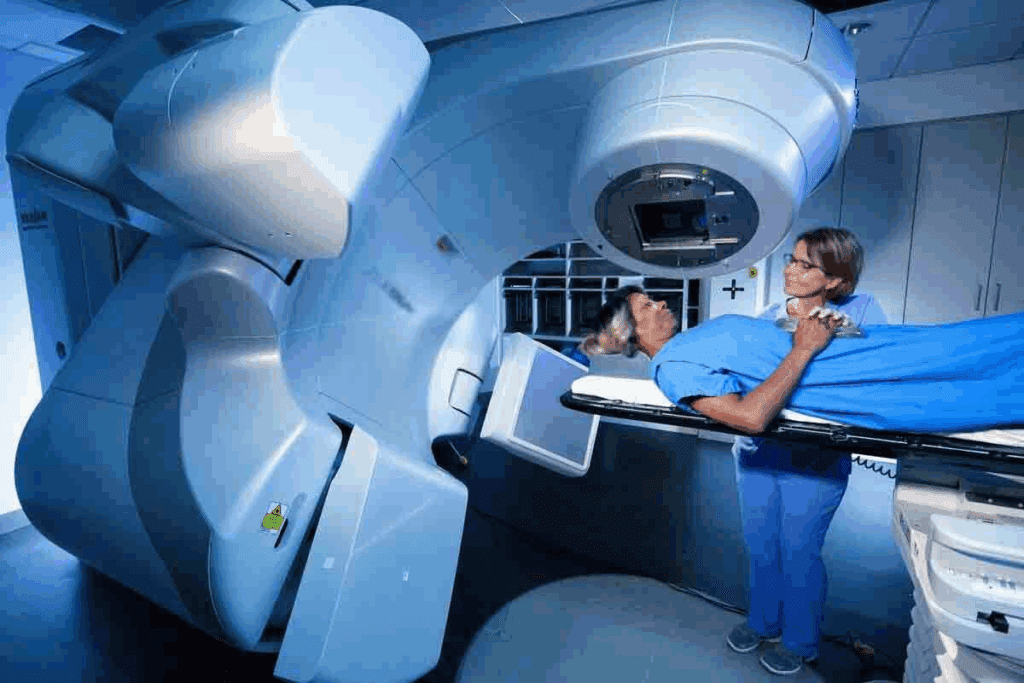
Differences Between Internal and External Radiation
It’s important to know how internal and external radiation therapy differ. External beam radiation therapy (EBRT) sends radiation from outside the body to the tumor. Internal radiotherapy, on the other hand, puts the radioactive material inside or near the tumor.
| Characteristics | Internal Radiotherapy | External Beam Radiation Therapy |
| Radiation Source | Placed inside or near the tumor | Machine outside the body |
| Radiation Dose | Highly localized, high dose to tumor | Variable dose, depending on tumor depth and location |
| Side Effects | Generally fewer systemic side effects | May cause more systemic side effects due to radiation exposure to larger areas |
Internal radiotherapy delivers radiation directly to cancer sites. This makes it a precise and effective treatment for many cancers. It not only improves treatment results but also helps patients by lowering the risk of side effects from widespread radiation.
Key Fact 2: Major Types of Internal Radiotherapy Delivery Methods
Internal radiotherapy uses different methods to treat cancer. Each method is chosen based on the cancer type and the patient’s health. The goal is to find the best way to fight cancer.
We use many ways to give internal radiotherapy. This shows how cancer is different and how we need to treat each case differently. We use intravenous radiotherapy, interstitial implantation, and cavity insertions, among others.
Intravenous Radiotherapy Administration
Intravenous radiotherapy puts radioactive substances into the bloodstream. This method is good for cancers that have spread or are everywhere in the body.
Liquid radiation treatment is a type of intravenous radiotherapy. It uses a liquid form of radioactive material. This is often used for thyroid cancer, where it targets thyroid cells.
Interstitial Implantation Techniques
Interstitial implantation puts small radioactive sources into or near the tumor. This method gives a high dose of radiation to the tumor. It helps protect healthy tissues around it.
| Treatment Type | Description | Cancer Types |
| Interstitial Implantation | Radioactive sources are placed directly into or near the tumor | Prostate, breast, and other localized cancers |
| Intravenous Radiotherapy | Radioactive substances administered into the bloodstream | Thyroid, certain types of lymphoma |
| Cavity Insertions | Radioactive material placed into body cavities | Gynecological, certain gastrointestinal cancers |
Cavity Insertions and Specialized Approaches
Cavity insertions put radioactive material into body cavities like the uterus or vagina. This method is used for gynecological cancers. It can be very effective when used with other treatments.
“The precision and flexibility of internal radiotherapy delivery methods have significantly improved cancer treatment outcomes, giving new hope to patients worldwide.”
— Senior Oncologist
In conclusion, there are many ways to deliver internal radiotherapy. Each method is chosen based on the cancer type and the patient’s health. This helps doctors create treatment plans that work best for each patient, improving radioisotope treatment results.
Key Fact #3: Essential Isotopes Used in Cancer Therapy
Certain radioactive isotopes are key in cancer treatment. They target cancer cells, reducing harm to healthy tissues. This makes them vital in fighting cancer.
Iodine-131 for Thyroid Cancer Treatment
Iodine-131 is a top choice for thyroid cancer treatment. The thyroid gland absorbs iodine, making Iodine-131 effective. This targeted approach helps destroy cancer cells while protecting other tissues.
A leading oncologist says, “Iodine-131 therapy is a cornerstone in thyroid cancer treatment. It’s very effective in managing the disease.”
“The use of Iodine-131 in thyroid cancer represents one of the earliest and most successful applications of targeted radioactive therapy.”
Lutetium-177 Applications in Neuroendocrine Tumors
Lutetium-177 (Lu-177) dotatate treats neuroendocrine tumors (NETs). It binds to somatostatin receptors on NET cells. This specificity makes Lu-177 dotatate a targeted therapy, improving outcomes for patients with advanced NETs.
| Isotope | Application | Targeted Cancer Type |
| Iodine-131 | Thyroid Cancer Treatment | Thyroid Cancer |
| Lutetium-177 | Neuroendocrine Tumor Treatment | Neuroendocrine Tumors |
| Radium-223 | Bone Metastases Management | Prostate Cancer with Bone Metastases |
| Yttrium-90 | Liver Cancer Treatment | Liver Cancer |
Radium-223 for Bone Metastases Management
Radium-223 dichloride treats prostate cancer that has spread to the bone. It emits alpha particles that kill cancer cells in the bone. This improves survival and quality of life for patients with advanced prostate cancer.
Yttrium-90 Microsphere Therapy for Liver Cancer
Yttrium-90 microsphere therapy delivers Yttrium-90 to liver tumors via the hepatic artery. The microspheres target the tumor, sparing normal liver tissue. This method is great for treating liver cancer that can’t be removed surgically.
These isotopes are big steps forward in cancer treatment. They offer targeted and effective treatments for different cancers. Knowing how each isotope works helps doctors give patients better care.
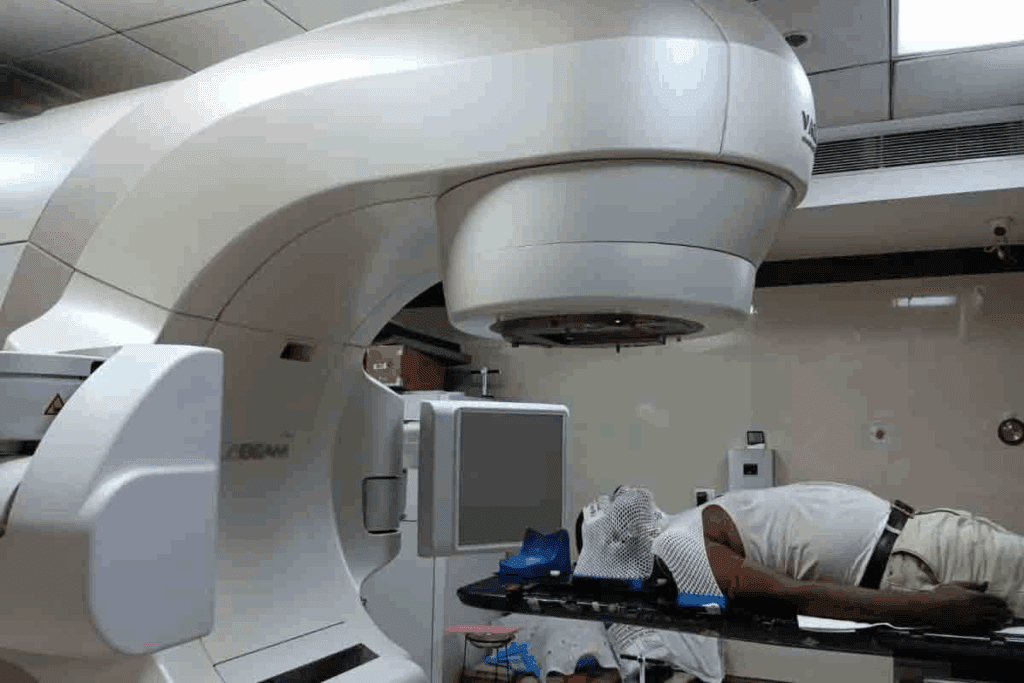
Key Fact 4: Brachytherapy as Precision-Targeted Radiation
Brachytherapy is a key cancer treatment that targets tumors with precision. It delivers high doses of radiation right to the tumor, protecting healthy tissues. We’ll look at how it works, its methods, and the types of implants used. This highlights its role in treating tumors with great accuracy.
High-Dose Rate vs. Low-Dose Rate Approaches
Brachytherapy comes in two main types: High-Dose Rate (HDR) and Low-Dose Rate (LDR). High-Dose Rate (HDR) brachytherapy gives a high dose of radiation in a short time, often in one session. It’s good for tumors that are easy to reach and need quick treatment.
Low-Dose Rate (LDR) brachytherapy sends out radiation slowly over days. It’s often used for prostate cancer, where tiny radioactive seeds are left in the body to slowly release radiation.
| Characteristics | High-Dose Rate (HDR) | Low-Dose Rate (LDR) |
| Radiation Delivery | High dose over a short period | Continuous low dose over several days |
| Typical Applications | Accessible tumors, various cancer types | Prostate cancer, certain other localized tumors |
| Implant Duration | Temporary | Permanent or temporary |
Permanent vs. Temporary Implants
Brachytherapy implants can be permanent or temporary. Permanent implants, used in LDR, place small radioactive seeds in or near the tumor. These seeds slowly release radiation and then stop.
Temporary implants are used in HDR and some LDR treatments. They involve placing a radioactive source in the tumor for a set time before it’s removed. This method gives precise control over the radiation.
“Brachytherapy offers a highly targeted approach to cancer treatment, minimizing damage to surrounding tissues and reducing side effects.”
— Expert in Radiation Oncology
Brachytherapy’s precision is a big plus. It treats tumors well while keeping patients’ quality of life high.
Key Fact 5: Liquid Radiation and Intravenous Therapy Applications
Liquid radiation therapy is a big step forward in cancer treatment. It uses radioactive substances in a form that can be dissolved. This method sends radiation straight to cancer cells, reducing harm to healthy tissues nearby.
How Soluble Radioactive Substances Work
Soluble radioactive substances are given through an IV. They move through the blood and find cancer cells. These substances kill cancer cells by damaging their DNA, stopping them from growing and dividing.
Key characteristics of soluble radioactive substances include:
- High specificity for cancer cells
- Ability to reach tumors in hard-to-access areas
- Minimal side effects compared to traditional chemotherapy
Administration Procedures and Patient Experience
Getting liquid radiation therapy involves an IV injection. Patients might feel tired or nauseous, but these effects are usually short-lived and not severe.
Patient preparation is key for treatment success. This includes a full medical check-up, talking about possible side effects, and advice on what to do after treatment.
| Procedure | Description | Patient Experience |
| Pre-treatment evaluation | Comprehensive medical check-up | Discussion of treatment expectations |
| Administration of radioactive substance | Intravenous injection | Mild discomfort at injection site |
| Post-treatment care | Monitoring for side effects | Guidance on managing side effects |
Targeting Hard-to-Reach Cancers
Liquid radiation therapy is great for cancers that are hard to get to. It uses substances that can dissolve and target tumors in places surgery or external radiation can’t reach. This gives hope to patients with tough cases.
As we keep improving in nuclear medicine, liquid radiation therapy is a standout. It can target cancer cells well while protecting healthy tissues. This makes it a powerful tool in our fight against cancer.
Key Fact 6: Cancer Types Effectively Treated with Radioisotope Therapy
Radioisotope therapy is a key treatment for many cancers. It has improved outcomes for prostate, thyroid, and blood diseases. We’ll look at cancers that radioisotope therapy can treat well.
Thyroid Cancer Management
Thyroid cancer is often treated with radioisotope therapy. Iodine-131 is used because the thyroid takes it up. This method kills thyroid cancer cells without harming other tissues.
Prostate Cancer Treatment Options
Radioisotope therapy has made a big difference in prostate cancer treatment. Radium-223 helps those with bone metastasis by easing pain and improving life quality. It’s a big help for advanced cases.
Blood Cancers and Targeted Approaches
Blood cancers like leukemia and lymphoma can be treated with radioisotope therapy. Radioimmunotherapy uses antibodies to find and kill cancer cells. It’s a precise way to target tumors.
Liver and Neuroendocrine Tumor Applications
Liver cancer and neuroendocrine tumors also benefit from radioisotope therapy. Yttrium-90 microspheres target liver tumors. Lutetium-177 is good for neuroendocrine tumors, hitting cancer cells while protecting healthy tissue.
| Cancer Type | Radioisotope Used | Treatment Benefits |
| Thyroid Cancer | Iodine-131 | Targeted destruction of thyroid cancer cells |
| Prostate Cancer | Radium-223 | Pain relief and improved quality of life |
| Blood Cancers | Radioimmunotherapy | Direct delivery of radiation to tumor sites |
| Liver Cancer | Yttrium-90 microspheres | Localized radiation to liver tumors |
| Neuroendocrine Tumors | Lutetium-177 | Targeted treatment with minimal damage to healthy tissue |
Radioisotope therapy is versatile and effective for many cancers. As research goes on, we’ll see more progress. This gives hope to patients all over the world.
Key Fact 7: Recent Advances in Radioisotope Cancer Treatment
The world of cancer treatment is evolving with new radioisotope therapies. These recent advances have greatly improved how we treat cancer. Now, treatments are less invasive and more targeted.
Less Invasive Treatment Innovations
New treatments use advanced radioisotopes that target cancer sites precisely. This reduces harm to healthy tissues. Early trials show patients have fewer side effects and recover faster.
Enhanced Targeting Technologies
New technologies help radioactive materials reach tumors more accurately. Ligand-based targeting is a key method. It promises to make radioisotope therapy even more precise.
Improved Outcomes in Previously Challenging Cancers
These breakthroughs have brought hope to patients with hard-to-treat cancers. Radioisotope therapy is now effective against some neuroendocrine tumors and prostate cancer.
| Advance | Description | Benefit |
| Less Invasive Treatments | Precise targeting of cancer sites | Reduced damage to healthy tissues |
| Enhanced Targeting Technologies | Accurate delivery of radioactive materials | Improved treatment efficacy |
| Improved Outcomes | Effective treatment of challenging cancers | New hope for patients |
Side Effects and Management in Internal Radiotherapy
It’s important to know about the side effects of internal radiotherapy. This treatment uses radioactive materials placed inside or near tumors. It can harm both cancer cells and healthy tissues.
Common Side Effects by Treatment Type
The side effects of internal radiotherapy depend on the treatment type, where the radioactive material is placed, and the dose. For example:
- Fatigue: Many people feel tired because their bodies react to the radiation.
- Nausea and Vomiting: These happen more often if the treatment area is near the stomach or if certain isotopes are used.
- Local Reactions: Skin irritation can occur if the radioactive material is near the skin or in cavities.
Strategies for Managing Complications
Managing side effects of internal radiotherapy needs a detailed plan. Here are some strategies:
- Personalized Care Plans: Treatments and care plans are customized based on the individual’s health and needs.
- Medication: Medicines help with symptoms like nausea or pain.
- Dietary Adjustments: Changing diets can help with side effects like nausea or diarrhea.
- Rest and Recovery: Getting enough rest helps fight fatigue.
Long-term Considerations
Some side effects can last a long time or even be permanent. It’s key to know about these long-term effects, including:
- Risk of Secondary Cancers: There’s a small chance of getting secondary cancers from radiation.
- Organ Damage: Radiation can harm certain organs over time, depending on the location and dose.
- Hormonal Changes: Treatments that affect endocrine glands can cause hormonal imbalances.
Understanding these points helps patients and doctors work together. This way, they can reduce risks and get the most benefits from internal radiotherapy.
Patient Selection Criteria for Radioisotope Therapy
Choosing the right patients for radioisotope therapy is key to its success. This therapy uses radioactive materials to fight cancer. It works best for certain types and stages of cancer.
Determining Suitable Candidates
We pick patients for radioisotope therapy based on several things. These include the cancer type and stage, and the patient’s health. For example, those with thyroid cancer might get Iodine-131 therapy because the thyroid gland absorbs iodine.
The assessment process involves:
- Evaluating the cancer type and its response to radioisotope therapy
- Checking the cancer stage to see if therapy can help
- Looking at the patient’s health and recovery chances
| Factor | Description | Importance Level |
| Cancer Type | Type of cancer being treated | High |
| Cancer Stage | Stage of cancer progression | High |
| Overall Health | Patient’s general health condition | Medium |
Contraindications and Risk Assessment
Some conditions make radioisotope therapy not suitable. Pregnancy is a big no because it could harm the baby. We also think about the risk of radiation to others, like young kids or breastfeeding moms.
“Careful patient selection is the cornerstone of successful radioisotope therapy,” says a leading oncologist.
Radiation Safety and Post-Treatment Protocols
Keeping safe from radiation is very important for patients and their caregivers after radioisotope therapy. This treatment uses radioactive materials to fight cancer. But it’s also important to handle it carefully to protect others from radiation.
Precautions for Patients and Caregivers
Patients and caregivers need to take steps to lower radiation exposure after treatment. Following the advice of healthcare professionals is key to staying safe. They might need to:
- Stay away from others, like kids and pregnant women, for a while.
- Not share things like utensils, towels, or clothes.
- Use separate bathrooms and flush the toilet a few times after use.
Doctors say, “Keeping safe from radiation is not just for the patient. It’s also for those around them.” These steps can greatly reduce the risk of radiation exposure.
Monitoring and Follow-up Requirements
After treatment, it’s important to keep an eye on how well it’s working and watch for side effects. Patients must go to their follow-up appointments as their doctor says. These visits might include:
- Physical checks to see how the patient is doing.
- Imaging tests to see how the cancer is responding.
- Lab tests to check radiation levels and other health signs.
“The success of treatment depends on more than just the therapy,” experts say. “It also depends on careful monitoring and follow-up care.”
By following these steps and talking openly with doctors, patients can have a better recovery. This helps to reduce risks from radiation.
Conclusion: The Evolving Landscape of Internal Radiotherapy
Internal radiotherapy is key in fighting cancer, thanks to new tech in nuclear medicine and radiation therapy. Studies show MRI use in brachytherapy planning has grown a lot. It went from 11% in 2015 to 32% in 2020, as seen in a study on PubMed.
New tools and methods are making internal radiotherapy better. This includes hybrid applicators and interstitial brachytherapy. These help treat more cancers, like prostate, thyroid, and liver cancers.
Looking ahead, internal radiotherapy will keep getting better. It will aim to make treatments more effective and less harsh. Using radioisotopes and radioactive treatments will be important for future cancer care.
We’ll see more breakthroughs in internal radiotherapy soon. This will make cancer treatments more precise and effective. This means better results for patients.
FAQ
What is internal radiotherapy treatment?
Internal radiotherapy, also known as brachytherapy, is a treatment. It places radioactive materials close to the tumor. This delivers high doses of radiation to cancer cells while protecting healthy tissues.
How does internal radiotherapy treatment work?
It works by targeting cancer sites with radiation. This method allows for precise treatment of tumors. It also reduces damage to healthy tissues nearby.
What are the different types of internal radiotherapy delivery methods?
There are several delivery methods. These include intravenous administration, interstitial implantation, and cavity insertions. Each method is used for different types of cancers.
What isotopes are commonly used in cancer therapy?
Common isotopes include Iodine-131 for thyroid cancer. Lutetium-177 is used for neuroendocrine tumors. Radium-223 treats bone metastases. Yttrium-90 is used for liver cancer.
What is brachytherapy and how does it work?
Brachytherapy is a precise radiation therapy. It involves placing radioactive materials near the tumor. This delivers high doses of radiation to cancer cells.
What is the difference between high-dose rate and low-dose rate brachytherapy?
High-dose rate brachytherapy uses a higher dose rate for a shorter time. Low-dose rate brachytherapy uses a lower dose rate for a longer time.
What is liquid radiation therapy?
Liquid radiation therapy involves giving radioactive substances intravenously. It targets cancer cells, making it useful for hard-to-reach cancers.
What types of cancer are effectively treated with radioisotope therapy?
It treats various cancers. These include thyroid, prostate, blood cancers, liver cancer, and neuroendocrine tumors.
What are the side effects of internal radiotherapy?
Side effects vary by treatment type. They can include fatigue, nausea, and localized reactions. These can be managed with proper strategies.
How are patients selected for radioisotope therapy?
Patients are chosen based on their cancer type, medical history, and health. Contraindications and risk assessments are considered.
What precautions should patients take after undergoing radioisotope therapy?
Patients should follow radiation safety guidelines and post-treatment protocols. This minimizes exposure to others and ensures safe recovery.
What are the recent advances in radioisotope cancer treatment?
Recent advances include less invasive treatments and improved targeting technologies. These offer new hope for patients with challenging cancers.
References:
- Traub-Weidinger T, Lonsdale MN, Gil-Nagel A, et al. EANM practice guidelines for an appropriate use of PET and SPECT in epilepsy. Eur J Nucl Med Mol Imaging. 2024;51(5):1261-1280. https://pmc.ncbi.nlm.nih.gov/articles/PMC11139752/
- Ponisio MR, McConathy J. The Role of SPECT and PET in Epilepsy. AJR Am J Roentgenol. 2021;216(1):186-195. https://doi.org/10.2214/AJR.20.23336
- Baradaran-Salimi K, Wielepp T, Wiest R, et al. Brain perfusion SPECT in the presurgical evaluation of drug-resistant epilepsy: Estimating the rate of high-confidence seizure onset zone candidates. Epilepsy Res. 2024;205:107432. https://pmc.ncbi.nlm.nih.gov/articles/PMC11393367/










