Last Updated on November 26, 2025 by Bilal Hasdemir

We are seeing big changes in how we treat cancer, thanks to interventional oncologists. These doctors use new imaging tech to do precise, small procedures. They help find and treat cancer in new ways, making treatments better and faster. What is an interventional oncologist? The ultimate guide to this specialty, explaining the powerful treatments and therapies they perform.
At Liv Hospital, we mix global expertise with new healthcare ideas. We offer interventional oncology solutions that are safer, quicker, and more accurate. Our team works hard to give top-notch care and support to patients from around the world.
Key Takeaways
- Cancer care is being transformed by interventional oncologists using minimally invasive procedures.
- Advanced imaging techniques enable targeted treatments with fewer side effects.
- Liv Hospital offers innovative interventional oncology solutions with international expertise.
- Patients benefit from less invasive treatments and faster recovery times.
- Comprehensive support and guidance are provided for international patients.
The Role and Expertise of an Interventional Oncologist

Interventional oncologists lead in cancer treatment. They use their special training to target tumors directly. This method lowers the risk of problems and helps patients recover faster.
Definition and Specialized Training
Interventional oncology is seen as a key part of cancer care. It joins medical, surgical, and radiation oncology. These doctors get deep training for doing small, precise procedures.
- They learn to use advanced imaging like CT, MRI, and ultrasound.
- They perform minimally invasive treatments to hit tumors right on.
- They understand cancer well and keep up with new treatments.
Diagnostic and Treatment Capabilities
Interventional oncologists are great at both finding and treating tumors. They use top-notch imaging to guide their treatments. This makes their treatments both precise and effective.
- Image-guided tumor ablations: They use methods like RFA and microwave ablation to kill cancer cells.
- Embolization procedures: They use TACE and Y90 to block tumors’ blood supply.
- Targeted drug delivery: They send chemotherapy or other drugs straight to the tumor.
Interventional Oncology: The Fourth Pillar of Cancer Care
Interventional oncology is now a key part of cancer treatment. It offers minimally invasive procedures that help patients. It uses interventional radiology to diagnose, treat, and manage cancer-related issues.
Evolution and Recognition in Cancer Treatment
Interventional oncology has grown a lot over time. It has become a unique field in oncology. This growth is thanks to new technology and techniques that make treatments better and more precise.
We see interventional oncology as the fourth main part of cancer care. It works with medical, surgical, and radiation oncology. Together, they make cancer treatment better and more effective for patients.
Integration with Medical, Surgical, and Radiation Oncology
Integrating interventional oncology with other cancer treatments has been a big step forward. It combines with medical, surgical, and radiation oncology. This way, doctors can create treatment plans that fit each patient’s needs.
This teamwork means patients get the best treatment. It could be through small procedures or a mix of treatments.
The table below shows what interventional oncology does and how it works with other treatments:
| Treatment Modality | Role in Cancer Care | Benefits |
| Interventional Oncology | Minimally invasive procedures for diagnosis and treatment | Reduced recovery time, fewer complications |
| Medical Oncology | Systemic treatments such as chemotherapy and immunotherapy | Targets cancer cells throughout the body |
| Surgical Oncology | Surgical removal of tumors and affected tissues | Potential for curative resection |
| Radiation Oncology | High-energy radiation to kill cancer cells | Precise targeting of tumors |
Knowing what each treatment does helps doctors make plans that work best for each patient. This way, patients get the best care possible.
Advanced Imaging Technologies Used by Interventional Oncologists
Interventional oncologists use advanced imaging to see tumors clearly. This lets them target treatments with great accuracy. These technologies give us detailed views of tumors and how they respond to treatment in real-time. This makes treating cancer more effective.
CT, MRI, and Ultrasound Guidance Systems
Interventional oncologists use CT, MRI, and ultrasound to guide procedures. These tools help us:
- Find tumors accurately and see their size and shape
- Guide tools to the right spot with precision
- Watch the treatment area live, making changes as needed
Real-Time Visualization During Procedures
Seeing things in real-time is key in interventional oncology. It lets us:
- See how treatment affects the tumor right away
- Adjust the treatment to get better results
- Protect healthy tissues from damage
Advanced imaging has changed interventional oncology for the better. It makes treatments more precise and effective. Here’s a table that shows what each technology offers:
| Imaging Modality | Key Features | Benefits |
| CT Guidance | High-resolution images, excellent for soft tissue visualization | Precise tumor localization, effective for complex procedures |
| MRI Guidance | Superior soft tissue contrast, real-time imaging capabilities | Enhanced visualization of tumor boundaries, reduced risk of complications |
| Ultrasound Guidance | Real-time imaging, portable, and cost-effective | Quick and accurate guidance, useful for bedside procedures |
By using these advanced imaging tools, we can greatly improve cancer treatment. This means better and less invasive options for patients.
Minimally Invasive Procedures: Benefits and Outcomes
The field of interventional oncology is moving towards less invasive methods. This change helps patients recover faster and lowers the risk of complications. These new methods use advanced imaging to treat cancer with great precision and little harm to the body.
Reduced Recovery Time and Hospital Stays
Minimally invasive procedures are a big win for patients. They need less time to recover and stay in the hospital. This is because they use smaller cuts, causing less damage and pain.
For example, thermal ablation and embolization are done through tiny holes or tubes. This means patients don’t have to stay in the hospital for as long. It makes patients happier and saves money on healthcare.
Fewer Complications Compared to Traditional Surgery
These new procedures also have fewer side effects than old-school surgery. They avoid big cuts, which lowers the chance of infections and other problems. Doctors use live images to guide the treatment, making it more accurate.
- Reduced risk of infection
- Less blood loss during procedures
- Lower risk of damage to surrounding tissues
Companies like Boston Scientific lead in making new tech for these treatments. This makes them safer and more effective.
Quality of Life Improvements for Cancer Patients
Minimally invasive procedures greatly improve life for cancer patients. They cause less harm than traditional surgery, helping patients stay strong and recover faster.
Also, these treatments can be done outside the hospital. This lets patients spend more time with their loved ones at home. It makes a big difference in their well-being during tough times.
As interventional oncology keeps growing, we can expect even better results. New techniques and tools will likely lead to better survival rates and quality of life for patients.
Essential Interventional Oncology Treatments and Therapies
Interventional oncology is key in cancer treatment, bringing new therapies. We use different treatments for solid tumors in organs like the liver, lungs, and kidneys. These methods are less invasive, helping patients recover faster and do better.
Thermal Ablation Techniques
Thermal ablation is a main part of interventional oncology. It uses heat or cold to kill cancer cells. The main methods are:
- Radiofrequency Ablation (RFA)
- Microwave Ablation
- Cryoablation
RFA uses electrical currents to heat up and kill tumor cells. Microwave ablation does the same but with microwave energy. Cryoablation freezes cells to destroy them.
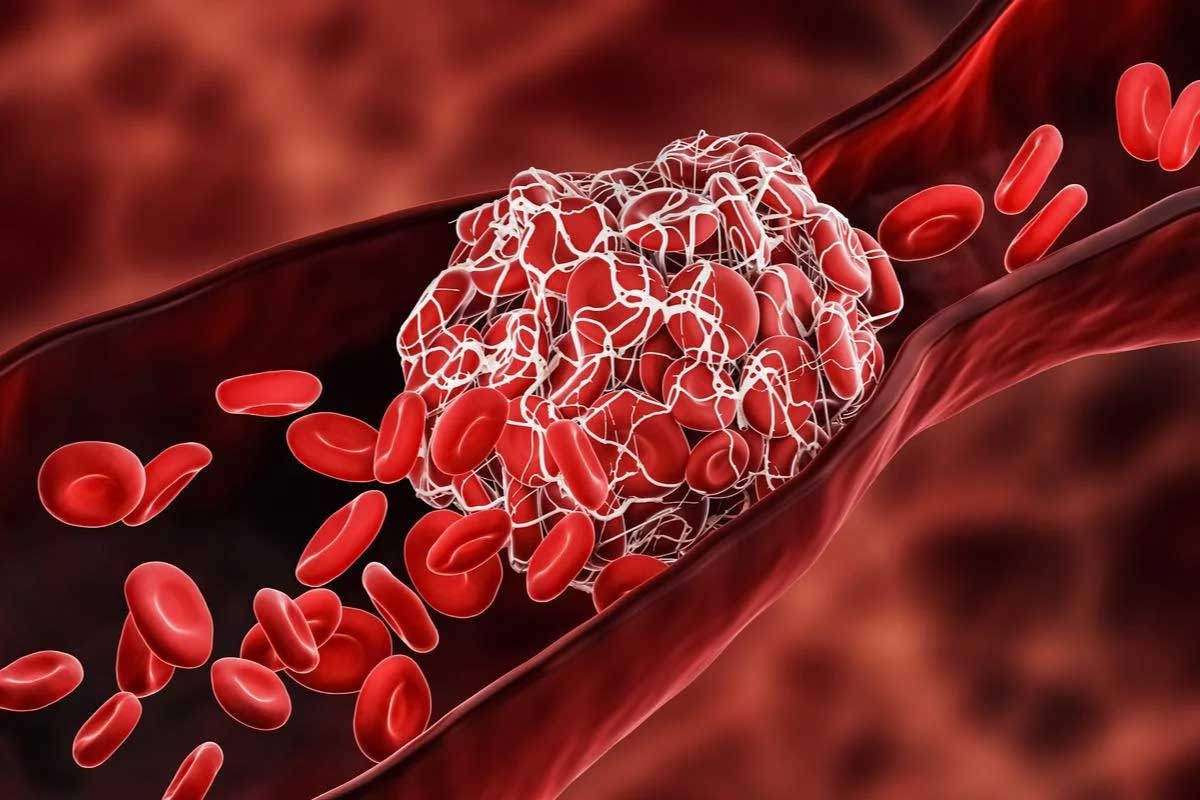
Embolization Procedures
Embolization procedures are also vital in interventional oncology. They cut off the blood supply to tumors, starving them. The main techniques are:
- Transarterial Chemoembolization (TACE)
- Yttrium-90 (Y90) Radioembolization
TACE delivers chemotherapy directly to the tumor while cutting off its blood supply. Y90 radioembolization uses beads with Y90, a radioactive isotope, to target the tumor’s blood supply.
Targeted Drug Delivery Methods
Targeted drug delivery aims to get drugs directly to the tumor, reducing side effects. The main methods are:
- Transarterial Chemotherapy
- Drug-Eluting Beads
Transarterial chemotherapy delivers drugs directly to the tumor’s arteries. Drug-eluting beads are loaded with drugs and injected into the tumor’s blood supply, releasing drugs slowly.
| Treatment | Description | Primary Use |
| RFA | Uses electrical currents to heat and destroy tumor cells | Liver, kidney, and lung tumors |
| TACE | Delivers chemotherapy and blocks blood supply to the tumor | Liver cancer |
| Y90 Radioembolization | Injects radioactive beads into the tumor’s blood supply | Liver cancer |
These treatments in interventional oncology show great promise in fighting cancer. By knowing the options, we can make treatment plans that fit each patient’s needs. This improves their outcomes and quality of life.
Organ-Specific Applications in Interventional Oncology
Interventional oncology offers targeted treatments for various organs hit by cancer. It’s a key part of cancer treatment, using small procedures that meet each patient’s needs.
Liver Cancer Interventions and Outcomes
The liver often sees cancer, both primary and spread. Doctors use several methods to tackle liver cancer, like:
- Transarterial Chemoembolization (TACE)
- Transarterial Radioembolization (TARE or Y90 Radioembolization)
- Thermal Ablation (Radiofrequency Ablation or Microwave Ablation)
These methods have shown great promise. They can boost survival chances and improve life quality for liver cancer patients. For example, TACE delivers chemotherapy right to the tumor and blocks its blood supply, starving it.
Lung Tumor Management Approaches
Lung cancer is tough to treat. But, interventional oncology brings new ways to handle lung tumors, such as:
- Thermal Ablation: Methods like RFA and MWA kill lung tumors.
- Embolization Techniques: Procedures like bronchial artery embolization help manage symptoms like bleeding.
These methods help patients who can’t have surgery or have cancer that comes back.
Kidney Cancer Treatment Options
Interventional oncology is also key in treating kidney cancer. Techniques such as:
- Cryoablation
- Radiofrequency Ablation
- Embolization
are used to treat kidney tumors. These small procedures can be an alternative to surgery, reducing recovery time and risks.
In summary, interventional oncology offers specific treatments for liver, lung, and kidney cancers. It uses targeted, small procedures to improve patient outcomes and life quality.
Patient Selection: Who Benefits Most from Interventional Treatments
Interventional oncologists must carefully choose patients for treatments. This selection is key to getting the best results. We team up with other doctors to decide who will benefit most.
Evaluation Criteria for Candidacy
Several factors are looked at when deciding if a patient is a good candidate. These include the cancer type and stage, the patient’s health, and any past treatments. Advanced imaging technologies help a lot in this process. They give us detailed info about the tumor and the patient’s body.
We look at the patient’s medical history and current health. We also consider the cancer’s specific traits. This helps us pick the best treatment for them.
Alternative Options for Non-Candidates
For those not fit for interventional oncology, we look at other options. This might include conventional cancer therapies like surgery, chemo, or radiation. We also consider clinical trials for new treatments.
If interventional oncology isn’t the best choice, we create a plan just for them. It meets their unique needs and situation.
The Meaning and Significance of “Interventional” in Cancer Care
“Interventional” in cancer care means moving towards treatments that are more precise and less invasive. This shift has greatly changed how we fight cancer today.
Interventional oncology (IO) therapy is key in cancer treatment. It offers patients treatments that are less invasive and target tumors directly. Thanks to advanced imaging, these treatments are more accurate and have fewer side effects than old methods.
Medical Definition and Clinical Implications
“Interventional” means using advanced tech to directly attack disease sites. In cancer care, this means using these tools to find and treat tumors. The term includes thermal ablation techniques, embolization procedures, and targeted drug delivery methods.
- Thermal ablation techniques, like radiofrequency ablation (RFA) and microwave ablation, use heat to kill cancer cells.
- Embolization procedures, like transarterial chemoembolization (TACE) and Y90 radioembolization, block blood to tumors.
- Targeted drug delivery methods let doctors give chemotherapy or other drugs right to the tumor.
These procedures are big deals because they offer effective treatments with less recovery time and fewer side effects than surgery.
Interventional vs. Conventional Treatment Approaches
Interventional treatments differ from old-school cancer treatments in big ways. Old treatments can affect the whole body, causing many side effects. But, interventional oncology focuses on the tumor itself, protecting healthy tissues.
The definition of interventional therapy shows it can lead to better patient outcomes. By adding interventional oncology to cancer care plans, doctors can offer more tailored treatments.
In short, knowing about “interventional” in cancer care is key to understanding its role in today’s oncology. As IO therapy grows, it will likely become even more vital in fighting cancer.
Onco Radiology: Collaborative Multidisciplinary Cancer Care
At the core of onco radiology is the idea of working together to fight cancer. This approach brings radiologists, oncologists, and other experts together. They work as a team to create detailed treatment plans for each patient.
Tumor Board Decision-Making Process
Tumor boards are key in planning cancer treatments. They are made up of many experts who look at each patient’s case. Together, they make personalized treatment plans.
The process of making decisions in a tumor board includes:
- Looking at the patient’s medical history and test results
- Talking about different treatment options and what might happen
- Creating a detailed plan that fits the patient’s needs
Personalized Treatment Planning and Implementation
Personalized treatment is a big part of onco radiology. We focus on each patient’s cancer to make treatments that work better. This approach helps improve results.
The good things about personalized treatment are:
- Better treatment results
- Less chance of bad side effects
- Better quality of life for patients
By working together, we offer the best care to cancer patients. Onco radiology is a big step forward in cancer treatment. It gives hope to patients and their families.
Conclusion: Advancing Cancer Care Through Interventional Oncology
Interventional oncology is changing how we treat cancer. It offers new, less invasive ways to fight tumors. Techniques like heat or cold ablation are making a big difference.
As this field grows, it’s becoming a key part of cancer care. It combines advanced treatments to create personalized plans. This approach improves patient outcomes and quality of life.
The future of cancer treatment looks bright. Ongoing research in interventional oncology is leading to new, better treatments. It’s clear that this field will be essential in improving cancer care for patients everywhere.
FAQ
What is interventional oncology?
Interventional oncology is a medical field. It uses advanced imaging to treat cancer. This approach is less invasive and targets tumors directly.
What is the role of an interventional oncologist?
An interventional oncologist uses imaging to find and treat cancer. They aim to reduce risks and speed up recovery. This is done by delivering treatments directly to tumors.
What are the benefits of interventional oncology treatments?
These treatments cut down on recovery time and hospital stays. They also lead to fewer complications. This improves the quality of life for cancer patients.
What are some common interventional oncology treatments?
Treatments include thermal ablation, embolization, and targeted drug delivery. These methods manage solid tumors in organs like the liver, lungs, and kidneys.
How do interventional oncologists use imaging technologies?
They use CT, MRI, and ultrasound to guide procedures. This allows for precise and accurate treatment delivery. It’s done in real-time.
What is the significance of “interventional” in cancer care?
Interventional oncology offers targeted therapies. These can be used alongside other treatments. This improves patient outcomes and expands treatment options.
How is patient selection determined for interventional oncology treatments?
Doctors work together to choose the best treatments. They consider various factors and alternatives. This ensures the right treatment for each patient.
What is onco radiology, and how does it contribute to cancer care?
Onco radiology combines experts for better cancer care. It plays a key role in treatment planning. This leads to more personalized care for patients.
What is the future of interventional oncology?
This field is growing fast. It offers new ways to treat cancer. Advances in technology and techniques are improving care.
What does “define interventional” mean in the context of cancer treatment?
It means understanding the role of interventional oncology. It highlights its importance in delivering targeted therapies. This improves patient outcomes.
How does interventional oncology integrate with other cancer therapies?
It’s now a key part of cancer treatment. It offers minimally invasive procedures. These can be used with other treatments to better patient outcomes.
References:
- Nanavati, A. J. (2016). Why have we embraced minimally invasive surgery and will it remain? Journal of Minimal Access Surgery, 12(4), 187–192. https://pmc.ncbi.nlm.nih.gov/articles/PMC4916764/