What is Interventional Radiology?
Interventional radiology is a medical specialty that treats many conditions using imaging guidance such as ultrasound, X ray, CT, and sometimes MRI to perform precise, minimally invasive procedures. Instead of making large incisions, interventional radiologists use tiny skin punctures to guide catheters, wires, and special tools right to the problem area.
For patients, this usually means less pain, fewer complications, and a quicker recovery compared to traditional surgery.
If you’re wondering what interventional radiology is, think of it as targeted therapy delivered from the inside out. Common benefits include smaller access points, lower infection risk, shorter hospital stays, and a quicker return to normal activities.
These image guided treatments are used to improve blood flow, stop bleeding, treat tumors, relieve blockages in bile ducts or kidneys, drain infections, and manage pain from spine fractures, along with many other conditions.
What Does Interventional Radiology Do? Conditions Treated and Minimally Invasive Care
Patients often ask what does interventional radiology do and when it’s used. Interventional radiology is used for both diagnosis and treatment, across many areas of the body.
Examples of conditions commonly treated:
Vascular disease: Peripheral arterial disease (PAD) causing leg pain when walking; deep vein thrombosis (DVT); pulmonary embolism (PE); varicose veins; chronic venous insufficiency; pelvic congestion syndrome.
Oncology: Targeted cancer care such as tumor ablation (heating, freezing) and embolization to cut blood supply to tumors; specialized liver directed therapies for primary liver cancer or metastases when appropriate.
Women’s health: Uterine fibroid embolization (UFE) for heavy bleeding and pelvic pressure; pelvic pain related to varicose veins in the pelvis.
Men’s health: Prostatic artery embolization (PAE) to improve urinary symptoms from enlarged prostate
(BPH) for selected candidates.
Organ and drainage: Biliary drainage or stents for blocked bile ducts; nephrostomy for kidney blockage; abscess and fluid drainage in the abdomen, chest, or soft tissues.
Spine and pain: Vertebroplasty or kyphoplasty for painful compression fractures to improve stability and reduce pain.
Dialysis access: Creation and maintenance of fistulas and grafts; angioplasty or clot removal to keep access working.
Trauma and bleeding: Emergency embolization to stop internal bleeding.
Interventional Radiology Procedures: What to Expect Before, During, and After
Before
Evaluation: Your team reviews your history, medications (especially blood thinners), allergies (including iodine/contrast), and prior imaging.
Testing: You may need blood work or updated ultrasound/CT imaging.
Instructions: You’ll receive clear guidance about fasting, fluids, and which medications to take or hold.
During
Comfort: Most procedures use local anesthesia and light sedation so you’re relaxed and comfortable. Some cases involve deeper sedation or anesthesia when needed.
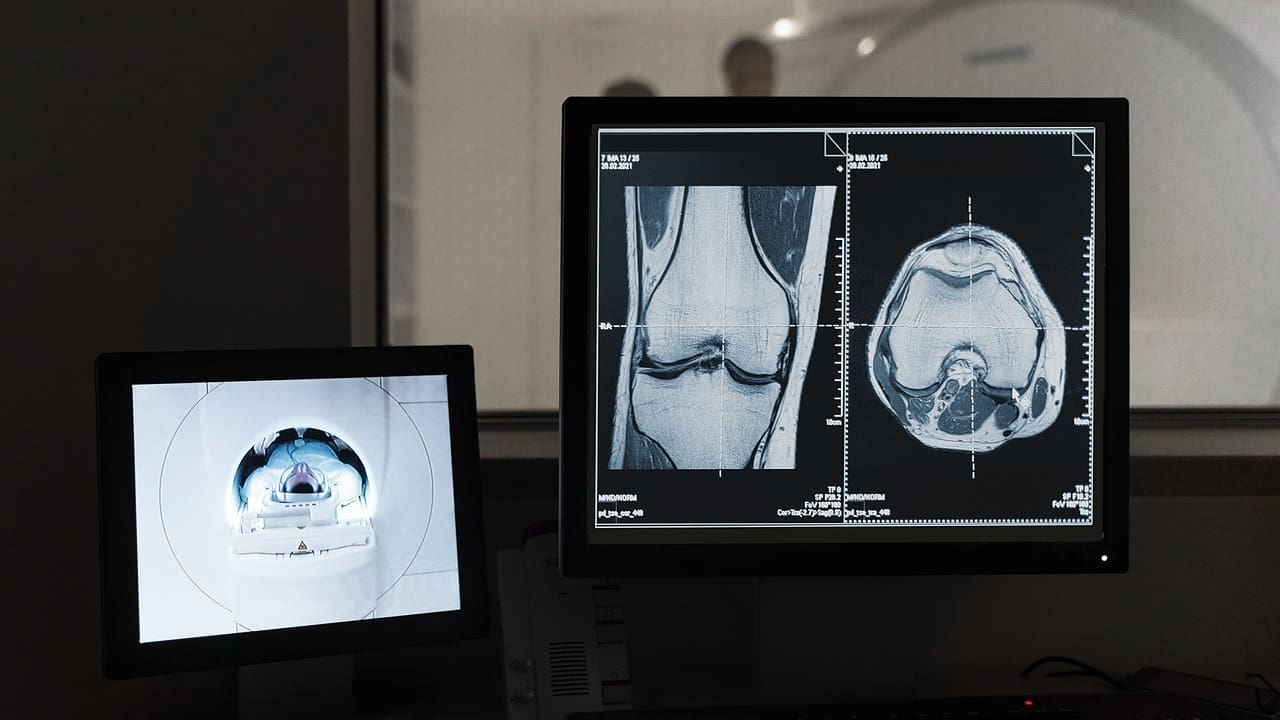
Imaging guidance: Ultrasound, fluoroscopy, or CT directs precise catheter or needle placement.
Safety: The team follows strict sterile protocols and tracks radiation exposure while maintaining accuracy.
After
Recovery: You’ll be monitored for a short period; many patients return home the same day.
Activity: Most resume light activities within 24–72 hours, depending on the procedure.
Follow up: Expect a call or visit to review results, adjust medications, and plan any follow up imaging.
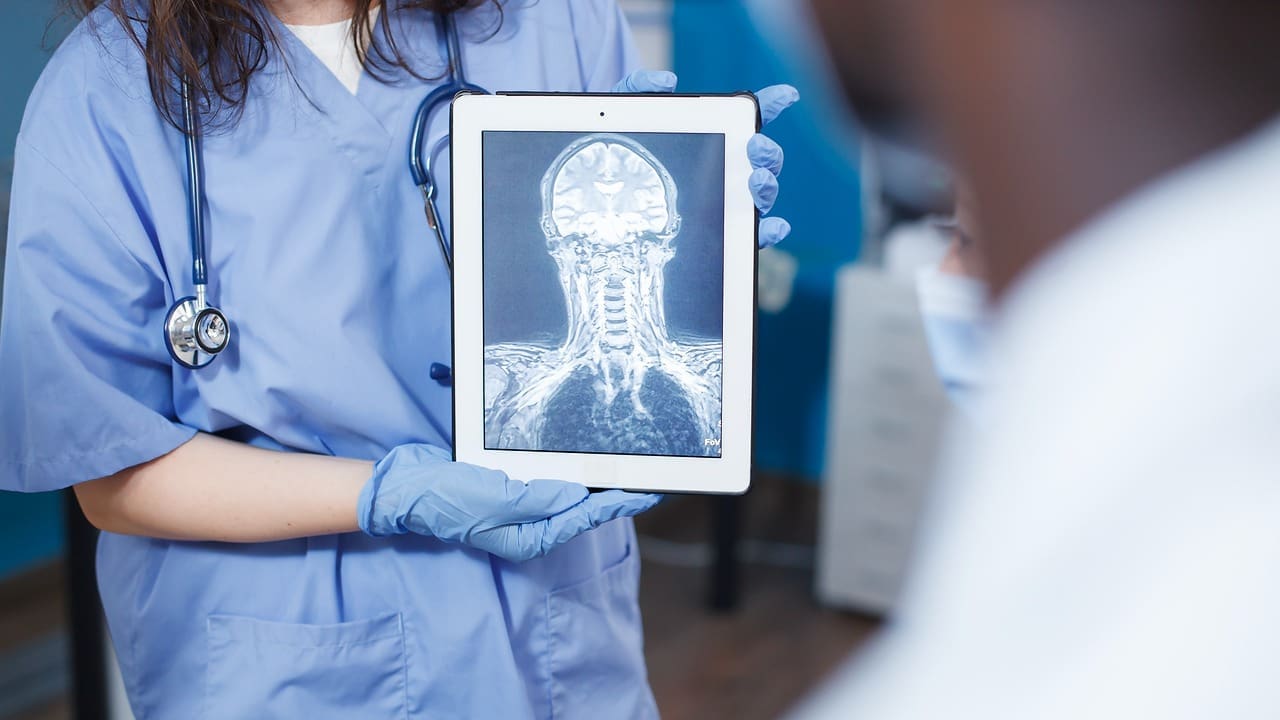
Neuro Interventional Radiology: Stroke and Aneurysm Treatments Explained

Neuro interventional radiology applies minimally invasive, image guided techniques to blood vessels of the brain, head, and neck. For eligible patients experiencing an acute stroke caused by a large vessel clot, mechanical thrombectomy can remove the clot and restore blood flow often improving outcomes when performed quickly.
For brain aneurysms, procedures such as endovascular coiling or flow‐diverting stents seal the aneurysm from within. Carotid artery stenting may help selected patients with carotid stenosis reduce stroke risk.
Because “time is brain,” our team coordinates rapid pathways with stroke centers to evaluate, transfer if needed, and treat quickly. After treatment, patients receive individualized plans for blood pressure, cholesterol, diabetes, smoking cessation, and rehabilitation.

Our Interventional Radiology team uses advanced imaging (CT, ultrasound, fluoroscopy) and precision tools to treat a wide range of conditions — from vascular blockages to tumour ablation — offering lower risk, less pain and faster recovery.
Vascular and Interventional Radiology: PAD, DVT, Varicose Veins, and More
Vascular and interventional radiology focuses on arteries and veins throughout the body. Using angiography (contrast dye and X‐ray), intravascular ultrasound, and ultrasound mapping, specialists diagnose and treat blockages and abnormal veins from the inside.
PAD: Angioplasty and stenting can improve leg blood flow, reduce pain with walking, and help heal wounds.
DVT and PE: Catheter directed thrombolysis or thrombectomy may remove or dissolve clots in selected patients, aiming to reduce long term swelling and improve function.
Varicose veins and venous insufficiency: Endovenous ablation (thermal, laser, or adhesive) and microphlebectomy treat bulging veins and heavy, achy legs. These procedures are often done with local anesthesia and require minimal downtime.
Pelvic congestion syndrome: Minimally invasive vein embolization relieves chronic pelvic pain associated with enlarged pelvic veins.
Interventional Radiology Nurse: Who They Are and What They Do for Your Care
- Prepare you for procedures, review instructions, and answer questions.
- Start IVs, monitor your sedation, and track vital signs throughout the procedure.
- Provide recovery care, pain control guidance, wound care tips, and discharge instructions.
- Coordinate follow up calls and visits to ensure smooth recovery. Interventional radiology nursing also includes education on medications, contrast reactions, and signs that should prompt a call to the clinic.
Interventional Radiology Near Me: When to See a Specialist and How to Prepare
Consider an interventional radiology consultation if you have:
- Leg pain with walking, nonhealing foot wounds, or symptoms of PAD.
- Varicose veins, leg heaviness, or swelling that affects daily life.
- Heavy menstrual bleeding from uterine fibroids or pelvic pressure.
- BPH symptoms (frequent urination, weak stream) and want minimally invasive options.
- Known DVT, venous insufficiency, or concerns about blood clots.
- Liver tumors or metastases being evaluated for embolization or ablation.
- Kidney or biliary obstruction causing pain, infection, or jaundice.
- Painful spine compression fractures affecting mobility.
- Recurrent infections or fluid collections needing drainage.
- Dialysis access problems (low flow, clotting, swelling).
How to prepare:
- Bring prior imaging and lab results if available.
- Share all medications and allergies, including any reactions to contrast dye.
- Ask about sedation, activity restrictions, and when you can return to work.
- Arrange a driver for sedated procedures.
Is Interventional Radiology Safe? Risks, Recovery, and Patient Safety Standards
Patients commonly ask if interventional radiology is safe and is a form of radiology or surgery.Interventional radiology procedures are generally safe and often carry a lower risk than open surgery because they use small access points and less anesthesia. Potential risks include bleeding, infection, allergic reactions to contrast, or injury to nearby vessels or organs. These are uncommon, and your team discusses individualized risks beforehand.
Safety standards we follow:
- Society level checklists and time outs for correct patient, site, and procedure.
- Sterile technique and antibiotic stewardship to reduce infection risk.
- Kidney protection protocols for contrast, and alternatives when needed.
- Radiation dose optimization and tracking to keep exposure as low as reasonably achievable.
Most patients experience faster recovery and fewer complications compared with traditional surgery. Many procedures are outpatient with same day discharge.
What’s the Difference Between Radiology and Interventional Radiology?

Diagnostic radiology focuses on imaging to detect and monitor disease (for example, X‐rays, ultrasound,CT, MRI). Interventional radiology uses those imaging tools to treat conditions through tiny incisions without open surgery.
If you’ve searched what is the difference between radiology and interventional radiology or what is vascular and interventional radiology, the simple answer is: diagnostic radiology shows what’s wrong; interventional radiology can often fix it using image guidance.
Why Choose Interventional Radiology: Faster Recovery, Fewer Complications
When medically appropriate, interventional radiology offers:
- Minimally invasive access with tiny entry points.
- Lower infection risk and less postoperative pain.
- Shorter hospital stays and quicker return to activities.
- Targeted therapy that preserves healthy tissue.
- Options for patients who are not ideal surgical candidates.
Patient Friendly Examples of Interventional Radiology Procedures
Angioplasty and stenting: Open narrowed arteries in legs or kidneys to improve blood flow and reduce pain.
Embolization: Block abnormal vessels feeding fibroids, tumors, or bleeding sites to relieve symptoms or control hemorrhage.
Ablation (radiofrequency, microwave, cryoablation): Destroys tumors by precisely heating or freezing them. This is often done as an outpatient procedure.
Endovenous ablation and sclerotherapy: Treat varicose veins and venous insufficiency to improve comfort and leg appearance.
Vertebroplasty/kyphoplasty: Stabilize painful spine fractures to reduce pain and improve mobility.
Biliary and urinary stenting/drainage: Relieve obstructions that cause pain, infection, or jaundice.
Abscess and fluid drainage: Safely remove infected or excess fluid from abdomen, chest, or soft tissues under imaging guidance.
Dialysis access interventions: Keep fistulas and grafts working well with angioplasty or clot removal.
Recovery Timeline and Daily Life After IR Procedures
How long does interventional radiology take? Most procedures last 30–120 minutes, plus a short recovery period. Many patients return to light activity within 1–3 days. Your exact timeline depends on the procedure type, your overall health, and job demands. You’ll receive personalized instructions on:
- Wound care and bathing.
- Pain control and safe activity progression.
- Medications to start, stop, or continue.
- Warning signs that warrant a call (fever, severe pain, increasing redness, shortness of breath).
Liv Hospital Interventional Radiology;
Liv Hospital Radiology Clinic offers the opportunity to treat many diseases from brain aneurysms to brain tumors with interventional radiology techniques without surgery.
After the procedure, the patient can be discharged directly. The clinic has a high tech angiography device that guides the interventions. Non surgical varicose vein treatment is performed in the clinic, which provides 100% improvement, and the patient is discharged immediately after treatment.
Vascular diagnosis and treatments
Stenting and angioplasty procedures (Aorta, iliac, renal, mesenteric, femoral and below the knee vessels, upper extremity, dialysis fistula stenosis) Aneurysm treatment Preoperative embolization in hypervascular tumors (Bone tumor metastasis, RCC, Neural tumors, etc.) Embolization as a non surgical minimally invasive option for the semtomatic treatment of myoma and adenomyosis Tissue biopsies, drainages and RF ablation treatments in oncological patients.
Treatment of locally advanced liver tumors
Local tumor ablation (RF ablation, Microwave ablation, Nanoknife, etc.) in the group of patients who are not surgical candidates (Liver, lung, kidney and thyroid) Fine needle and tru cut all organ biopsies (Liver, kidney, lung, bone, prostate, thyroid, pancreas, etc.) Abscess, collection, biliary system, urinary system, pleural and peritoneal fluid drainage are performed.
For more information about our academic and training initiatives, visit Liv Hospital Academy.
Frequently Asked Questions for Invertional Radiology
What does an interventional radiology nurse do?
Preps you for procedures, manages IVs and sedation, monitors safety, provides recovery instructions,
and coordinates follow-up.
What is neuro interventional radiology?
A subspecialty focused on brain, head, and neck vessels, treating stroke (mechanical thrombectomy), aneurysms (coiling, flow-diversion), and carotid stenosis (stenting) in selected patients.
What is the difference between radiology and interventional radiology?
Diagnostic radiology finds and monitors disease with imaging. Interventional radiology uses imaging to
treat disease through minimally invasive procedures.
Is interventional radiology considered surgery?
It’s not open surgery. It’s minimally invasive “image-guided surgery” done through tiny access points, often without general anesthesia.
Is interventional radiology safe?
Yes, for most patients it’s very safe. Risks like bleeding, infection, or contrast reactions are uncommon and discussed in advance. Safety protocols minimize radiation and protect kidney function.
What is an interventional radiology procedure like?
Most use local anesthesia with light sedation, last 30–120 minutes, and are outpatient with quick recovery and clear aftercare instructions.
What is an example of interventional radiology?
Uterine fibroid embolization to reduce heavy bleeding and pain; angioplasty and stenting to restore leg blood flow; abscess drainage guided by ultrasound.




