Last Updated on November 20, 2025 by Ugurkan Demir
Acute Lymphoblastic Leukemia (ALL) is a blood and bone marrow cancer. We don’t know all about its causes yet. But, research shows genetics and heredity are key in who gets it. Learn is all hereditary, genetic causes, and risk factors contributing to acute lymphoblastic leukemia in children.
Most ALL cases aren’t passed down in families. Yet, some genetic changes and syndromes raise the risk. The American Cancer Society says most ALL patients have known risk factors. But, it’s tricky to say these factors actually caused the leukemia.
At Liv Hospital, we give you the facts about ALL’s genetic causes and risk factors. This helps you understand your situation better.

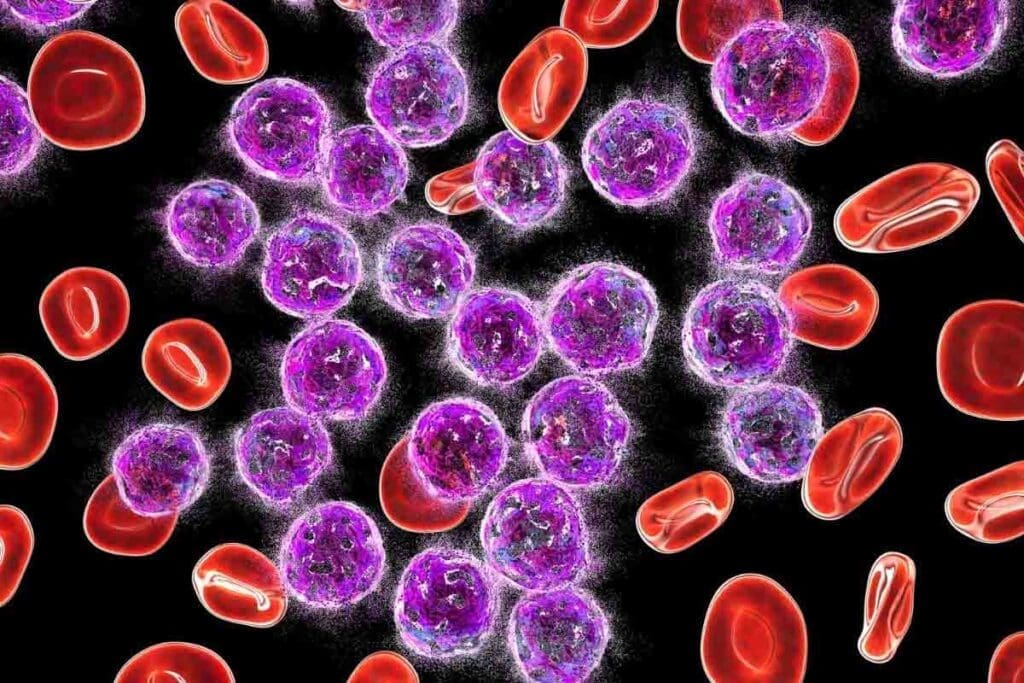
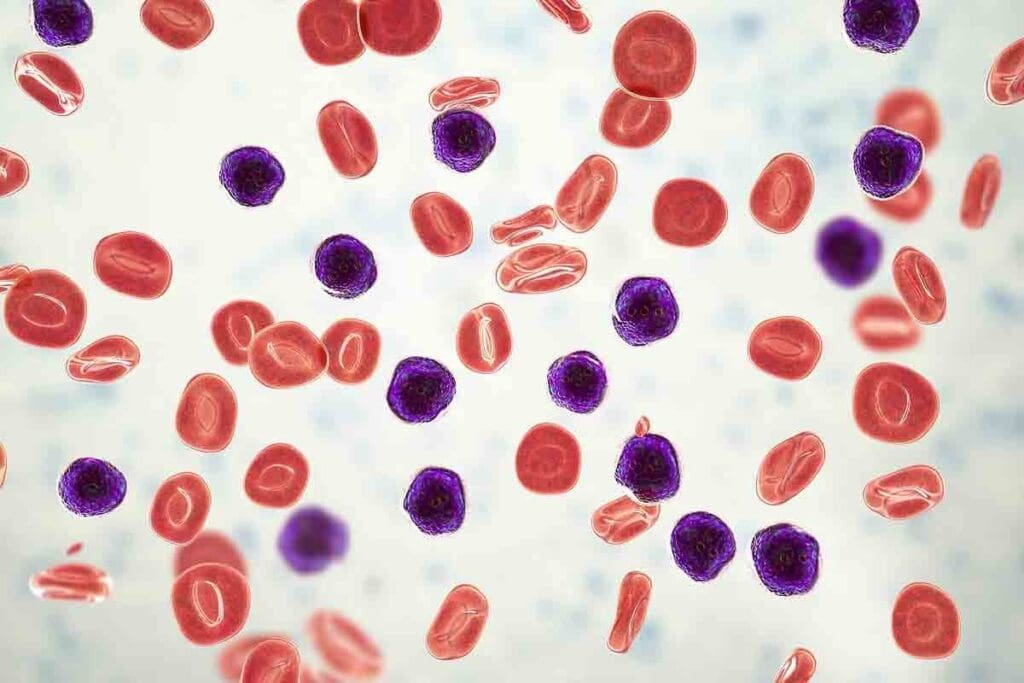
ALL, or Acute Lymphoblastic Leukemia, is a cancer that affects blood cell production in the bone marrow. It happens when immature blood cells, called lymphoblasts or leukemic blasts, grow too fast. These cells take over the bone marrow, leaving little room for normal blood cells.
ALL starts with genetic changes in bone marrow cells. These changes can happen on their own or because of environmental factors. As a result, the bone marrow makes abnormal white blood cells that can’t fight off infections well.
The growth of ALL involves genetics and the environment. Genetic mutations are key, and some genetic syndromes raise the risk of getting ALL.
ALL is divided into types based on the affected blood cell and the leukemia cells’ genetics. The main types are B-cell ALL and T-cell ALL, with B-cell ALL being more common, mainly in kids.
ALL is the most common cancer in kids but can also affect adults. Its occurrence changes with age, peaking in early childhood and again in adults over 60.
Knowing who gets ALL helps find risk factors and create better treatments. Studies on genetic predisposition and environmental exposures are helping us understand this complex disease better.
To figure out if Acute Lymphoblastic Leukemia (ALL) is hereditary, we need to know what ‘hereditary’ means in cancer terms. Hereditary conditions come from parents to kids through genes. But, genetic conditions can happen due to DNA changes or mutations.
Not every genetic condition is passed down. Some can happen because of the environment or random DNA errors.
The words ‘hereditary’ and ‘genetic’ are often mixed up, but they’re not the same. Hereditary conditions come from parents. Genetic conditions are caused by DNA changes.
ALL is seen as a genetic condition because of specific DNA mutations. But, is it hereditary? That depends on if these mutations are passed down.
Many think leukemia, like ALL, is passed down from parents. But, the National Cancer Institute says most leukemia isn’t inherited. It’s caused by a mix of genes and the environment.
This is key to understanding ALL’s risks and causes.
Most ALL cases aren’t hereditary. While some families may have it, it’s rare. Less than 5% of ALL cases have a family link.
The exact number can change based on the study and the genetic syndromes involved.
In short, ALL is linked to genetic mutations but isn’t usually hereditary. Knowing the difference between genetic and hereditary is important for understanding ALL’s risks and causes.
ALL’s causes mix acquired genetic changes with inherited ones. Most ALL-related genetic changes happen during a person’s life, not from parents. Knowing the difference helps doctors diagnose and treat ALL better.
Somatic mutations happen in non-reproductive cells and aren’t passed to kids. In ALL, these mutations are the main cause. They can come from many things like environmental factors, DNA copying mistakes, or viruses.
Key characteristics of somatic mutations in ALL include:
Germline mutations, found in reproductive cells, are passed to kids. Though rarer, they can raise the risk of ALL. Some genetic syndromes linked to germline mutations also increase ALL risk.
Examples of germline mutations linked to ALL include:
| Genetic Syndrome | Associated Gene | Risk Implication |
| Li-Fraumeni Syndrome | TP53 | Increased risk of various cancers, including ALL |
| Down Syndrome | Trisomy 21 | Higher risk of developing ALL |
Telling somatic from germline mutations is key to understanding ALL. It helps figure out risk and treatment plans. Genetic tests can show if a mutation is somatic or germline.
Knowing about ALL’s genetic mutations helps us see how complex the disease is. It shows why we need treatments tailored to each person.
Genetic predisposition from certain syndromes can greatly increase the risk of Acute Lymphoblastic Leukemia (ALL). We will look at the inherited genetic syndromes linked to a higher risk of ALL.
People with Down syndrome are more likely to get ALL. Studies show they are 20 times more at risk than others. The extra chromosome 21 is thought to play a role in this increased risk.
Li-Fraumeni syndrome is a rare genetic disorder caused by TP53 gene mutations. Those with this syndrome face a higher risk of cancers, including ALL. The mutation hampers the body’s DNA repair, raising cancer risk.
Fanconi anemia is a genetic disorder that affects DNA repair. It increases the risk of cancers like ALL due to genetic mutations.
Several rare genetic syndromes also raise the risk of ALL. These include:
These syndromes often have DNA repair or tumor suppressor defects. They show the complex genetic nature of ALL.
Understanding these syndromes and their link to ALL can help us understand the disease better. It may also guide treatment strategies.
Acute Lymphoblastic Leukemia (ALL) is linked to several key gene mutations. These genetic changes disrupt normal cell functions. This leads to the growth of cancerous lymphoblasts.
Mutations in the ETV6 and PAX5 genes are common in ALL patients. ETV6 helps control blood cell development. Its mutation causes abnormal blood cells.
PAX5 is key for B-cell development. Mutations in this gene stop B-cell maturation. This contributes to B-cell ALL.
DNA repair genes keep our genome stable. Mutations in these genes make it hard for cells to fix DNA damage. This leads to genetic instability and a higher risk of ALL.
Tumor suppressor genes, like TP53, control cell growth and prevent tumors. Mutations in these genes remove their protective effects. This helps ALL develop and grow.
Oncogenes, when mutated or overactive, promote cell growth and survival. This contributes to leukemia. Specific oncogenes are often active in ALL, causing lymphoid cells to become malignant.
| Gene Mutation | Function | Impact on ALL |
| ETV6 | Regulates hematopoiesis | Abnormal blood cell development |
| PAX5 | Crucial for B-cell development | Arrest of B-cell maturation |
| TP53 | Tumor suppressor gene | Loss of protective functions |
Understanding these gene mutations is key to understanding ALL. It helps us develop targeted treatments. More research will help us better understand this complex disease.
It’s key to know about chromosomal changes in Acute Lymphoblastic Leukemia (ALL) for good diagnosis and treatment. These changes affect how the disease grows and reacts to treatment.
Hyperdiploidy means leukemia cells have more than 50 chromosomes. This is good news for kids with ALL. Studies show that having extra chromosomes can change how the disease acts and how well it responds to treatment.
Research shows kids with hyperdiploid ALL do well with chemotherapy. This leads to better survival rates. The extra chromosomes might make the leukemia cells more treatable.
Translocations swap genetic material between chromosomes, creating fusion genes that can cause leukemia. In ALL, common ones include the BCR-ABL1 and MLL-AF4 fusion genes. These come from swaps between chromosomes 9 and 22, and 4 and 11, respectively.
These genetic changes affect how well ALL can be treated. For example, BCR-ABL1 is linked to a worse outlook. But, new treatments like tyrosine kinase inhibitors have helped these patients more.
Chromosomal changes in ALL are vital for predicting the disease’s course and treatment. They help doctors choose the best therapy for each patient.
| Chromosomal Abnormality | Prognostic Impact | Treatment Implications |
| Hyperdiploidy | Favorable prognosis | Responsive to chemotherapy |
| BCR-ABL1 fusion | Poor prognosis | Targeted therapy with tyrosine kinase inhibitors |
| MLL-AF4 fusion | Variable prognosis | Intensive chemotherapy and possible targeted therapy |
Knowing the chromosomal changes in a patient’s leukemia is key for effective treatment. By identifying these changes, doctors can create a treatment plan that targets the disease’s root causes. This improves patient outcomes.
Understanding the risk of Acute Lymphoblastic Leukemia (ALL) starts with looking at family medical history. If your family has a history of leukemia or other cancers, your risk might be higher. This is true, even more so if there are known genetic syndromes involved.
Genetic testing is a good idea if your family has a lot of leukemia or related cancers. People with a family history of known genetic syndromes like Li-Fraumeni or Down syndrome should think about genetic counseling and testing. This can spot genetic changes that might raise your risk of getting ALL.
Genetic testing is advised for those with:
Looking at family cancer patterns means checking the types of cancers and when they were found. Seeing many cancers in a family, or cancers that happen when people are young, might mean there’s a genetic link.
| Family Cancer Pattern | Potential Indication |
| Multiple cases of leukemia or lymphoma | Possible genetic predisposition to hematological malignancies |
| Cancers diagnosed at a young age | Potential hereditary cancer syndrome |
| Multiple types of cancer in a single individual | Possible genetic mutation affecting multiple cancer types |
Calculating the risk of ALL looks at family history, genetic changes, and environmental factors. Tools like the Claus model for breast cancer are being adapted for leukemia risk assessment. These tools help figure out the risk based on family history and other factors.
We combine:
By understanding family history, we can better figure out the risk of ALL. This helps us suggest the right steps for genetic testing and managing risk.
Acute Lymphoblastic Leukemia (ALL) is shaped by a mix of genes and the environment. We’ve looked at the genetic side before. Now, let’s see how the environment adds to the risk of ALL.
Being exposed to ionizing radiation is a known risk for ALL. This can happen from nuclear accidents, some medical treatments, or work-related exposure. Chemicals like benzene and pesticides also raise the risk of getting ALL.
Key Environmental Risk Factors:
Environmental factors can cause genetic changes that might lead to ALL. For example, ionizing radiation can damage DNA, causing mutations in genes that control cell growth. Chemicals can also change genes, messing with how cells work.
“The interaction between environmental exposures and genetic susceptibility plays a critical role in the etiology of ALL.”
— Medical Expert, Leukemia Researcher
Knowing how these interactions work is key to stopping ALL before it starts. It helps us find who’s at higher risk because of their environment.
Some risks can’t be avoided, but others can. For instance, we can lower radiation risk by using protective gear and careful therapy. Staying away from harmful chemicals like benzene also helps prevent ALL.
| Risk Factor | Preventive Measure |
| Ionizing Radiation | Use of protective equipment, judicious use of radiation therapy |
| Benzene Exposure | Avoidance of benzene-containing products, use of protective gear in occupational settings |
| Pesticide Exposure | Use of personal protective equipment, safer pesticide alternatives |
By tackling these environmental risks, we can lower ALL cases. This improves life for those with the disease.
Research is making big strides in understanding Acute Lymphoblastic Leukemia (ALL). We’re learning about new treatments and ways to prevent it. The study of ALL genetics is growing fast, with new insights into its causes and risk factors.
New genetic mutations linked to ALL have been found. These changes affect genes involved in cell development and DNA repair. These emerging genetic discoveries are key to understanding ALL and finding better treatments.
For example, studies show that mutations in ETV6 and PAX5 genes play a big role in ALL. These genes are important for cell development, and problems with them can cause leukemia.
Knowing the specific genetic changes in ALL patients is leading to personalized medicine. Doctors can now tailor treatments based on each patient’s unique genetic profile. This approach aims to improve treatment results and lower the chance of relapse.
It also helps avoid unnecessary chemotherapy and its side effects. This makes treatment more effective and safer for patients.
For those at high risk of ALL, like those with a family history, preventive strategies are being looked into. These might include regular check-ups, genetic counseling, and preventive treatments.
It’s important to understand the genetic risks of ALL to develop good prevention plans. Research is focused on spotting high-risk individuals early and stopping the disease before it starts.
As we learn more about ALL genetics, we’re getting closer to better treatments and prevention. This is a big step towards fighting this complex disease.
Acute lymphoblastic leukemia (ALL) is a complex disease. It involves many factors like genetics, heredity, and environment. Most ALL cases aren’t passed down through families, but some genetic and hereditary factors can raise a person’s risk.
Studies have found that genetic changes, like those in the ETV6 and PAX5 genes, are key in ALL. Also, inherited conditions like Down syndrome and Li-Fraumeni syndrome can make someone more likely to get ALL.
Exposure to radiation and some chemicals can also lead to ALL by causing genetic changes. Knowing what causes ALL is vital for finding better ways to prevent and treat it.
As we learn more about ALL, it’s clear we need a broad approach to tackle it. By looking at how genetics, heredity, and environment interact, we can help those with ALL.
Most ALL cases are not passed down through genes. But, some genetic mutations and syndromes can raise the risk of getting ALL.
Genetic conditions come from gene mutations. Hereditary conditions are passed down through genes. Not all genetic conditions are hereditary.
No, not all leukemia cases are genetic. While genes play a role, environment also affects the risk.
Down syndrome, Li-Fraumeni syndrome, and Fanconi anemia are linked to a higher risk of ALL.
Chromosomal issues, like having more than 50 chromosomes, can change how ALL is treated. Some issues are better, others worse.
Family history is important for ALL risk. It’s key if there’s a history of leukemia or cancers in the family.
Genetic testing might be needed for those with a family history of leukemia or cancers. Or for those with known genetic syndromes linked to ALL.
Yes, things like radiation and chemicals can increase the risk of ALL by causing genetic changes.
Research is looking at new genetic discoveries, personalized medicine, and ways to prevent ALL in high-risk groups.
There’s no sure way to prevent ALL. But avoiding harmful environments and genetic testing for high-risk individuals might help.
Having more than 50 chromosomes, or hyperdiploidy, is a common abnormality in ALL. It often means a better prognosis.
While most leukemia is not inherited, some genetic mutations and syndromes can increase the risk.
The exact cause of ALL is not fully known. It’s believed to be a mix of genetic and environmental factors.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!