
Aplastic anemia is a serious blood disorder. It happens when the bone marrow can’t make enough blood cells. Severeaplastic anemia (SAA) is the most serious form. It means there’s a big drop in blood cell production.
Knowing how to diagnose and treat aplastic anemia is key. A bone marrow transplant can be a cure for some patients.
At Liv Hospital, we use the newest treatments for aplastic anemia. This includes bone marrow transplant. We focus on our patients and use methods known worldwide.
Key Takeaways
- Understanding the aplastic anemia diagnosis is key to good care.
- Severe aplastic anemia (SAA) is a serious form of the disease.
- A bone marrow transplant is a possible cure for some.
- Liv Hospital offers care that puts patients first for aplastic anemia treatment.
- We use methods known worldwide in our treatment.
Understanding Aplastic Anemia: A Bone Marrow Failure Disorder

Aplastic anemia happens when the bone marrow can’t make enough blood cells. This includes red blood cells, white blood cells, and platelets. It’s caused by a problem with the bone marrow’s stem cells, leading to a lack of all blood cell types.
What Happens in the Bone Marrow
The bone marrow makes blood cells from stem cells. But in aplastic anemia, this process stops working. This means the marrow can’t make enough red blood cells, white blood cells, and platelets.
This failure can cause tiredness, infections, and bleeding problems. The reasons for aplastic anemia include the immune system attacking the bone marrow and problems with the stem cells themselves.
Common Causes and Risk Factors
Many things can lead to aplastic anemia. These include:
- Exposure to certain chemicals and toxins
- Radiation therapy
- Viral infections
- Autoimmune disorders
- Genetic predispositions
Knowing these causes and risk factors helps doctors diagnose and treat aplastic anemia. We’ll look at these in more detail to understand the condition better.
Severe Aplastic Anemia (SAA): Defining the SAA Medical Abbreviation
Severe Aplastic Anemia (SAA) is a serious condition where the bone marrow doesn’t make enough blood cells. This leads to severe health problems. Knowing how severe Aplastic Anemia is helps doctors choose the right treatment.
Classification of Severity Levels
Aplastic Anemia is sorted by how severe it is. Doctors look at blood cell counts and the patient’s health to decide. This helps them pick the best treatment.
| Severity Level | Characteristics |
| Mild | Some reduction in blood cell counts, but patients may not show significant symptoms. |
| Moderate | Noticeable reduction in blood cell counts, with some symptoms such as fatigue and infections. |
| Severe (SAA) | Significant reduction in blood cell counts, with severe symptoms including frequent infections, severe anemia, and bleeding. |
Differences Between Mild and Severe Forms
The main difference between mild and severe Aplastic Anemia is how much the bone marrow fails. Mild Aplastic Anemia might not need urgent treatment. But SAA needs quick and strong medical help.
Doctors must understand these differences to create the right treatment plan. For SAA patients, getting a diagnosis and treatment fast is key to avoiding serious problems.
Is SAA Cancer? Understanding the Distinction
SAA is not a cancer, even though it shares some symptoms with blood cancers. It is a bone marrow failure disorder. This means the body can’t make enough blood cells, which is very serious.
How SAA Disease Differs from Blood Cancers
SAA is different from blood cancers like leukemia or lymphoma. Blood cancers grow out of control in the bone marrow or lymph system. SAA, on the other hand, happens when the bone marrow fails to make enough blood cells.
To tell SAA apart from blood cancer, doctors do blood tests and bone marrow biopsies. Knowing the difference is key to choosing the right treatment.
Similar Symptoms but Different Pathology
Even though SAA and blood cancers have similar symptoms like tiredness, infections, and bleeding, they have different causes. The body reacts differently to each condition.
Getting the right diagnosis is very important. It helps doctors give the right treatment for SAA or blood cancer. Below is a table showing the main differences between SAA and common blood cancers.
| Condition | Pathology | Common Symptoms | Treatment Approach |
| Severe Aplastic Anemia (SAA) | Bone marrow failure | Fatigue, infections, bleeding | Immunosuppressive therapy, bone marrow transplant |
| Leukemia | Malignant proliferation of white blood cells | Fatigue, infections, bleeding, weight loss | Chemotherapy, targeted therapy, and bone marrow transplant |
| Lymphoma | Malignant proliferation of lymphocytes | Swollen lymph nodes, fever, weight loss, fatigue | Chemotherapy, radiation therapy, and immunotherapy |
Understanding the differences between SAA and blood cancers helps doctors give better treatment. This leads to better health outcomes for patients.
Recognizing Symptoms of Aplastic Anemia
It’s important to know the early signs of aplastic anemia to get the right treatment. This condition shows up when there are not enough red and white blood cells and platelets in the body.
Early Warning Signs
The first signs of aplastic anemia can be tricky to spot. They might include:
- Fatigue and weakness because of too few red blood cells. This can cause shortness of breath and dizziness.
- Frequent infections due to low white blood cells. This makes it hard for the body to fight off germs.
- Bleeding or bruising easily. This includes nosebleeds, bleeding gums, or small spots on the skin, all because of low platelet counts.
When to Seek Medical Attention
If you notice any of these, you should see a doctor right away:
- Severe fatigue that makes it hard to do everyday things.
- Recurring infections that don’t get better with treatment.
- Unexplained bleeding or bruising.
Getting diagnosed and treated early can really help people with aplastic anemia. If you’re worried about your symptoms, talk to a doctor. They can help figure out what’s going on and how to take care of you.
The SAA Diagnosis Process: Confirming Aplastic Anemia
To diagnose SAA, doctors use blood tests, bone marrow exams, and other tools. Finding aplastic anemia, a severe form, is complex. It needs careful checks and ruling out other blood disorders.
Complete Blood Count Analysis
The first step is a Complete Blood Count (CBC) test. It checks the levels of red, white blood cells, and platelets. In SAA, the CBC shows low counts of all blood cell types.
CBC Parameters:
| Blood Cell Type | Normal Range | Typical Findings in SAA |
| White Blood Cells (WBC) | 4,500 – 11,000 cells/μL | Decreased |
| Red Blood Cells (RBC) | 4.32 – 5.72 million cells/μL (varies by age and sex) | Decreased |
| Platelets | 150,000 – 450,000 cells/μL | Decreased |
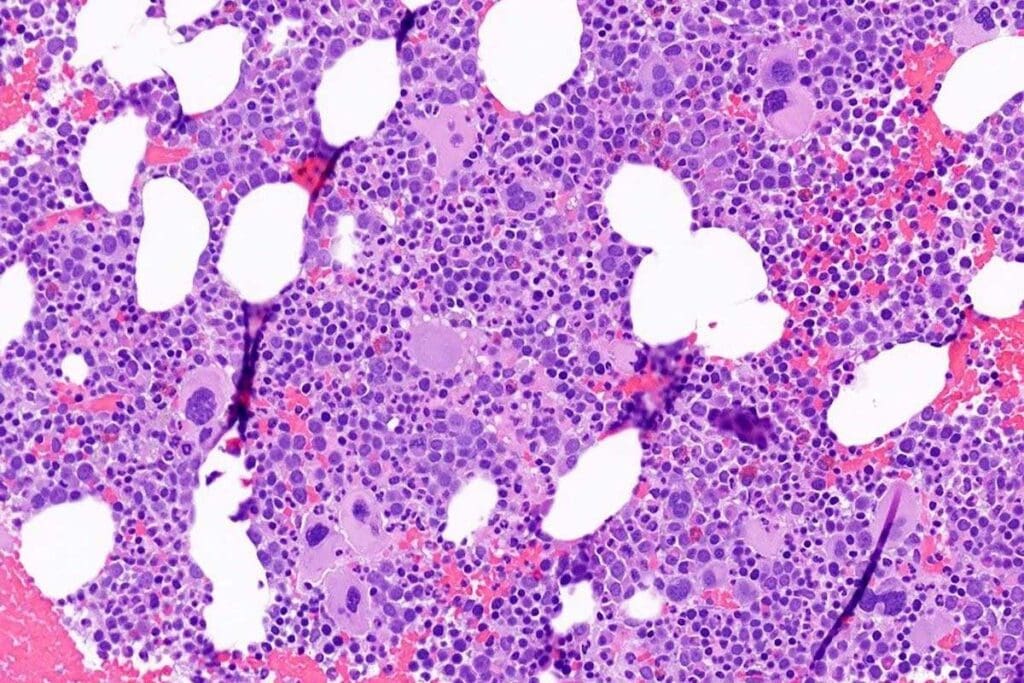
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy and aspiration are key for SAA diagnosis. These take a bone marrow sample for study. In SAA, the marrow has fewer cells than usual.
Additional Testing to Rule Out Other Conditions
More tests are done to confirm SAA and rule out other conditions. These include tests for infections, autoimmune diseases, and other bone marrow failures.
We combine these tests to make sure we diagnose SAA correctly. This helps us plan the right treatment for patients.
Is Aplastic Anemia Curable? Treatment Success Rates
To understand if aplastic anemia is curable, we need to look at treatment success rates and patient outcomes. Aplastic anemia is when the bone marrow can’t make enough blood cells. Thanks to new treatments, many patients now have a better chance of recovery.
Factors Affecting Curability
Several things can affect whether aplastic anemia can be cured. The severity of the disease, the patient’s age, and their health are key. Severe aplastic anemia (SAA) is a more serious case that needs quick action. The treatment chosen, like bone marrow transplantation or immunosuppressive therapy, also matters a lot.
We will look at what makes aplastic anemia curable, including:
- Severity of the condition
- Patient’s age and overall health
- Effectiveness of the chosen treatment
- Response to initial treatment
Long-term Survival Statistics
Thanks to new treatments, more aplastic anemia patients are living longer. Bone marrow transplantation is a promising cure for many, mainly those with severe aplastic anemia.
| Treatment Type | 5-Year Survival Rate | 10-Year Survival Rate |
| Bone Marrow Transplant | 70-80% | 60-70% |
| Immunosuppressive Therapy | 50-60% | 40-50% |
The table shows survival rates for different treatments. Remember, each person’s outcome can vary for many reasons.
Quality of Life After Treatment
After treatment, the quality of life for aplastic anemia patients is very important. Those who get better often feel much better overall. But some may face ongoing issues, like dealing with treatment side effects.
It’s vital to have ongoing care to help with these challenges. This includes regular check-ups, support, and managing any lasting effects of treatment.
Bone Marrow Transplant for Aplastic Anemia: The Curative Approach
Bone marrow transplant (BMT) is a promising cure for aplastic anemia. It replaces the damaged bone marrow with healthy stem cells from a donor. This helps the body make blood cells again.
How BMT Works for Aplastic Anemia
In aplastic anemia, the bone marrow can’t make enough blood cells. BMT starts by getting rid of the damaged bone marrow with chemotherapy and sometimes radiation. Then, the donor’s stem cells are given to the patient. These cells go to the bone marrow and start making new blood cells.
The success of BMT depends on several factors. These include the donor match, the patient’s health, and the treatment plan.
Finding a Compatible Donor
Finding a donor is key in BMT. The best donor is usually a sibling or relative who matches at the HLA genes. If a relative isn’t available, a donor from a registry can be found.
HLA typing is used to find a donor. It helps lower the risk of graft-versus-host disease (GVHD), a big risk of BMT.
The Transplantation Process and Timeline
The BMT starts with the conditioning regimen, lasting from a few days to a week. The transplant itself is quick and painless, where the donor stem cells are given to the patient.
After the transplant, the patient needs to recover. They are watched for signs of engraftment, GVHD, and other issues. The recovery time varies, but patients usually stay in the hospital for weeks and then recover at home for months.
Recovery After Aplastic Anemia Bone Marrow Transplant
Recovering from a bone marrow transplant for aplastic anemia is a long and careful process. It starts with a period of low blood counts, then slowly gets better. Knowing this helps us better care for our patients.
Timeline for Blood Count Recovery
How long it takes to get better varies from person to person. Most people see their blood counts improve over weeks to months after the transplant.
- Neutrophil recovery: Usually happens in the first few weeks.
- Platelet recovery: Takes longer, often needing transfusions until counts are stable.
- Red blood cell recovery: Also takes time, with some needing transfusions early on.
Potential Complications and Management
Even though a bone marrow transplant can cure aplastic anemia, there are risks. We must manage these complications carefully:
| Complication | Management Strategy |
| Graft-versus-host disease (GVHD) | Immunosuppressive medications, close monitoring |
| Infections | Prophylactic antibiotics, isolation precautions |
| Organ toxicity | Supportive care, monitoring of organ function |
Long-term Follow-up Care Requirements
Long-term care is key to watch for disease return and manage transplant side effects. This includes regular visits, blood tests, and treatments for GVHD.
Following up closely is vital for the best long-term results for transplant patients with aplastic anemia.
Immunosuppressive Therapy: When BMT Isn’t an Option
Immunosuppressive therapy is key for aplastic anemia patients who can’t get a bone marrow transplant. It helps by reducing the immune system’s attack on the bone marrow. This makes it easier for the bone marrow to start making blood cells again.
Treatment Mechanism
This therapy calms down the immune system’s harmful attack on the bone marrow. In aplastic anemia, the immune system mistakenly attacks the bone marrow. This leads to a big drop in blood cell production. By stopping this attack, the therapy helps the bone marrow to start making blood cells again.
Medications and Their Effects
The therapy uses a mix of medicines, like antithymocyte globulin (ATG) and cyclosporine. ATG gets rid of T-cells, which are part of the immune system and attack the bone marrow. Cyclosporine also stops T-cells from working, helping the bone marrow to recover.
Key Medications Used:
- Antithymocyte Globulin (ATG)
- Cyclosporine
Success Rates Compared to BMT
- While a bone marrow transplant is a cure for aplastic anemia, immunosuppressive therapy is a good choice when a transplant isn’t possible. The success of this therapy is seen in better blood counts and fewer blood transfusions needed.
| Treatment Outcome | Bone Marrow Transplant | Immunosuppressive Therapy |
| Response Rate | High | Moderate to High |
| Relapse Rate | Low | Moderate |
| Treatment-Related Mortality | Moderate | Low |
- The table shows BMT has a higher success rate and a lower chance of relapse. But immunosuppressive therapy has a lower risk of treatment-related death. This makes it a good choice for patients who can’t have a transplant.
Selecting the Right Treatment Approach: BMT vs. Immunosuppression
Choosing between Bone Marrow Transplant (BMT) and immunosuppression is a big decision. When you’re diagnosed with Severe Aplastic Anemia (SAA), knowing the details of each option is key. This helps you make a choice that’s right for you.
Age and Health Considerations
Age and health are big factors in picking a treatment. Younger patients with a good donor match are often best suited for an MT. It’s a chance for a cure. But older patients or those with health issues might do better with immunosuppressive therapy. This is because BMT can be risky.
- Age under 40: Generally considered more suitable for BMT
- Presence of comorbidities: May lean towards immunosuppressive therapy
- Overall health status: Plays a critical role in treatment tolerance
Donor Availability Factors
Having a compatible donor is key to BMT. A matched sibling donor is the best choice. If not, unrelated donors or cord blood can be options too.
- Matched sibling donor: Ideal for BMT
- Unrelated donor: Alternative option with higher risks
- Cord blood: Considered for patients without a matched donor
Personalized Treatment Decision-Making
Deciding on treatment is all about you. We look at your health, what you want, and your goals. We work with you to create a plan that fits your needs.
The choice between BMT and immunosuppression depends on many things. We consider your health, donor options, and what you prefer. This way, we can choose the best treatment for you.
Living with Aplastic Anemia: Day-to-Day Management
Managing aplastic anemia daily is key to a better life for those affected. We’ll look at the main ways to handle this condition well.
Lifestyle Adjustments and Precautions
Living with aplastic anemia means big lifestyle changes to avoid problems. Patients need to watch their surroundings and daily actions closely. Staying away from crowded places and sick people helps prevent infections.
Good hygiene, like washing hands often, is also very important. It’s vital for patients to know about their condition and its treatment. Learning aboutaplastic anemia treatment options helps them make better care choices.
Preventing Infections and Bleeding
Stopping infections and bleeding is key in managing aplastic anemia. Patients should wear protective gear and be careful with sharp objects. They should also know the signs of infection or bleeding and get help fast if they see them.
- Practice good hygiene to prevent infections.
- Avoid contact with people who are sick.
- Use protective gear during activities that could cause injury.
- Monitor for signs of bleeding or infection.
Psychological Support and Resources
Dealing with aplastic anemia is tough, not just physically but emotionally, too. Psychological support is essential for managing stress and anxiety. Counseling, support groups, and connecting with others who face similar issues can help a lot.
A strong support system is very important for managing aplastic anemia daily. We suggest patients look for resources that offer emotional support and guidance on their journey.
Conclusion: The Future of Aplastic Anemia Treatment
Looking ahead, aplastic anemia treatment is set to improve. Advances in bone marrow transplant and immunosuppressive therapy have made a big difference. Bone marrow transplant, in particular, has changed how we treat severe aplastic anemia.
We expect more progress as research continues. New treatments and better transplant methods will help more patients. This brings hope to those dealing with aplastic anemia and their families.
Bone marrow transplant is now a key part of treatment for many. We look forward to even better treatments and new ways to fight this disease.
We’re excited about the future for those with aplastic anemia. Our goal is to keep improving care and support for patients worldwide. We’re committed to helping everyone affected by this condition.
FAQ
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make enough blood cells. This leads to health problems.
What does SAA stand for in medical terms?
SAA means Severe Aplastic Anemia. It’s when the bone marrow can’t make enough blood cells.
Is SAA a form of cancer?
No, SAA is not cancer. But it can have similar symptoms. It needs its own treatment.
What are the common symptoms of aplastic anemia?
Symptoms include feeling very tired, weak, and short of breath. You might also get sick more easily and bleed a lot.
How is aplastic anemia diagnosed?
Doctors use a blood test, bone marrow biopsy, and more tests to diagnose it. They check for other conditions too.
Is aplastic anemia curable?
Yes, it can be cured with the right treatment. A bone marrow transplant or immunosuppressive therapy can help.
What is the bone marrow transplant process for aplastic anemia?
First, find a bone marrow donor. Then, get ready for the transplant with conditioning therapy. The whole process takes time, depending on the person.
What are the possible complications after a bone marrow transplant?
Complications include graft-versus-host disease, infections, and damage to organs. It’s important to watch for these and get follow-up care.
How does immunosuppressive therapy work for aplastic anemia?
This therapy uses medicines to calm down the immune system. It helps the bone marrow recover and make blood cells again.
What lifestyle adjustments are necessary for living with aplastic anemia?
You should avoid infections, manage bleeding risks, and eat well. These steps help improve your health and quality of life.
What are the success rates for bone marrow transplant in treating aplastic anemia?
Success rates depend on the donor match and the patient’s health. New treatments have made outcomes better.
Can aplastic anemia be treated without a bone marrow transplant?
Yes, you can use immunosuppressive therapy instead. It’s an option when a transplant isn’t possible or preferred.
How do I choose between BMT and immunosuppressive therapy?
Your choice depends on your age, health, and whether you have a donor. It’s a personal decision based on your situation.
References
- Bacigalupo, A., & Bruno, B. (2015). Acquired bone marrow failure: Severe aplastic anemia. In Hematology/Oncology Clinics of North America (Vol. 29, Issue 2, pp. 471-487). https://www.ncbi.nlm.nih.gov/books/NBK608280/



































