Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know over 2 million endoscopic procedures happen every year in the U.S.? This shows how big a deal endoscopy in medical practice is. We need to get how endoscopy helps find and fix many stomach problems.
Endoscopy is key in gastrointestinal examination. It lets doctors do small, quick surgeries that help patients heal faster. But, the big question is: is endoscopy considered general surgery? We’ll look into this to clear things up.
Key Takeaways
- Endoscopy is a critical diagnostic and therapeutic tool in gastrointestinal medicine.
- The relationship between endoscopy and general surgery is complex and multifaceted.
- Understanding the role of endoscopy in general surgery can improve patient care.
- Endoscopic procedures are increasingly used in various medical specialties.
- The distinction between endoscopy and general surgery is not always clear-cut.
Understanding Endoscopy: Definition and Basic Concepts
Endoscopy is a medical technique that has grown a lot over time. It’s now key for checking and treating health issues. We’ll look at what endoscopy is, its history, and the tools used.
What Is an Endoscopic Procedure?
An endoscopic procedure uses a special tube with a camera and light. This tube lets doctors see inside the body without surgery. It’s used to check the digestive, respiratory, and urinary systems.
Key aspects of endoscopic procedures include:
- Minimally invasive, reducing recovery time
- Diagnostic capabilities, allowing for tissue sampling
- Therapeutic applications, enabling treatments such as polyp removal
History and Evolution of Endoscopy
The first endoscopes were made in the early 19th century. Technology has improved a lot, making endoscopy better for diagnosing and treating diseases.
Period | Development |
Early 19th Century | First endoscopes developed |
Late 20th Century | Introduction of flexible endoscopy |
21st Century | Advancements in high-definition imaging and capsule endoscopy |
Basic Equipment and Technology
Today’s endoscopy uses high-tech tools like cameras and monitors. The endoscope can be flexible or rigid, depending on the task. New tech includes capsule endoscopy and AI-assisted endoscopy.
New tech in endoscopy is making it even better for diagnosing and treating health issues.
The Scope of General Surgery
General surgery is a key part of medical care. It deals with many health issues. This field is broad and covers a lot of surgical procedures. It’s a base for other surgical areas and often the first stop for surgery needs.
Definition and Traditional Boundaries
General surgery traditionally covers the abdomen, breast, skin, and soft tissues. It’s a main part of hospital care. It handles emergencies and planned surgeries.
The field has changed over time. New tech and healthcare changes have shifted its focus. General surgeons used to do many types of surgeries, from simple to complex.
Modern General Surgery Practice
Today, general surgery keeps growing. It uses new tech and methods. It now includes special areas like surgical oncology and endocrine surgery.
Now, general surgery mixes old and new ways of operating. It uses laparoscopic and endoscopic methods. This makes treatments more precise and less invasive.
Core Procedures in General Surgery
General surgery includes many key operations. These include removing the appendix, gallbladder, and repairing hernias. These are key parts of a general surgeon’s training.
Procedure | Description | Common Indications |
Appendectomy | Surgical removal of the appendix | Appendicitis |
Cholecystectomy | Removal of the gallbladder | Gallstones, cholecystitis |
Hernia Repair | Surgical correction of a hernia | Inguinal, umbilical, or incisional hernias |
General surgery and endoscopy work together. Many general surgeons use endoscopy for diagnosis and treatment. This approach helps patients recover faster and improves their health outcomes.
Is Endoscopy Considered General Surgery?
To figure out if endoscopy is seen as general surgery, we need to look at its classification challenges. The lines between medical specialties are often fuzzy. Endoscopy is a great example of this.
Classification Challenges in Medical Specialties
Sorting out endoscopic procedures is tough for doctors. With new tech, these procedures are used in many fields. This makes it hard to decide where they fit.
Some big challenges are:
- Figuring out what general surgery covers
- Deciding which specialty endoscopy belongs to
- Handling areas where specialties overlap
Overlapping Domains Between Specialties
Endoscopy is used in many areas, like gastroenterology, pulmonology, and surgery. This mixing up can make it unclear if it’s part of general surgery.
For example, gastroenterologists do endoscopies for checking and treating. Surgeons also use it in surgeries. This shows we need clear rules on how to classify it.
Historical Development of Specialty Boundaries
The growth of medical specialties has shaped how we classify endoscopy. New tech and techniques change how we work, sometimes causing disagreements between doctors.
Knowing this history helps us see why classifying endoscopy is tricky. It also shows why working together across specialties is key.
Important things that have shaped specialty boundaries include:
- New medical tech
- Changes in how doctors are trained
- Updates in how we practice and follow guidelines
Looking at these points helps us understand the fine details of endoscopy’s classification and its tie to general surgery.
Endoscopy Across Medical Specialties
Endoscopy is now a key tool in many areas of medicine. It’s used in different fields for both diagnosis and treatment. This makes it very important in healthcare today.
Gastroenterology and Endoscopy
In gastroenterology, endoscopy is very important. It helps find and treat problems in the stomach and intestines. Tests like colonoscopy and EGD are used to find cancers early and manage long-term issues.
Endoscopy has greatly helped patients in gastroenterology. It allows for precise treatments like removing polyps and opening narrow areas.
Pulmonology and Bronchoscopy
Pulmonology uses endoscopy through bronchoscopy. This lets doctors look at the airways and lungs. It’s key for finding lung diseases like infections and cancers.
Through bronchoscopy, doctors can take tissue samples, remove objects, and do treatments. This is very important for lung health.
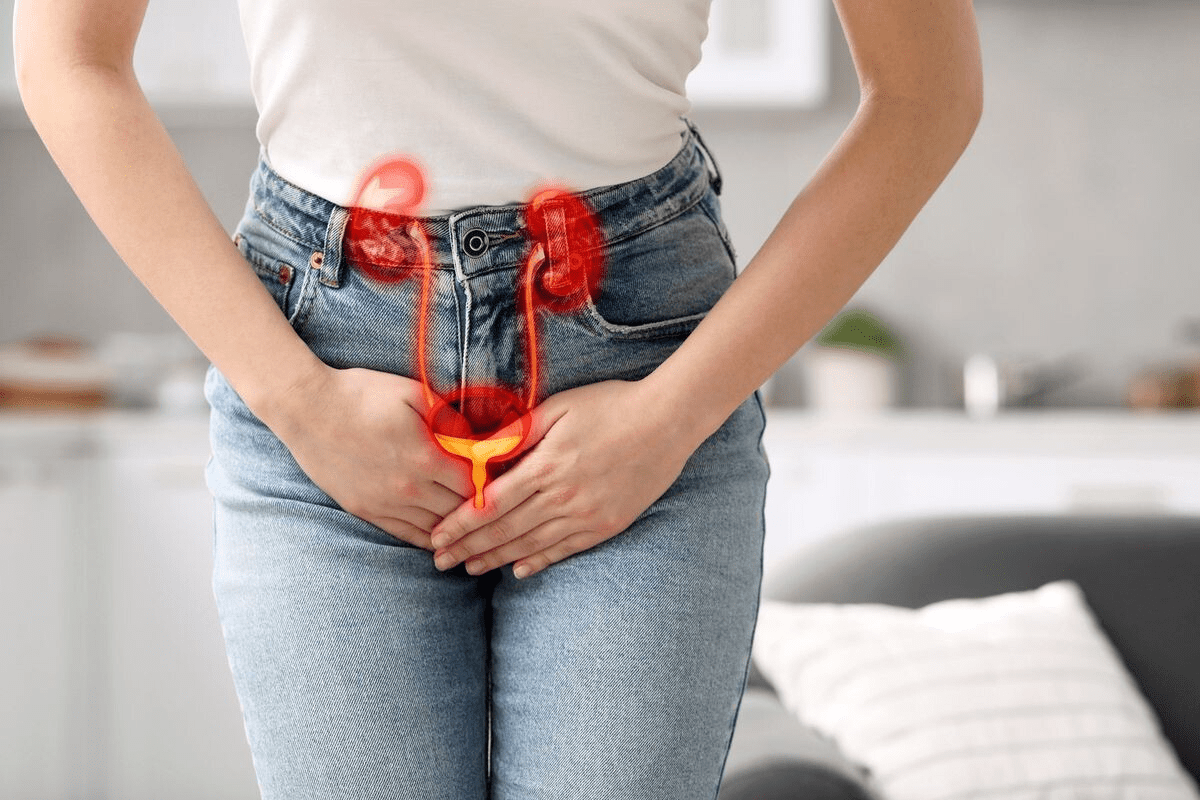
Urology and Cystoscopy
In urology, cystoscopy is a main endoscopy tool. It lets doctors see inside the bladder and urethra. This is vital for finding and treating problems like bladder stones and tumors.
Cystoscopy helps urologists see the urinary tract clearly. They can do biopsies and surgeries without big cuts. This makes recovery faster for patients.
ENT and Laryngoscopy
Otolaryngology (ENT) uses endoscopy, mainly laryngoscopy, to check the larynx and vocal cords. This is key for diagnosing voice issues and throat problems.
Laryngoscopy lets ENT doctors see the larynx closely. They can find problems like cancer and decide on treatments.
Endoscopy is widely used in many medical fields. It helps doctors diagnose and treat patients in a less invasive way. This improves care and results in many areas of medicine.
Types of Endoscopic Procedures
Endoscopy is very versatile, used for both diagnosis and treatment. It’s a key part of modern medicine, providing many options for doctors and patients.
Diagnostic Endoscopy
Diagnostic endoscopy lets doctors see inside the body. It helps find problems early. This is often the first step in figuring out how to treat a patient.
Diagnostic endoscopy gives doctors a direct look at the body’s inside. This can reveal things that other tests can’t.
Therapeutic Endoscopy
Therapeutic endoscopy is for treating medical issues. It includes removing polyps, widening narrow areas, and stopping bleeding. Therapeutic endoscopy is a less invasive way to treat problems, leading to faster recovery and fewer side effects.
Interventional Endoscopy
Interventional endoscopy is more advanced. It involves complex procedures like ERCP and EUS-FNA. These need special training and tools, showing how endoscopy is getting better.
In summary, the variety of endoscopic procedures shows big progress in medicine. From diagnostic endoscopy to interventional endoscopy, these methods are key in patient care. They offer effective, less invasive ways to improve health and life quality.
Endoscopy in Surgical Practice
Endoscopy is key in surgery, helping with both diagnosis and treatment. It’s used before, during, and after surgery to improve patient care.
Pre-Surgical Diagnostic Applications
Before surgery, endoscopy helps a lot. It lets surgeons see inside the body to find problems and plan the best surgery. Pre-surgical endoscopy can avoid more risky tests, making recovery faster.
Endoscopy often changes the surgery plan. For example, in stomach surgery, it finds issues that imaging can’t. This is very helpful.
Intraoperative Endoscopy
During surgery, intraoperative endoscopy gives a live view of the area being worked on. This is very useful in tricky surgeries. It helps surgeons see everything clearly and check their work as they go.
This method helps avoid problems and makes sure the surgery is a success. It leads to better results and fewer complications.
Post-Surgical Follow-up and Surveillance
After surgery, post-surgical endoscopy checks on how the body is healing. It spots any issues early and deals with them quickly. It can also remove stitches or widen narrowed areas.
Using endoscopy after surgery helps patients recover faster. It makes sure they don’t need more surgeries. It’s a safe way to keep an eye on patients long-term.
Adding endoscopy to surgery makes care more precise and less invasive. As technology gets better, endoscopy will play an even bigger role in surgery. It will help doctors diagnose and treat better.
Training and Certification for Endoscopy
To master endoscopy, doctors must go through tough training and get certified. This training is key to making sure they can do these procedures well and safely.
General Surgery Residency Training
General surgery residency teaches the basics of surgery, including endoscopy. Doctors learn how to assess patients, prepare for surgery, and care for them after. Endoscopy training during residency also covers when to use endoscopy, when not to, and possible problems.
- Basic surgical skills
- Patient assessment and care
- Introduction to endoscopic techniques
Gastroenterology Fellowship Training
Gastroenterology fellowship is for learning about GI disorders with endoscopy. Fellows get a lot of practice in different endoscopy procedures. Advanced training in gastroenterology helps them handle tough GI cases.
- Diagnostic endoscopy
- Therapeutic endoscopy
- Advanced endoscopic techniques
Advanced Endoscopy Fellowships
Advanced endoscopy fellowships offer more training in complex procedures. These include endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS). Doctors get a lot of practice and learn to handle hard cases.
Board Certification Requirements
Getting certified is a big step in proving a doctor’s skill in endoscopy. Doctors must pass a big exam that tests their knowledge and skills. Maintaining certification means keeping up with education and following professional rules.
- Comprehensive examination
- Ongoing education requirements
- Adherence to professional standards
In summary, getting good at endoscopy needs a lot of training and certification. Doctors need to go through general surgery, gastroenterology fellowship, and advanced endoscopy training. They also need to get certified. This way, they can give the best care to their patients.
Endoscopy vs. Other Surgical Approaches
When looking at surgical options, it’s key to know the differences between endoscopy and other methods. Surgery has changed a lot, with many techniques now available. Each one meets different needs and conditions.
Endoscopy vs. Laparoscopy: Key Differences
Endoscopy and laparoscopy are both minimally invasive. But they work in different ways. Endoscopy uses a tube with a camera and light through a small opening. Laparoscopy makes small cuts in the belly to insert tools.
Endoscopy is less invasive and often used for checks or simple treatments. Laparoscopy is for more detailed surgeries, like removing the gallbladder or doing a hysterectomy.
Characteristics | Endoscopy | Laparoscopy |
Invasiveness | Less invasive, often through natural orifices | More invasive, requires small abdominal incisions |
Primary Use | Diagnostic and minor therapeutic procedures | Complex surgeries like gallbladder removal |
Recovery Time | Generally quicker recovery | Recovery time varies based on the procedure |
Endoscopy vs. Open Surgery: Advantages and Limitations
Endoscopy and open surgery are at opposite ends of the surgical spectrum. Open surgery uses a big cut for direct access. It’s more invasive, leading to longer healing times and bigger scars.
Endoscopy is less invasive, with benefits like less risk of problems, less pain, and faster healing. But, it can’t reach all areas and needs special tools and training.
The Spectrum of Minimally Invasive Procedures
Minimally invasive methods, like endoscopy and laparoscopy, have changed surgery a lot. They reduce harm to the patient and improve looks. Knowing about these options helps pick the best treatment.
Every patient is different, and the right choice depends on their health, the condition, and the surgeon’s skills.
Endoscopy in Various Healthcare Settings
Endoscopy is used in many healthcare places, like hospitals and centers for outpatient surgery. This makes it easy for doctors to do endoscopies in different places. It helps meet the needs and wishes of patients.
Operating Room Endoscopy
Endoscopy in the operating room means using endoscopes during surgery. It lets surgeons do small, less invasive surgeries. This means patients heal faster and have less scarring.
- Operating room endoscopy lowers the chance of problems and speeds up recovery.
- It lets surgeons see what they’re doing in real time, making them more precise.
Ambulatory Surgery Centers
Ambulatory surgery centers (ASCs) are a good choice for endoscopies. They are set up for surgeries that don’t need a long hospital stay. This makes things easier and cheaper for patients.
ASCs have the latest facilities and are staffed by experts. They make sure patients get great care. The efficiency and safety of endoscopies here are big pluses for patients.
Office-Based Endoscopy
Office-based endoscopy is becoming more common. It lets doctors do simple endoscopies in their offices. This makes things easier for patients.
Setting | Advantages | Limitations |
Hospital-Based | Advanced equipment, trained staff | Higher costs, longer waits |
Office-Based | Convenient, cost-effective | Limited equipment, possible complications |
In conclusion, endoscopy is used in many places, each with its own good points and challenges. Knowing these helps doctors give the best care to their patients.
Coding and Billing Classification of Endoscopy
Classifying endoscopy in medical coding and billing is complex but vital. Healthcare providers use endoscopic procedures for both diagnosis and treatment. It’s key to understand the coding and billing for these services.
CPT Coding for Endoscopic Procedures
CPT coding for endoscopy requires picking the right codes for the procedure. These codes are specific to the type of endoscopy, the body part examined, and any interventions. For example, gastrointestinal endoscopy codes depend on the examination’s extent and any additional procedures like biopsy or polypectomy.
“Accurate CPT coding is vital for correct reimbursement of healthcare services,” highlights the need for precise coding in endoscopic procedures.
Surgical vs. Medical Billing Considerations
Deciding if an endoscopic procedure is surgical or medical billing depends on several factors. These include the procedure’s purpose, where it was done, and the patient’s condition. Surgical billing is for more invasive procedures or those in an operating room. Medical billing is for diagnostic endoscopies or procedures in an outpatient setting.
- Surgical endoscopy codes often include diagnostic endoscopy codes.
- Medical billing for endoscopy requires accurate documentation of the procedure and the patient’s diagnosis.
Insurance Coverage and Reimbursement
Insurance coverage for endoscopic procedures varies by payer and procedure. It’s important for healthcare providers to understand the coverage policies of different insurance providers. Factors affecting reimbursement include the procedure’s medical necessity, the provider’s network status, and the patient’s out-of-pocket costs.
Key considerations for insurance coverage include:
- Pre-authorization requirements for certain procedures.
- Documentation of medical necessity.
- Compliance with payer-specific coding and billing guidelines.
Understanding the latest guidelines and payer policies is essential for accurate reimbursement and avoiding financial risks in endoscopy coding and billing.
Clinical Guidelines and Standards for Endoscopy
Clinical guidelines for endoscopy are key to ensuring quality and safety in GI procedures. These guidelines, made by professional groups, help standardize care and improve patient results.
American College of Gastroenterology Guidelines
The American College of Gastroenterology (ACG) sets guidelines for gastroenterology, including endoscopy. These guidelines cover many areas, like when to use endoscopy, how to prepare patients, and care after the procedure. For example, the ACG gives detailed advice on when to do follow-up colonoscopies for those with polyps or cancer.
Key Recommendations:
- Surveillance colonoscopy intervals based on polyp characteristics
- Guidelines for the management of Barrett’s esophagus
- Recommendations for the diagnosis and treatment of gastrointestinal bleeding
American Society for Gastrointestinal Endoscopy Standards
The American Society for Gastrointestinal Endoscopy (ASGE) focuses on endoscopy practice. They set standards for training, equipment, and quality checks. The ASGE guidelines cover topics like when to use endoscopic ultrasound and how to handle complications.
“The ASGE guidelines on quality indicators for endoscopy are key for maintaining high standards in GI endoscopy.” –
ASGE President
American College of Surgeons Recommendations
The American College of Surgeons (ACS) also offers recommendations for endoscopy, mainly for surgical practices. The ACS guidelines often focus on how to integrate endoscopy with surgery, including before and after surgery care.
Quality Metrics and Benchmarks
Quality metrics and benchmarks are vital for checking endoscopic procedure performance. These include things like adenoma detection rate, cecal intubation rate, and complication rates. By monitoring these, healthcare providers can spot areas for betterment and enhance their endoscopy practices.
- Adenoma Detection Rate (ADR)
- Cecal Intubation Rate
- Withdrawal Time
- Complication Rates
By following these clinical guidelines and standards, healthcare providers can make sure their endoscopy practices are top-notch. This leads to better results for patients.
The Future of Endoscopy in Surgical Practice
Endoscopy is on the verge of a new era, thanks to innovations that will improve surgical results. Several key areas are emerging that will shape the future of endoscopy in surgery.
Technological Advancements in Endoscopic Equipment
New endoscopic equipment is a key factor in the evolution of endoscopy. High-definition imaging and 3D visualization are becoming more common. They give surgeons clearer views of the operating area.
Advances in flexible endoscopy and robotic-assisted endoscopy are also expanding what’s possible in complex procedures.
These advancements are making endoscopic procedures more precise and safer for patients. For example, augmented reality is being used to improve navigation and visualization in complex surgeries.
Artificial Intelligence and Computer-Assisted Endoscopy
The use of Artificial Intelligence (AI) and computer-assisted technologies is changing endoscopy. AI can detect abnormalities like polyps or lesions during exams, improving accuracy. Computer-assisted endoscopy also helps with more precise control of instruments, reducing complications.
AI can also predict patient outcomes and tailor treatment plans based on data. This is done using historical data and real-time information during procedures.
Expanding Applications and Novel Procedures
The future of endoscopy includes new procedures and expanded uses of existing ones. For example, endoscopic submucosal dissection is now allowing for more complex resections endoscopically. The exploration of natural orifice transluminal endoscopic surgery (NOTES) also offers less invasive options.
As these technologies and techniques evolve, we’ll see more conditions treated endoscopically. This could reduce the need for more invasive surgeries.
Patient Considerations for Endoscopic Procedures
When thinking about endoscopic procedures, patients need to know a few important things. These procedures are a big step forward in medicine. They offer a less invasive way to treat health issues compared to traditional surgery.
Benefits of Endoscopic Approaches
Endoscopic methods have many advantages. They lead to less recovery time, less pain after surgery, and little to no scarring. Patients can usually get back to their daily activities faster than with traditional surgery. Plus, endoscopy can help diagnose and treat problems, making it a flexible tool in healthcare.
- Minimally invasive, resulting in less tissue damage
- Reduced risk of complications compared to open surgery
- Shorter hospital stays and recovery periods
- Ability to perform procedures on an outpatient basis
Risks and Possible Complications
Even though endoscopic procedures are safe, there are risks and complications to be aware of. These can include bleeding, infection, and organ perforation. While these are rare, they can be serious and might need more medical care.
- Bleeding or hemorrhage during or after the procedure
- Infection, either localized or systemic
- Perforation of the organ, potentially requiring surgical repair
Preparation and Recovery Expectations
Getting ready for an endoscopic procedure is key. Patients often have to follow special diets and adjust their medicines. After the procedure, some discomfort is normal but can be managed with medication. Knowing what to expect can help patients prepare better.
Choosing Between Endoscopic and Surgical Options
The decision between endoscopic and surgical options depends on several factors. These include the condition being treated, the patient’s health, and the risks and benefits of each method. We help patients choose the best option based on their needs and preferences.
Understanding the benefits, risks, and what to expect from endoscopic procedures helps patients make informed choices. Our goal is to support patients fully during their treatment, aiming for the best results.
Endoscopy Privileges and Credentialing
Getting endoscopy privileges involves several important steps. Healthcare professionals must go through a detailed process to show they can do these procedures well. Credentialing for endoscopy is serious. It checks if a doctor is really good at doing endoscopic exams and treatments.
Hospital Credentialing Requirements
To get endoscopy privileges, a doctor’s background is carefully checked. This includes their medical degree, residency, and any fellowships. Credentialing committees look at how much experience a doctor has with endoscopy. They check how many procedures they’ve done and how they turned out. This makes sure only the right doctors can do endoscopy.
Volume Requirements and Maintaining Competency
Doctors need to do a certain number of endoscopy procedures to keep their privileges. This shows they’re good at it. Staying good at endoscopy is key. Hospitals check this to make sure doctors know the latest methods and tools.
Cross-Specialty Considerations and Turf Battles
When doctors get endoscopy privileges, there can be issues between specialties. Gastroenterology and surgery might both want to do endoscopy. Credentialing committees have to figure out who gets to do what. They look at who’s best for each type of procedure, not just who’s in which specialty.
Privileging Challenges for New Procedures
New endoscopy procedures and tools bring new challenges. Credentialing groups have to set up rules for these. They need to decide how to check if doctors are ready. This is a tough job that needs teamwork between different doctors and groups to make sure rules are fair and right.
Conclusion
Endoscopy plays a big role in general surgery, but it’s more than that. It has grown to be key in many medical fields like gastroenterology, pulmonology, and urology. This shows how endoscopy has become a vital tool in healthcare.
Endoscopy is not just for looking inside the body. It’s also used to treat problems. It helps doctors before, during, and after surgery. This makes patient care better and less invasive.
In summary, endoscopy is not just for general surgery. It’s used in many areas of medicine. Knowing how endoscopy works is important for doctors to improve patient care.
As technology gets better, endoscopy will too. We can expect even more advanced and less invasive procedures. This will make endoscopy even more important in surgery.
FAQ
Is endoscopy considered a part of general surgery?
Yes, endoscopy is often part of general surgery. Surgeons use it to examine internal organs and treat conditions using minimally invasive techniques. However, its classification can vary depending on the specialty and the specific procedure.
What is the difference between diagnostic and therapeutic endoscopy?
Diagnostic endoscopy helps doctors view internal organs to identify medical conditions.
Therapeutic endoscopy goes a step further, allowing doctors to perform treatments such as removing growths, stopping bleeding, or widening narrowed passages.
What are the benefits of endoscopic procedures compared to open surgery?
Endoscopy offers several benefits over open surgery. It is less invasive, causes minimal tissue damage, results in faster recovery, reduces pain, lowers the risk of complications, and leaves smaller or no visible scars.
What kind of training is required to perform endoscopic procedures?
Doctors performing endoscopy undergo specialized training that includes theoretical learning, hands-on practice, and supervised procedures. General surgeons typically learn endoscopy during residency, while gastroenterologists receive advanced training during fellowship.
What are the risks and possible complications of endoscopic procedures?
Endoscopy is generally safe, but possible risks include bleeding, infection, organ injury, and reactions to anesthesia or sedation. Complications are rare and depend on the procedure type and patient’s health.
How are endoscopic procedures coded and billed for insurance purposes?
Endoscopic procedures are assigned CPT (Current Procedural Terminology) codes based on the type of procedure performed. Billing classification may differ depending on whether it is considered a medical or surgical service, influencing insurance coverage.
What are the current clinical guidelines for endoscopy?
Clinical guidelines are provided by professional organizations such as the American College of Gastroenterology (ACG) and American Society for Gastrointestinal Endoscopy (ASGE). These cover quality standards, patient preparation, safety, and procedural best practices.
How is artificial intelligence being integrated into endoscopy?
Artificial Intelligence (AI) is increasingly used in endoscopy to enhance image analysis, improve detection of abnormalities, and assist with real-time decision-making during procedures. AI helps increase diagnostic accuracy and efficiency.
What is the future of endoscopy in surgical practice?
The future of endoscopy involves advanced imaging, robotic assistance, and AI-powered diagnostics. These innovations promise greater precision, minimally invasive treatments, and improved patient outcomes in surgical care.
How do healthcare settings impact the delivery of endoscopic services?
The quality, cost, and accessibility of endoscopic procedures vary by setting — hospitals, outpatient centers, or specialized clinics. Each environment offers different advantages in terms of technology, staffing, and patient comfort.
What are the requirements for obtaining endoscopy privileges?
Physicians must complete accredited training, demonstrate competence, and meet case volume requirements to obtain endoscopy privileges. Hospitals and clinics set specific credentialing criteria depending on the specialty and procedure type.
References
National Center for Biotechnology Information. Endoscopy in surgery. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10233939/