Last Updated on November 26, 2025 by Bilal Hasdemir

Nearly 1 in 8 men will be diagnosed with prostate cancer in their lifetime, making the decision to undergo prostate removal surgery a critical one. Explore if is prostate surgery worth it based on age, cancer stage, risks, and long-term health improvements.
For those diagnosed, understanding the benefits of prostatectomy is crucial. This surgery can potentially save lives by removing cancerous tissues. However, it’s also important to consider the risks associated with prostate removal surgery, such as incontinence and impotence.
Weighing these factors is essential to making an informed decision. As we explore the intricacies of prostate surgery, it’s vital to examine both the positive outcomes and potential complications.
Key Takeaways
- Prostate cancer affects nearly 1 in 8 men in their lifetime.
- Prostatectomy can be a life-saving surgery by removing cancerous tissues.
- Risks of prostate removal surgery include incontinence and impotence.
- Understanding the benefits and risks is crucial for making an informed decision.
- Men diagnosed with prostate cancer should carefully weigh their treatment options.
Understanding Prostate Cancer and Surgical Intervention
Understanding the intricacies of prostate cancer is crucial for patients and healthcare providers to make informed decisions about surgical intervention. Prostate cancer, like many other cancers, varies significantly in its presentation and severity, influencing the choice of treatment.
Types of Prostate Cancer and Their Severity
Prostate cancer is not a single disease but encompasses several types, with adenocarcinoma being the most common, accounting for about 90% of cases. The severity and aggressiveness of prostate cancer are determined by the cancer’s grade and stage. The Gleason score is a critical tool used to grade prostate cancer based on the tumor’s microscopic appearance, helping predict the disease’s aggressiveness.
The stage of prostate cancer, which describes the extent of the cancer’s spread, is another vital factor in determining the severity. Early-stage prostate cancer is often localized within the prostate, making it potentially more treatable, whereas advanced prostate cancer has spread beyond the prostate, complicating treatment.
When Surgery Becomes a Consideration
Surgery becomes a consideration for prostate cancer treatment based on several factors, including the cancer’s stage, grade, and the patient’s overall health and preferences. For men with localized prostate cancer that is considered intermediate or high-risk, radical prostatectomy, or surgical removal of the prostate, is often recommended as a potentially curative treatment.
The decision to undergo surgery involves weighing the potential benefits against the risks and side effects. It’s a decision that should be made after thorough consultation with a healthcare provider, considering the individual’s specific circumstances and the latest evidence on prostatectomy success rates.
Different Types of Prostate Surgery Procedures
The treatment of prostate cancer can involve various surgical procedures, each with its unique benefits and drawbacks. Understanding these differences is crucial for patients to make informed decisions about their care.
Radical Prostatectomy
Radical prostatectomy involves the surgical removal of the prostate gland and some surrounding tissue. This procedure is often recommended for patients with localized prostate cancer. The goal is to remove the cancer entirely, potentially curing the disease. There are different approaches to radical prostatectomy, including open, laparoscopic, and robotic-assisted techniques.
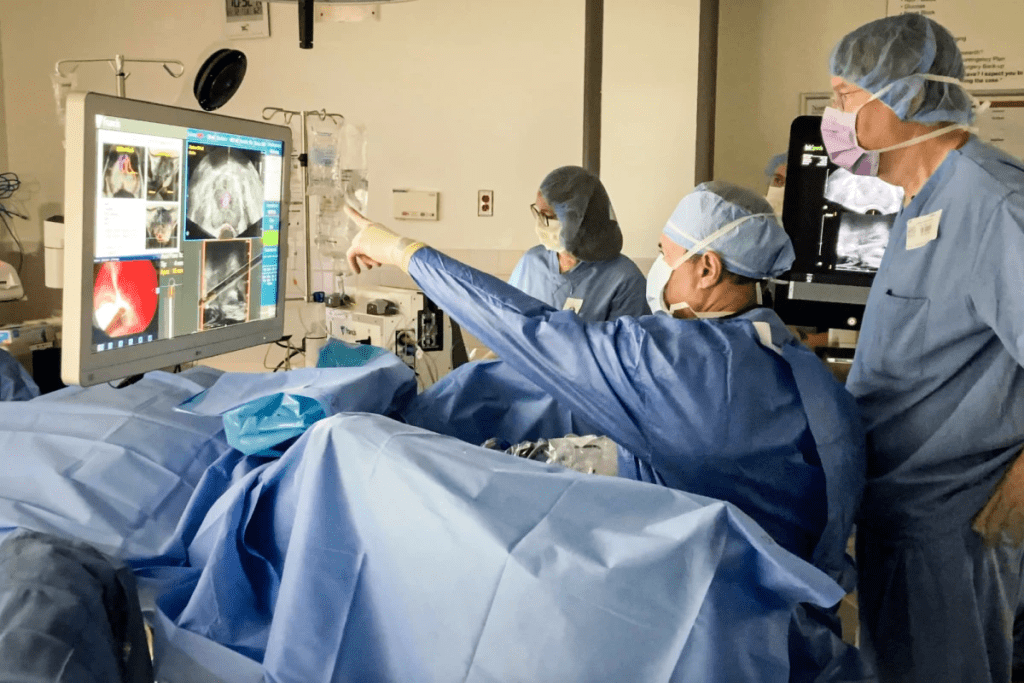
Robotic-Assisted Laparoscopic Prostatectomy
Robotic-assisted laparoscopic prostatectomy is a minimally invasive surgical technique that utilizes a robotic system to assist the surgeon. This approach offers enhanced precision, flexibility, and a clearer view of the surgical area. Benefits include smaller incisions, less blood loss, and potentially quicker recovery times compared to traditional open surgery.
Open Prostatectomy
Open prostatectomy involves a larger incision to access the prostate gland directly. While this traditional method is more invasive than robotic or laparoscopic approaches, it is still a viable option for certain patients, particularly those with more complex cases or when other techniques are not feasible.
| Surgical Procedure | Key Characteristics | Potential Benefits |
| Radical Prostatectomy | Removal of prostate gland and surrounding tissue | Potential cure for localized prostate cancer |
| Robotic-Assisted Laparoscopic Prostatectomy | Minimally invasive, robotic assistance | Less blood loss, quicker recovery, enhanced precision |
| Open Prostatectomy | Traditional, more invasive approach | Viable for complex cases, direct access to prostate |
Each of these surgical procedures has its indications, benefits, and potential side effects. Understanding the specifics of each can help patients and their healthcare providers make the most appropriate choice based on individual circumstances.
The Benefits of Prostatectomy
Prostatectomy, or the surgical removal of the prostate gland, offers numerous benefits for patients diagnosed with prostate cancer. This surgical intervention is a significant consideration for men facing a prostate cancer diagnosis, as it can potentially eliminate the cancer and improve survival rates.
Cancer Control and Survival Rates
One of the primary benefits of prostatectomy is its impact on cancer control and survival rates. Studies have shown that surgical removal of the prostate can significantly reduce the risk of cancer recurrence, thereby improving long-term survival rates for patients. The effectiveness of prostatectomy in controlling cancer is a crucial factor in the decision-making process for many men diagnosed with prostate cancer.
Research indicates that patients who undergo prostatectomy often experience improved cancer-specific survival rates compared to those who opt for other treatment modalities. This is particularly true for men with localized prostate cancer, where surgery can be curative.
Psychological Benefits of Complete Tumor Removal
Beyond the physical benefits, prostatectomy also offers psychological benefits associated with the complete removal of the tumor. For many patients, the knowledge that the cancerous prostate gland has been removed can provide a significant sense of relief and reduce anxiety related to cancer recurrence.
The psychological impact of undergoing a prostatectomy should not be underestimated. The removal of the cancerous gland can lead to improved mental well-being and a better quality of life post-surgery. Patients often report feeling more in control of their health and more optimistic about their future following the procedure.
Potential Risks and Complications
Understanding the potential risks and complications of prostate surgery is crucial for patients considering this treatment option. Prostatectomy, like any major surgery, involves risks that can affect a patient’s quality of life both in the short and long term.
Short-Term Surgical Complications
Short-term complications following prostate surgery can include infection, bleeding, and reactions to anesthesia. These risks are generally associated with any surgical procedure and are managed with appropriate medical care.
Common short-term complications:
- Infection
- Bleeding or hemorrhage
- Adverse reactions to anesthesia
- Blood clots
As noted by a study published in the Journal of Urology, “The incidence of complications after radical prostatectomy has decreased over the years due to improvements in surgical techniques and perioperative care.”
“The incidence of complications after radical prostatectomy has decreased over the years due to improvements in surgical techniques and perioperative care.”
Journal of Urology
Long-Term Health Implications
Long-term health implications of prostate surgery can be significant and include issues such as erectile dysfunction and urinary incontinence. These complications can have a lasting impact on a patient’s quality of life.
| Complication | Incidence Rate | Management Strategies |
| Erectile Dysfunction | Up to 80% in some studies | Medications, penile implants, vacuum devices |
| Urinary Incontinence | Varied, but significant improvement over time | Pelvic floor exercises, surgery, absorbent products |
It’s essential for patients to discuss these potential complications with their healthcare provider to understand the risks and benefits associated with prostate surgery.
Is Prostate Surgery Worth It? Weighing the Evidence
The decision to undergo prostate surgery is multifaceted, involving a careful weighing of benefits and risks. This section aims to provide a balanced view by examining the evidence regarding the worth of prostate surgery, focusing on success rates and factors that influence outcomes.
Success Rates Across Different Patient Profiles
Prostate surgery, or prostatectomy, is a significant treatment option for prostate cancer. Its success can vary based on several factors, including the patient’s overall health, the stage of cancer, and the surgical technique used.
Success rates across different patient profiles show variability. For instance, men with localized prostate cancer tend to have higher success rates with surgery compared to those with more advanced cancer.
Studies have shown that men with low-risk prostate cancer have excellent long-term cancer control rates after surgery, with some studies indicating rates as high as 90% or more at 10 years post-surgery.
In contrast, men with high-risk prostate cancer may have lower success rates, necessitating additional treatments such as radiation therapy or hormone therapy.
Factors That Influence Surgical Outcomes
Several factors can influence the outcome of prostate surgery. These include the surgeon’s experience, the surgical technique used, and the patient’s pre-operative health status.
For example, robotic-assisted laparoscopic prostatectomy has been associated with fewer complications and quicker recovery times compared to traditional open prostatectomy.
In conclusion, whether prostate surgery is worth it depends on individual circumstances, including the patient’s health profile and the specifics of their cancer. By understanding success rates and the factors that influence surgical outcomes, patients can make more informed decisions about their treatment.
Quality of Life After Prostatectomy
Quality of life after prostatectomy is a multifaceted concept that encompasses physical recovery, emotional adjustment, and psychological well-being. As patients navigate the post-surgical period, understanding these aspects can help manage expectations and improve outcomes.
Physical Recovery Timeline
The physical recovery timeline following a prostatectomy varies among individuals. Generally, patients can expect to return to their normal activities within a few weeks to a couple of months. However, full recovery, including the return of urinary continence and sexual function, may take longer.
Key milestones in the physical recovery process include:
- Immediate post-surgery recovery (1-2 weeks)
- Return to light activities (2-4 weeks)
- Resumption of strenuous activities (6-12 weeks)
As one patient noted, “The first few weeks were challenging, but with each passing day, I felt stronger and more like myself.” This sentiment is echoed by many who undergo the procedure, highlighting the importance of a supportive care network during this period.
Emotional and Psychological Adjustment
The emotional and psychological adjustment post-prostatectomy is just as crucial as physical recovery. Patients may experience a range of emotions, from relief to anxiety about their cancer status and future health.
Strategies for coping with emotional and psychological challenges include:
- Counseling or therapy to address anxiety or depression
- Support groups to share experiences with others
- Open communication with healthcare providers about concerns and fears
“After my surgery, I joined a support group, and it was incredibly helpful to hear others’ stories and know I wasn’t alone,” shared a prostate cancer survivor. Such testimonials underscore the value of emotional support in the recovery journey.
By understanding the quality of life after prostatectomy, patients can better prepare for the journey ahead, leveraging the support of healthcare professionals, family, and peers to navigate the challenges and triumphs that lie within.
Urinary Incontinence After Prostate Surgery
The risk of urinary incontinence after prostate surgery is a significant consideration for patients and healthcare providers alike. Urinary incontinence, or the loss of bladder control, is a potential side effect that can impact a patient’s quality of life post-operatively.
Incidence Rates and Duration
Studies have shown that the incidence of urinary incontinence after prostate surgery varies. Early incontinence is common immediately after surgery, but for many men, continence improves over time. Research indicates that at 1-year post-surgery, a significant percentage of men regain full continence.
- Short-term incontinence: Most men experience some level of incontinence immediately following prostate surgery.
- Long-term incontinence: The percentage of men with persistent incontinence decreases over time, with a smaller percentage experiencing long-term issues.
Management Strategies and Treatments
Fortunately, there are several management strategies and treatments available for urinary incontinence after prostate surgery. These include:
- Pelvic floor exercises, such as Kegel exercises, to strengthen the muscles that control urination.
- Behavioral therapy, which may involve bladder training and lifestyle modifications.
- Medical devices, like penile clamps or urinary catheters, for managing incontinence.
- Surgical interventions, including the implantation of an artificial urinary sphincter, for severe cases.
It’s essential for patients to discuss their individual situation and the best management strategies with their healthcare provider. With the right approach, many men are able to manage or overcome urinary incontinence after prostate surgery.
Sexual Function and Erectile Dysfunction Following Surgery
Understanding the effects of prostate surgery on sexual health is essential for men preparing for this operation. Prostate surgery, a common treatment for prostate cancer, can have significant implications for a man’s sexual well-being.
Prevalence of Erectile Dysfunction Post-Surgery
Erectile dysfunction (ED) is a well-documented potential complication following prostate surgery. Studies indicate that the prevalence of ED after prostatectomy varies widely, influenced by factors such as the surgical technique used, the patient’s age, and preoperative erectile function.
The risk of developing ED is a significant concern for men undergoing prostate surgery. It is crucial for patients to discuss their individual risk factors with their healthcare provider to understand what to expect.
Treatment Options for Restoring Sexual Function
Fortunately, various treatment options are available to help restore sexual function in men who have undergone prostate surgery. These include:
- Phosphodiesterase type 5 inhibitors (PDE5 inhibitors), such as sildenafil, which can help improve erectile function.
- Vacuum erection devices, which are non-invasive and can be effective.
- Penile implants, a more invasive option considered when other treatments fail.
Each treatment has its benefits and drawbacks, and what works for one patient may not work for another. A healthcare provider can help determine the most appropriate treatment based on individual health status and preferences.
Timeline for Potential Recovery
The timeline for recovering sexual function after prostate surgery can vary significantly among individuals. Some men may experience a return of erectile function within a few months, while for others, it may take longer.
Factors influencing the recovery timeline include the extent of nerve damage during surgery, the patient’s overall health, and the effectiveness of any treatments used to address ED. Patience and ongoing communication with a healthcare provider are key during this period.
Robotic Prostatectomy Outcomes and Advantages
Robotic prostatectomy has emerged as a significant advancement in the surgical treatment of prostate cancer, offering several benefits over traditional methods. This technique involves the use of a robotic system to assist the surgeon during the procedure, enhancing precision and reducing the risk of complications.
The advantages of robotic prostatectomy are multifaceted, including less blood loss, reduced risk of infection, and shorter hospital stays compared to open prostatectomy. These benefits contribute to a quicker recovery and less post-operative pain for patients.
Comparison to Traditional Open Surgery
When comparing robotic prostatectomy to traditional open surgery, several key differences emerge. Robotic surgery is minimally invasive, utilizing smaller incisions than those required for open surgery. This results in less tissue damage and trauma to the patient, leading to faster healing times.
- Reduced recovery time
- Less post-operative pain
- Improved precision during surgery
- Lower risk of complications
Studies have shown that robotic prostatectomy can lead to improved outcomes in terms of cancer control and reduced risk of urinary incontinence and erectile dysfunction, although results can vary based on the surgeon’s experience and patient-specific factors.
Learning Curve for Surgeons
The learning curve for surgeons adopting robotic prostatectomy is a critical consideration. While robotic systems offer advanced capabilities, mastering their use requires significant training and experience. Surgeons must undergo extensive practice to become proficient in robotic prostatectomy, as the technique demands a high level of dexterity and familiarity with the robotic interface.
To mitigate the risks associated with the learning curve, many institutions provide comprehensive training programs for surgeons. These programs include hands-on experience and mentorship, helping to ensure that surgeons are adequately prepared to perform robotic prostatectomies effectively.
As robotic technology continues to evolve, the outcomes for patients undergoing robotic prostatectomy are expected to improve, making it an increasingly viable option for those diagnosed with prostate cancer.
Prostate Surgery vs. Radiation Therapy: Comparative Outcomes
The decision between prostate surgery and radiation therapy is complex, involving considerations of cancer control, potential side effects, and overall quality of life. Both treatments are effective for prostate cancer, but they have different approaches and outcomes.
Efficacy in Cancer Control
Studies have shown that both surgery and radiation therapy can be effective in controlling prostate cancer. A key factor is the stage and aggressiveness of the cancer.
- Surgery is often preferred for patients with localized cancer that has not spread beyond the prostate.
- Radiation therapy can be used for localized cancer as well as for cases where the cancer has spread to surrounding tissues.
According to a study published in the Journal of Clinical Oncology, both radical prostatectomy and radiation therapy achieved similar cancer control outcomes for patients with high-risk prostate cancer.
Side Effect Profiles
The side effects of prostate surgery and radiation therapy can differ significantly.
- Prostate surgery can lead to urinary incontinence and erectile dysfunction.
- Radiation therapy may cause fatigue, urinary issues, and bowel problems.
A comparison of side effect profiles is crucial for patients to understand what to expect from each treatment.
Quality of Life Considerations
Quality of life after treatment is a significant consideration for patients.
Both treatments have their own recovery processes, and understanding these can help patients make informed decisions.
In conclusion, the choice between prostate surgery and radiation therapy depends on various factors, including the patient’s overall health, the stage of cancer, and personal preferences regarding potential side effects and quality of life.
Active Surveillance vs. Surgery: Pros and Cons
When diagnosed with prostate cancer, one of the most critical decisions a patient must make is whether to opt for active surveillance or undergo surgery. This decision hinges on various factors, including the stage and aggressiveness of the cancer, the patient’s overall health, and personal preferences.
Candidates for Active Surveillance
Active surveillance is typically recommended for patients with low-risk prostate cancer. These are individuals with tumors that are small, localized, and not very aggressive. The American Urological Association guidelines suggest that men with very low-risk prostate cancer are ideal candidates for active surveillance.
Candidates for active surveillance usually undergo regular monitoring, which includes:
- Prostate-specific antigen (PSA) tests
- Digital rectal exams (DRE)
- Periodic prostate biopsies
Psychological Aspects of Watchful Waiting
The psychological impact of choosing active surveillance over immediate treatment can be significant. Patients may experience anxiety or fear about the potential progression of their cancer. However, many men report feeling empowered by taking an active role in monitoring their condition.
Support from healthcare providers, family, and support groups can play a crucial role in mitigating these psychological effects. It’s essential for patients to discuss their concerns and understand the rationale behind their treatment plan.
When to Transition from Surveillance to Treatment
The decision to transition from active surveillance to treatment is based on evidence of cancer progression. This can be indicated by changes in PSA levels, findings from DRE, or results from surveillance biopsies showing an increase in cancer grade or volume.
| Indicator | Surveillance | Treatment Threshold |
| PSA Level | Regular monitoring | Rapid increase or high absolute value |
| DRE Findings | Regular exams | Detection of tumor growth or hardening |
| Biopsy Results | Periodic biopsies | Increase in Gleason score or cancer volume |
Understanding the pros and cons of active surveillance versus surgery is crucial for making an informed decision. While active surveillance avoids the immediate risks associated with surgery, it requires ongoing monitoring and the potential for future treatment. Surgery, on the other hand, offers the possibility of removing the cancer entirely but comes with its own set of risks and complications.
Recovery Time and Return to Normal Activities
Prostate surgery recovery time varies among individuals, but knowing what to expect can greatly ease the transition back to daily life. The recovery process involves several stages, from the initial hospital stay to the gradual resumption of normal activities.
Hospital Stay Duration
The length of hospital stay after prostate surgery can differ based on the type of surgical procedure performed and the patient’s overall health. Generally, patients who undergo robotic-assisted laparoscopic prostatectomy tend to have shorter hospital stays compared to those who have open prostatectomy.
On average, the hospital stay can range from 1 to 3 days. During this time, medical staff closely monitor the patient’s condition, manage pain, and watch for any immediate complications.
Milestones in the Recovery Process
Recovery from prostate surgery is marked by several key milestones. Initially, patients focus on managing pain and discomfort at home. Within a few weeks, most men are able to resume light activities.
Significant milestones include:
- Returning to normal daily activities without significant fatigue
- Gradually increasing physical activity, including walking and light exercise
- Regaining urinary control, though this can take several months for some patients
Returning to Work and Exercise
The timeline for returning to work depends on the nature of the job and the individual’s recovery pace. Generally, men with desk jobs may return to work within 2 to 4 weeks, while those with more physically demanding jobs may need 6 to 8 weeks or more.
Exercise is an important aspect of recovery, helping to improve overall health and potentially speeding up the recovery process. Patients are usually advised to start with light activities like walking and gradually progress to more strenuous exercises.
It’s crucial to follow the specific guidance provided by healthcare providers regarding physical activity to avoid complications and ensure a smooth recovery.
Decision-Making Framework for Patients
Making an informed decision about prostate cancer treatment involves understanding the available options, their implications, and how they align with the patient’s personal values and health goals. This decision-making process is critical and can be complex, involving various stakeholders and considerations.
Key Questions to Ask Your Doctor
One of the most crucial steps in the decision-making process is asking the right questions. Patients should inquire about the severity of their prostate cancer, the recommended treatment options, and the potential outcomes of each. Understanding the risks and benefits associated with each treatment pathway is vital.
- What are the stage and grade of my prostate cancer?
- What are the recommended treatment options for my specific condition?
- What are the potential side effects of each treatment option?
- How will the treatment impact my quality of life?
- Are there any clinical trials or new treatments available?
Involving Family in the Decision Process
Involving family members in the decision-making process can provide emotional support and help patients make more informed decisions. Family can offer different perspectives and help in remembering the information discussed during doctor’s visits.
Benefits of family involvement include:
- Emotional support during a challenging time
- Additional perspectives on treatment options
- Assistance in recalling information from doctor’s visits
- Help in evaluating the pros and cons of different treatments
By adopting a comprehensive decision-making framework that includes asking key questions and involving family, patients can navigate the complexities of prostate cancer treatment with greater confidence and clarity.
Conclusion
Deciding whether prostate surgery is worth it depends on various factors, including the severity of prostate cancer, overall health, and personal preferences. Prostatectomy, when considered, offers benefits in terms of cancer control and potentially improved life expectancy after prostate surgery.
While surgery carries risks and complications, advancements in techniques like robotic-assisted laparoscopic prostatectomy have improved outcomes and reduced recovery times. Quality of life post-surgery is a significant consideration, with many men experiencing a return to normal activities within a few months.
Ultimately, the decision to undergo prostate surgery should be made after thorough consultation with healthcare providers, considering individual circumstances and the potential impact on quality of life. By weighing the evidence and understanding the benefits and risks, patients can make informed decisions that align with their needs and priorities.
FAQ
What are the benefits of prostatectomy?
Prostatectomy can provide effective cancer control, improve survival rates, and offer psychological benefits by removing the tumor.
What are the risks of prostate removal surgery?
Risks include short-term surgical complications, long-term health implications, erectile dysfunction, and urinary incontinence.
How does prostate surgery affect quality of life?
Prostate surgery can impact physical recovery, emotional, and psychological adjustment, but many patients experience improved quality of life after recovery.
What is the success rate of prostatectomy?
Success rates vary depending on patient profiles, cancer stage, and surgical expertise, but prostatectomy is generally effective in controlling cancer.
Can prostate cancer recur after surgery?
Yes, prostate cancer can recur after surgery, but the risk varies depending on factors like cancer stage, Gleason score, and surgical margins.
How common is erectile dysfunction after prostate surgery?
Erectile dysfunction is a common side effect of prostate surgery, but the prevalence varies depending on the surgical technique, patient age, and pre-existing conditions.
What are the treatment options for erectile dysfunction after prostate surgery?
Treatment options include medications, vacuum erection devices, and penile implants, and the choice depends on individual patient needs and preferences.
How long does it take to recover from prostate surgery?
Recovery time varies, but most patients can return to normal activities within several weeks to a few months after surgery.
What are the costs associated with prostate cancer surgery?
Costs vary depending on factors like insurance coverage, surgical fees, and hospital charges, but patients can expect significant out-of-pocket expenses.
Is robotic prostatectomy better than traditional open surgery?
Robotic prostatectomy offers advantages like less blood loss, less pain, and faster recovery, but the outcome depends on the surgeon’s expertise and patient selection.
How does prostate surgery compare to radiation therapy?
Both treatments have their efficacy in cancer control, but they differ in side effect profiles and quality of life considerations, and the choice depends on individual patient needs.
What are the pros and cons of active surveillance versus surgery?
Active surveillance is suitable for low-risk patients, but it requires regular monitoring, while surgery offers definitive treatment, but with potential side effects.
What questions should I ask my doctor about prostate surgery?
Patients should ask about the surgeon’s experience, surgical technique, potential complications, and post-operative care to make an informed decision.
How can I manage urinary incontinence after prostate surgery?
Management strategies include pelvic floor exercises, lifestyle modifications, and medical treatments, and patients should discuss their options with their healthcare provider.
Can I return to my normal activities after prostate surgery?
Yes, most patients can return to their normal activities, including work and exercise, within several weeks to a few months after surgery, with some adjustments.
References
- Cancer.org. (2023, January 31). Considering Treatment Options for Early Prostate Cancer. https://www.cancer.org/cancer/types/prostate-cancer/treating/considering-options.html
- Medical News Today. (2025, April 29). 10 natural remedies for enlarged prostate and lifestyle tips. https://www.medicalnewstoday.com/articles/321231