Last Updated on December 2, 2025 by Bilal Hasdemir

Is strep throat the same as tonsillitis? No, Strep is a specific cause of tonsillitis, but not all tonsillitis is Strep. Many people wonder if strep throat and tonsillitis are the same thing. At Liv Hospital, we know how important it is to get the right diagnosis and treatment. Both can cause sore throats and swollen tonsils, but they have different causes and need different treatments.
Strep throat is caused by a specific bacteria, group A Streptococcus. On the other hand, tonsillitis is when the tonsils get inflamed, often from viruses or bacteria. We’ll explain the main differences between these two throat infections. This will help you understand their unique features and how to treat them.
Key Takeaways
- Strep throat is a bacterial infection caused by group A Streptococcus.
- Tonsillitis is inflammation of the tonsils due to various infections.
- The causes and symptoms of strep throat and tonsillitis differ.
- Accurate diagnosis is key for effective treatment.
- Liv Hospital offers patient-centered care for throat infections.
Understanding Throat Infections: The Basics

It’s important to know the basics of throat infections to get the right treatment. Conditions like strep throat and tonsillitis are common and can really affect your life. We’ll look at what causes sore throats, the anatomy of the throat and tonsils, and why getting a correct diagnosis is so important.
Common Causes of Sore Throats
Sore throats can come from many things, like viruses and bacteria. Viruses are the main cause, with the common cold and influenza being big offenders. But, bacterial infections, like those from group A Streptococcus, can also cause sore throats, as seen in strep throat.
Tonsils play a big role in throat infections. Tonsillitis, or inflammation of the tonsils, can be caused by viruses or bacteria. Knowing if it’s viral or bacterial is key to picking the right treatment.
Anatomy of the Throat and Tonsils
The throat, or pharynx, is a muscular tube that connects the digestive and respiratory systems. The tonsils are lymphoid organs on either side of the back of the throat. They help filter out pathogens that enter through the mouth or nose.
The anatomy of the throat and tonsils is complex. The tonsils are positioned to meet pathogens early. This makes them more likely to get infected and inflamed, leading to conditions like tonsillitis.
Why Accurate Diagnosis Matters
Getting the right diagnosis for throat infections is vital for proper treatment. Misdiagnosis or delayed diagnosis can lead to serious problems, like the spread of infection or severe conditions like rheumatic fever if strep throat is left untreated.
We use physical exams, medical history, and tests like rapid strep tests and throat cultures to diagnose throat infections accurately. Knowing if it’s a viral or bacterial cause is essential for choosing the right treatment.
What Exactly Is Strep Throat?

“Strep throat” is a bacterial infection that hits the throat and tonsils. It’s caused by Group A Streptococcus bacteria. This germ is super contagious and spreads through coughs, sneezes, or skin sores.
Definition and Causative Bacteria
Strep throat is an infection of the throat and tonsils by Group A Streptococcus (GAS) bacteria. This bacterium causes many infections, from mild to severe. Symptoms start suddenly with a very sore throat, fever, and swollen lymph nodes.
Key characteristics of strep throat include:
- Severe sore throat
- High fever
- Swollen lymph nodes
- White patches on the tonsils
- Headache and stomachache
Prevalence in Adults vs. Children
Strep throat hits kids more than adults, mainly between 5 to 15 years old. Kids get it more because their immune systems are growing and they’re in school. Adults can get it too, mostly if they’re around kids with it.
Age Group | Prevalence of Strep Throat |
Children (5-15 years) | Higher prevalence due to increased exposure and developing immune systems |
Adults | Lower prevalence, but can be infected through exposure to children or other infected individuals |
How Group A Streptococcus Spreads
Group A Streptococcus bacteria spread through:
- Direct contact with respiratory secretions (e.g., mucus, saliva)
- Infected skin sores
- Contaminated surfaces or objects
Good hygiene is key. Wash hands often and avoid touching sick people to stop the spread.
“Prevention is key in managing strep throat. By understanding how the infection spreads, we can take necessary precautions to protect ourselves and our loved ones.”
Knowing about strep throat helps us manage and prevent it. It’s all about understanding the cause, how it spreads, and who gets it.
Tonsillitis Explained: Beyond Strep Throat
“Tonsillitis” means the tonsils are inflamed. This can happen for many reasons, like viruses or bacteria. It’s often linked to strep throat, but it can also be caused by other things.
What Happens When Tonsils Become Inflamed
When tonsils get inflamed, they swell up, turn red, and hurt. It’s hard to swallow. You might also feel fever, headache, and feel really tired.
Viral vs. Bacterial Causes
Tonsillitis can come from viruses or bacteria. Viral tonsillitis is more common and can be from the common cold or flu. Bacterial tonsillitis is usually from Group A Streptococcus, the same bacteria as strep throat.
It’s not always easy to tell if it’s viral or bacterial. But bacterial tonsillitis is usually worse and might need antibiotics.
Acute vs. Chronic Tonsillitis
Tonsillitis can be either acute or chronic. Acute tonsillitis is short-term and can get better with treatment. Chronic tonsillitis keeps coming back and can cause serious problems if not treated right.
Comparison of Acute and Chronic Tonsillitis
Characteristics | Acute Tonsillitis | Chronic Tonsillitis |
Duration | Short-term, typically resolving within a few days to a week | Long-term, recurring, or persistent |
Symptoms | Severe sore throat, fever, swollen tonsils | Mild to moderate sore throat, bad breath, persistent tonsillar inflammation |
Treatment | Supportive care, antibiotics if bacterial | Long-term management, possible tonsillectomy |
Knowing the difference between acute and chronic tonsillitis is key. Acute tonsillitis might just need some temporary help. But chronic tonsillitis might need more serious treatment, like surgery.
Is Strep Throat the Same as Tonsillitis? The Critical Relationship
Strep throat can cause tonsillitis, but not all tonsillitis comes from strep throat. This shows why getting a correct diagnosis is so important. Let’s dive into this important connection.
How Strep Can Cause Tonsillitis
Strep throat, caused by Group A Streptococcus bacteria, can infect the tonsils. This leads to tonsillitis, with symptoms like swollen, red tonsils and fever. It also causes a sore throat.
Key factors that contribute to the development of tonsillitis from strep throat include:
- The virulence of the Group A Streptococcus bacteria
- The individual’s immune response to the infection
- Previous history of tonsillitis or strep throat
Why All Tonsillitis Is Not Strep Throat
Tonsillitis can be caused by many things, not just strep throat. Viruses like adenovirus, influenza, and mononucleosis can also cause it. Other bacteria, like Staphylococcus aureus, can lead to tonsillitis too. This means not all tonsillitis is caused by strep throat, making accurate testing key.
“Accurate diagnosis is critical in telling strep throat apart from other tonsillitis causes. It ensures the right treatment and prevents complications.”
Statistical Breakdown of Causes
Research shows strep throat causes 15% to 30% of tonsillitis in kids. In adults, it’s less common. The rest is due to viruses or other bacteria. Here’s a table showing the common causes and their prevalence:
Cause | Estimated Prevalence |
Viral infections | 50% – 70% |
Group A Streptococcus (Strep throat) | 15% – 30% |
Other bacterial infections | 5% – 15% |
Knowing the causes and their frequencies helps doctors choose the right tests and treatments.
Comparing Symptoms: How to Tell the Difference
Strep throat and tonsillitis can both cause sore throats. But they have different symptoms and signs. Knowing these differences is important for treating these conditions right.
Classic Signs of Strep Throat
Strep throat is caused by Group A Streptococcus bacteria. It has sudden and severe symptoms. Classic signs include a sore throat, fever, and swollen lymph nodes. Patients may also have headache, stomach pain, and nausea.
Medical experts say, “The sudden onset of severe sore throat is a hallmark of strep throat, distinguishing it from other throat infections.”
Typical Tonsillitis Symptoms
Tonsillitis can be caused by viruses or bacteria. Its symptoms include swollen tonsils, sore throat, and fever. Tonsillitis symptoms may take a few days to get worse. Other signs are white or yellow patches on the tonsils, bad breath, and trouble swallowing.
Overlapping Symptoms That Cause Confusion
Strep throat and tonsillitis share symptoms like sore throat, fever, and swollen lymph nodes. This makes it hard to tell them apart. But, there are unique signs for each condition.
Unique Indicators for Each Condition
Strep throat is known for severe throat pain and no cough. Tonsillitis shows visible swelling and redness of the tonsils. Strep throat starts suddenly, while tonsillitis symptoms come on more slowly. Knowing these signs is key for a correct diagnosis.
In conclusion, while both conditions share some symptoms, looking closely at their unique signs helps doctors diagnose and treat them right.
Diagnostic Approaches for Both Conditions
Diagnosing strep throat and tonsillitis involves several steps. We look at physical exams, lab tests, and sometimes imaging. This helps doctors tell these two conditions apart.
Physical Examination Techniques
A thorough physical exam is the first step. We check the throat for signs of inflammation. This includes redness, swelling, and white patches on the tonsils.
We also check for fever, swollen lymph nodes, and other symptoms. These signs help us decide if the infection is bacterial or viral.
Rapid Strep Tests and Their Accuracy
Rapid strep tests are used to find strep throat caused by Group A Streptococcus. They give quick results, usually in minutes. This helps doctors make treatment decisions fast.
Even though these tests are very specific, they’re not always 100% accurate. If the test is negative but symptoms suggest strep, a throat culture might be needed.
Throat Cultures and Laboratory Testing
Throat cultures are the best way to diagnose strep throat. A swab of the throat is sent to the lab to check for Group A Streptococcus. These tests also help find other causes of tonsillitis, like other bacteria or viruses.
The results help doctors choose the right antibiotic or treatment.
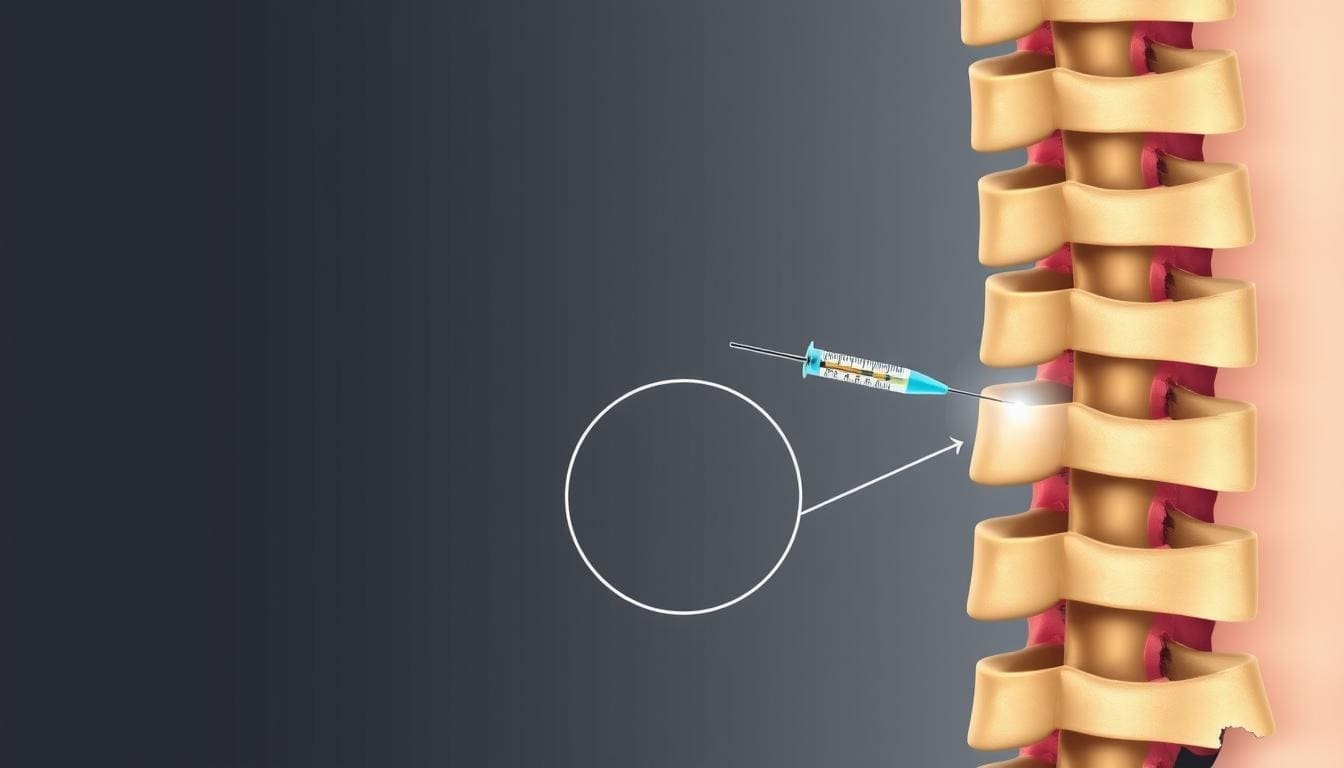
When Imaging May Be Necessary
In some cases, imaging is needed to check for complications of tonsillitis. This includes peritonsillar abscesses or to see how big the tonsils are. Ultrasound or CT scans can give important information for treatment plans.
By using these diagnostic methods, we can accurately diagnose strep throat and tonsillitis. This helps us develop the right treatment plan for each infection.
Treatment Strategies: Different Approaches for Different Causes
Understanding the cause of strep throat and tonsillitis is key to effective treatment. The treatment method changes based on whether it’s a bacterial or viral infection.
Antibiotic Therapy for Strep Throat
Strep throat is caused by Group A Streptococcus bacteria. Antibiotics are needed to shorten symptoms and prevent complications. The right antibiotic depends on the patient’s allergies and local resistance patterns. Penicillin and amoxicillin are common choices.
Antibiotic | Dosage | Duration |
Penicillin | 250 mg, 2-3 times a day | 10 days |
Amoxicillin | 500 mg, once or twice a day | 10 days |
Managing Viral Tonsillitis
Viral tonsillitis doesn’t need antibiotics. Instead, focus on rest, hydration, and pain relief. Over-the-counter pain meds can help. Antiviral meds might be used for certain viruses.
“The management of viral tonsillitis is largely supportive, focusing on relieving symptoms and supporting the body’s immune response.”
Pain Relief and Supportive Care
Pain relief is key for both strep throat and tonsillitis. Use over-the-counter pain relievers like acetaminophen or ibuprofen. Gargling with salt water and staying hydrated also helps. Rest is important for recovery.
When Tonsillectomy Might Be Recommended
For recurrent tonsillitis or complications, tonsillectomy might be an option. This is usually after other treatments fail and quality of life is affected. It can reduce tonsillitis episodes and symptoms.
Knowing the cause and choosing the right treatment helps healthcare providers manage these conditions better. This improves patient outcomes.
Potential Complications of Untreated Infections
Strep throat and tonsillitis can cause serious health problems if not treated. These common conditions need quick medical care to avoid long-term issues.
Serious Consequences of Untreated Strep Throat
Untreated strep throat can lead to serious issues. One major risk is rheumatic fever, which can harm the heart.
Rheumatic Fever and Heart Damage
Rheumatic fever is a serious disease that can happen after strep throat. It can damage heart valves, causing long-term health problems. The Centers for Disease Control and Prevention (CDC) says it’s a big worry in places with limited healthcare access.
Complication | Description | Potential Long-term Effects |
Rheumatic Fever | Inflammatory disease following strep throat | Heart valve damage, heart failure |
Scarlet Fever | Rash and fever associated with strep throat | Skin complications, kidney disease |
Scarlet Fever Development
Scarlet fever is another risk of untreated strep throat. It’s marked by a bright red rash and can cause kidney disease if not treated.
Complications Specific to Chronic Tonsillitis
Chronic tonsillitis can cause sleep disorders and trouble swallowing if not treated. In severe cases, a tonsillectomy might be needed to fix symptoms.
It’s important to get medical help for strep throat and tonsillitis quickly. Knowing the risks of untreated infections helps people get the care they need to avoid serious health problems.
Prevention Strategies for Both Conditions
Strep throat and tonsillitis can be prevented with simple hygiene practices and awareness of our environment. Understanding the causes and taking preventive steps can lower our risk of getting these illnesses.
Hygiene Practices to Reduce Transmission
Good hygiene is key to fighting strep throat and tonsillitis. Frequent handwashing with soap and water is essential. This is important after coughing or sneezing, and before eating. Also, avoid close contact with those who are sick, as infections can spread through the air.
- Wash hands frequently with soap and water.
- Avoid sharing utensils or personal items.
- Cover the mouth and nose when coughing or sneezing.
Environmental Factors and Risk Reduction
Our environment also affects the spread of strep throat and tonsillitis. Being mindful of our surroundings and taking steps to reduce exposure to infections is important.
- Avoid crowded areas during outbreaks.
- Ensure good ventilation in living and working spaces.
- Regularly clean and disinfect surfaces and objects that are frequently touched.
Building Immunity Through Lifestyle Choices
A healthy lifestyle can boost our immunity against infections like strep throat and tonsillitis. This includes eating a balanced diet, exercising regularly, and getting enough sleep.
Key Lifestyle Choices:
- Eat a balanced diet.
- Exercise regularly.
- Get enough sleep.
By making these prevention strategies a part of our daily lives, we can lower our risk of getting strep throat and tonsillitis.
When to Seek Medical Attention
Knowing when to get medical help is key for managing strep throat with tonsillitis. It helps avoid serious complications.
Red Flags That Warrant Immediate Care
Some symptoms mean you need to see a doctor right away. If you or your child has trouble breathing, severe throat pain, or a fever over 101.5°F, get help fast. These signs can mean a serious infection that needs quick treatment.
- Difficulty breathing or swallowing
- High fever above 101.5°F (38.6°C)
- Severe throat pain
- Swollen tonsils that are touching or nearly touching
Symptoms That Shouldn’t Be Ignored
Other symptoms also need medical attention. These include a sore throat that won’t go away, white patches on the tonsils, and swollen neck lymph nodes. Seeing a doctor is important to find out what’s wrong and how to treat it.
Follow-up Care After Treatment
After treating tonsillitis strep throat, you need to follow up. Your doctor might want to see you again to check if the infection is gone. If symptoms keep coming back, you might need more tests to find out why.
By knowing when to get medical help and following up, you can handle strep throat and tonsillitis well. If you’re not sure about your symptoms or what to do, always talk to a doctor.
Conclusion
In this article, we’ve looked into strep throat and tonsillitis. These two conditions are often mixed up. So, is strep throat the same as tonsillitis? The answer is no, they are different.
Strep throat is caused by a bacterial infection. Tonsillitis, on the other hand, can be from viruses or bacteria. Knowing the cause is key to treating it right.
Both conditions can make your throat hurt, but they need different treatments. It’s important to get a proper diagnosis. This helps figure out if you have strep or tonsillitis.
It’s hard to tell strep throat from tonsillitis just by symptoms. That’s why seeing a doctor is important. They can tell you what you really have.
In short, knowing the difference between strep throat and tonsillitis is important. It helps you get the right treatment. This way, you can avoid any serious problems.
FAQ
What is the difference between strep throat and tonsillitis?
Strep throat is a bacterial infection caused by Group A Streptococcus. Tonsillitis is inflammation of the tonsils, which can be caused by viruses or bacteria, including strep throat.
Can strep throat cause tonsillitis?
Yes, strep throat can cause tonsillitis. The bacteria can infect the tonsils, leading to inflammation.
Are swollen tonsils always a sign of strep throat?
No, swollen tonsils can be a symptom of various conditions. It’s not exclusive to strep throat.
How can I tell if I have strep throat or tonsillitis?
Both conditions share similar symptoms. Strep throat typically presents with severe throat pain, fever, and swollen lymph nodes. Tonsillitis may have additional symptoms like white or yellow patches on the tonsils.
Is tonsillitis the same as strep throat?
No, tonsillitis is a broader term. It encompasses inflammation of the tonsils from various causes. Strep throat is a specific bacterial infection.
Can tonsillitis lead to strep throat?
Tonsillitis itself is not a cause of strep throat. But if tonsillitis is caused by a bacterial infection like Group A Streptococcus, then it is strep throat.
What are the symptoms of strep throat with tonsillitis?
Symptoms include severe throat pain, swollen tonsils, fever, headache, and swollen lymph nodes in the neck.
How is strep throat diagnosed?
Diagnosis is made through a rapid strep test or throat culture. These tests detect the presence of Group A Streptococcus.
How is tonsillitis treated?
Treatment depends on the cause. Viral tonsillitis is managed symptomatically. Bacterial tonsillitis, including cases caused by strep throat, may require antibiotic therapy.
Can I prevent strep throat and tonsillitis?
Yes, practicing good hygiene helps. Frequent handwashing and avoiding close contact with infected individuals can reduce the risk of both conditions.
When should I seek medical attention for sore throat?
Seek medical attention for severe throat pain, difficulty swallowing, high fever, or if symptoms persist or worsen over time.
What is the difference between viral and bacterial tonsillitis?
Viral tonsillitis is caused by viruses. Bacterial tonsillitis is caused by bacteria, with strep throat being a common cause of the latter.
Can lifestyle choices help prevent strep throat and tonsillitis?
Yes, a healthy lifestyle can help. A balanced diet and regular exercise support immune function and may reduce the risk of these infections.
References
- Plager, D. A. (2017). Anesthesia for tonsillectomy: Current perspectives. Local and Regional Anesthesia, 10, 9-18. Link