
Ischemic Heart Disease (IHD) is a serious condition. It happens when blood flow to the heart is cut down. This is because the arteries are narrowed. It’s a major cause of death worldwide.
At Liv Hospital, we know how important it is to treat IHD well. We focus on preventing problems and saving lives. Our care is patient-centered and follows the latest medical standards.
It’s key to know the 7 main ways to manage IHD. Both doctors and patients need to understand these methods. We’ll look at them and why checking for risks is so important.
Key Takeaways
- Understanding IHD and its symptoms is key for managing it well.
- Treating IHD involves changing your lifestyle and using medical treatments.
- Checking for risks is very important to avoid serious problems.
- Liv Hospital is dedicated to giving top-notch care for IHD patients.
- Keeping up with new medical practices is vital for treating IHD.
What Is Ischemic Heart Disease?
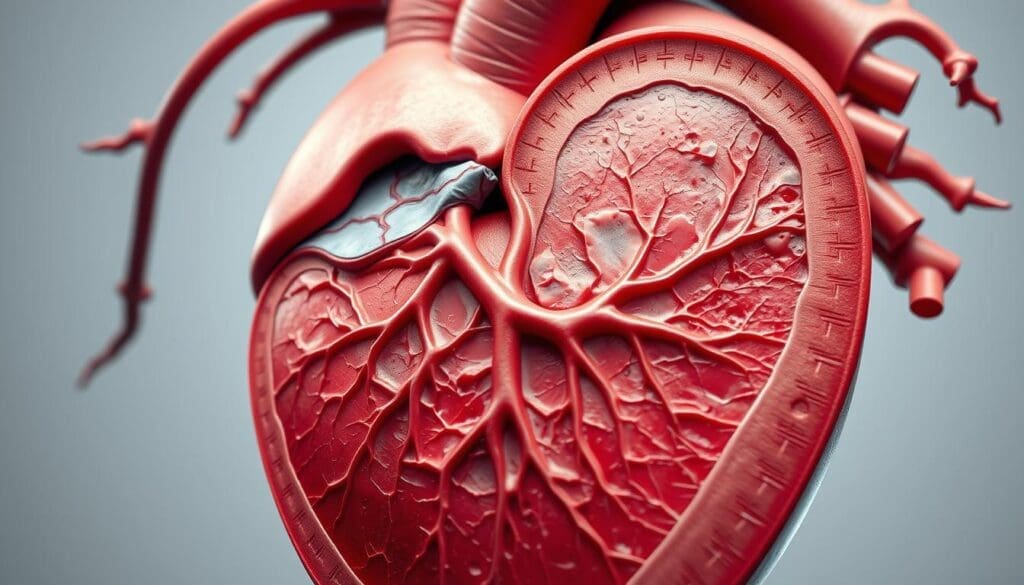
Understanding Ischemic Heart Disease is key to grasping its link to Coronary Artery Disease. It’s a condition where the heart muscle doesn’t get enough oxygen-rich blood. This usually happens because blood flow is reduced.
This reduction can cause symptoms and problems, making it a big deal for heart health.
Medical Definition and Terminology
Ischemic Heart Disease is when the heart muscle doesn’t get enough oxygen. This is often because of atherosclerosis. Atherosclerosis is when plaque builds up in the coronary arteries, narrowing them and cutting off blood flow to the heart.
Knowing the medical terms for IHD is important for diagnosing and treating it.
The word “ischemic” means there’s less blood flow to the heart muscle. “Heart disease” is a broader term that includes many conditions affecting the heart. So, IHD is a specific heart disease related to blood supply issues.
IHD vs. Coronary Artery Disease
Ischemic Heart Disease and Coronary Artery Disease (CAD) are connected but not the same. CAD is when the coronary arteries are narrowed or blocked by atherosclerosis. IHD is what happens when this narrowing or blockage reduces blood flow to the heart muscle.
Often, CAD causes IHD. But IHD can also come from other things that cut down blood flow or make the heart need more oxygen. Knowing the difference between these two is important for correct diagnosis and treatment.
Common Signs and Symptoms of IHD
Knowing the signs and symptoms of Ischemic Heart Disease (IHD) is key to managing it well. IHD can show itself in many ways, both typical and not so common.
Classic Symptoms: Chest Pain and Shortness of Breath
The most common signs of IHD are chest pain, or angina, and shortness of breath. Angina feels like pressure or tightness in the chest. It can spread to the arms, back, neck, jaw, or stomach. It usually happens when you’re active or stressed and goes away with rest or medicine.
Shortness of breath, or dyspnea, happens when the heart can’t pump well. This leads to fluid in the lungs. It can happen even when you’re not moving and gets worse if not treated.
Atypical Presentations and Silent Ischemia
Not everyone shows the usual signs of IHD. Some might feel tired, nauseous, or have discomfort in the upper belly. These can be mistaken for other issues. Others might have silent ischemia, where the heart doesn’t get enough blood but they don’t feel any symptoms.
Atypical symptoms are more common in some groups, like women, older people, and those with diabetes. Spotting these different signs is important for quick diagnosis and treatment.
| Symptom Type | Description | Common Triggers |
|---|---|---|
| Classic Symptoms | Chest pain (angina), shortness of breath | Physical exertion, stress |
| Atypical Presentations | Fatigue, nausea, upper abdominal discomfort | Varies, often less predictable |
| Silent Ischemia | No noticeable symptoms | Often asymptomatic, may be detected during testing |
We stress the need to know about these different symptoms. This way, you can get help fast. Early treatment can greatly improve life for those with IHD.
Comprehensive Risk Assessment for Ischemic Heart Disease
Assessing the risk of ischemic heart disease involves looking at both traditional and lifestyle factors. We examine these to figure out a person’s risk of getting IHD. Then, we tailor strategies to manage it.
Traditional Risk Factors
Traditional risk factors for IHD include hypertension, diabetes mellitus, and dyslipidemia. These conditions raise the risk of coronary artery disease and ischemic heart disease. For example, high blood pressure can narrow and harden arteries.
Diabetes mellitus also increases the risk of IHD. It makes managing the disease harder because of nerve damage and silent ischemia.
Lifestyle-Related Risks
Lifestyle risks like smoking, obesity, and chronic stress are also key in IHD development. Smoking damages blood vessel linings, making them more likely to block. Obesity is linked to other risks like high blood pressure and diabetes.
Chronic stress indirectly contributes to IHD. It can lead to unhealthy behaviors and affect blood pressure and inflammation.
A study in BMC Endocrine Disorders shows managing these risks is vital for preventing IHD.
| Risk Factor | Description | Impact on IHD |
|---|---|---|
| Hypertension | High blood pressure | Increases risk of artery narrowing and hardening |
| Diabetes Mellitus | High blood sugar levels | Associated with atherosclerosis and neuropathy |
| Dyslipidemia | Abnormal levels of lipids in the blood | Contributes to plaque formation in arteries |
| Smoking | Use of tobacco products | Damages blood vessel lining, increases blockage risk |
| Obesity | Excess body fat | Linked with hypertension, diabetes, and other risk factors |
| Chronic Stress | Ongoing mental or emotional strain | Promotes unhealthy behaviors, affects blood pressure and inflammation |
Diagnostic Evaluation Methods for IHD
We use a detailed plan to check patients with suspected ischemic heart disease. This method helps us find and treat IHD well, which improves patient results.
Non-Invasive Testing
First, we use non-invasive tests to start diagnosing IHD. These include:
- Electrocardiogram (ECG): This test is key. It shows the heart’s electrical activity. It helps spot signs of ischemia or past heart attacks.
- Stress Testing: This test checks the heart’s work under stress. It can show ischemia signs that don’t show up when the heart is at rest.
- Imaging Studies: Echocardiography, nuclear stress testing, and cardiac MRI give detailed heart images. They help diagnose IHD.
Invasive Procedures
If non-invasive tests show a big chance of coronary artery disease, we might need to do more.
- Coronary Angiography: This is the top test for coronary artery disease. It uses dye in the arteries to see blockages or problems on an X-ray.
By mixing the results from these tests, we get a full picture of a patient’s IHD. Then, we can make a good treatment plan.
Ischemic Heart Disease Treatment: Overview of 7 Essential Methods
Managing ischemic heart disease needs a treatment plan made just for each patient. Every patient is different, so their treatment must match their unique needs and risks.
Treatment Goals and Approach Selection
The main treatment goals are to lessen symptoms, slow disease growth, and boost quality of life. We look at many factors, like symptom severity, disease extent, and other health issues.
We choose treatments based on their benefits and risks. We follow the latest guidelines and research. Our goal is to find the best treatment with the least harm.
Acute vs. Chronic Treatment Strategies
Ischemic heart disease treatment falls into two main types: acute and chronic. Acute treatment deals with immediate needs, like easing symptoms during an angina attack. On the other hand, chronic treatment focuses on long-term care, like lifestyle changes and ongoing monitoring.
We stress the need for a complete treatment plan that covers both immediate and ongoing needs. This approach helps improve patient outcomes, lowers complication risks, and boosts quality of life.
The 7 key methods for treating ischemic heart disease will be explored in the following sections. These include lifestyle changes, medication, procedures, cardiac rehab, enhanced external counterpulsation, stem cell and gene therapy, and managing chronic disease.
Method 1: Lifestyle Modifications and Risk Factor Control
Lifestyle changes are key in managing Ischemic Heart Disease (IHD). They help lower the risk of serious problems. We suggest a wide range of lifestyle changes to boost heart health.
Heart-Healthy Diet and Weight Management
Eating a heart-healthy diet is essential for IHD management. Focus on fruits, veggies, whole grains, and lean proteins. Cut down on saturated fats, trans fats, and cholesterol.
Keeping a healthy weight is also vital. Too much weight puts extra strain on the heart and raises risk. To lose weight, mix diet changes with regular exercise. Try to lose 1-2 pounds a week for better results.
Exercise Programs and Smoking Cessation
Exercise is a big part of managing IHD. We help create an exercise program that fits your health and fitness level. Include activities like walking, cycling, or swimming, and resistance training for better heart health.
Quitting smoking is also critical for IHD patients. Smoking greatly increases heart disease risk. We provide support and resources to help you stop smoking, like counseling and medication.
By making these lifestyle changes, IHD patients can greatly improve their life quality. They can also lower the chance of future heart problems.
Method 2: Pharmacological Therapy for IHD
Pharmacological treatments are key in managing Ischemic Heart Disease. They help reduce symptoms and lower the risk of complications. We use different medications to tackle various aspects of IHD, aiming to enhance patient outcomes and quality of life.
Anti-Anginal Medications
Anti-anginal drugs are vital for treating angina pectoris, a common symptom of IHD. These drugs either lower the heart’s oxygen need or boost oxygen supply. The main types include:
- Nitrates: Nitroglycerin is a key drug for acute angina. It widens blood vessels, cutting down on oxygen demand.
- Beta-blockers: These drugs slow the heart rate and reduce its strength. This lowers oxygen demand and can improve survival rates.
- Calcium Channel Blockers: These drugs stop calcium from entering heart and blood vessel muscles. This action reduces muscle contraction and lowers oxygen demand.
Antiplatelet and Anticoagulant Therapy
Antiplatelet and anticoagulant treatments are essential to prevent blood clots in IHD patients. Aspirin is a mainstay antiplatelet drug, often paired with P2Y12 inhibitors (like clopidogrel) for stent patients. Anticoagulants, such as warfarin or direct oral anticoagulants (DOACs), are used in specific cases, like atrial fibrillation or post-myocardial infarction with left ventricular thrombus.
| Medication Class | Examples | Primary Mechanism |
|---|---|---|
| Antiplatelet Agents | Aspirin, Clopidogrel | Inhibit platelet aggregation |
| Anticoagulants | Warfarin, DOACs | Inhibit thrombin or factor Xa |
Lipid-Lowering and Blood Pressure Medications
Controlling high cholesterol and blood pressure is vital for IHD management. Statins are the main drugs for lowering LDL cholesterol and reducing heart events. For those with hard-to-treat high cholesterol, PCSK9 inhibitors might be used. To control blood pressure, we often prescribe ACE inhibitors or ARBs, which have been proven to lower heart risks.
By combining these treatments, we can manage IHD effectively, reduce symptoms, and improve patient outcomes. The right medication and treatment plan depend on the patient’s risk and condition.
Method 3: Revascularization Procedures
Revascularization techniques like PCI and CABG have changed how we treat heart disease. They help patients with serious heart artery problems. These methods aim to get blood flowing to the heart again, easing symptoms and improving health.
Percutaneous Coronary Intervention (PCI)
Percutaneous Coronary Intervention (PCI) is a non-surgical way to open blocked heart arteries. PCI is great for patients with sudden heart attacks or severe symptoms that don’t get better with medicine.
- Indications: PCI is for those with heart attacks, unstable angina, or stable angina that doesn’t improve with medicine.
- Benefits: It can lessen symptoms, enhance life quality, and might lower the chance of future heart problems.
- Risks: Though safe, PCI can lead to bleeding, vascular issues, and the chance of artery narrowing again.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a surgery that bypasses blocked heart arteries with grafts. CABG is suggested for those with complex heart disease or who didn’t get better with PCI.
- Indications: CABG is for complex heart disease, like left main coronary artery disease or diabetes.
- Benefits: It can offer long-term symptom relief, improve survival in some, and cut down on future surgeries.
- Risks: Like any big surgery, CABG has risks like infection, bleeding, and stroke.
PCI and CABG are key in treating heart disease. The choice between them depends on the heart disease’s extent, patient health, and personal choices.
Methods 4-7: Advanced Treatment Approaches
Ischemic Heart Disease treatment has grown to include new methods. These advanced treatments aim to better patient outcomes and quality of life.
Method 4: Cardiac Rehabilitation Programs
Cardiac rehab is key in managing IHD. It includes supervised exercise training, heart-healthy living education, and stress management techniques. These help patients recover and improve heart health.
Patients in cardiac rehab see big improvements. They feel better, have more energy, and enjoy a better life.
Method 5: Enhanced External Counterpulsation (EECP)
EECP is a non-invasive method. It uses external counterpulsation to boost heart blood flow. Cuffs on the legs inflate and deflate with the heartbeat.
EECP cuts down on angina, boosts exercise ability, and improves life quality for those with hard-to-treat angina.
Method 6: Stem Cell and Gene Therapy
Stem cell and gene therapy are new research areas for IHD. They aim to regenerate damaged heart tissue and enhance heart function.
Early studies show promise. They suggest better heart function and symptom relief.
Method 7: Management of Chronic Ischemic Heart Disease
Chronic IHD management is complex. It includes ongoing monitoring, lifestyle changes, and optimized medical therapy. This long-term plan is vital for stopping disease growth and managing symptoms.
With a detailed treatment plan, patients with chronic IHD can see better results and enjoy a higher quality of life.
Living with Chronic Ischemic Heart Disease
Managing chronic ischemic heart disease is key to avoiding serious problems and improving life quality. We know it’s tough, but the right steps can help patients live well.
Long-term Management Strategies
Handling chronic ischemic heart disease needs a team effort. This includes medication adherence, lifestyle changes, and regular doctor visits. Patients should team up with their doctors to create a plan that fits them.
Important parts of long-term care are:
- Following the doctor’s medication advice
- Making healthy lifestyle choices
- Going for regular check-ups
- Staying updated on their health
Preventing Complications and Recurrence
Stopping complications is a big part of managing chronic ischemic heart disease. It’s important to control risks like high blood pressure, diabetes, and high cholesterol. Eating right and staying active can help manage these risks.
| Risk Factor | Management Strategy |
|---|---|
| Hypertension | Keep an eye on blood pressure, take meds as directed, and eat less sodium. |
| Diabetes | Control blood sugar with diet, exercise, and meds as needed. |
| High Cholesterol | Eat healthy, exercise often, and take meds for cholesterol if told to. |
By tackling these risks, patients can lower their chance of serious problems and boost their health.
We stress the need for teamwork between patients and doctors in managing chronic ischemic heart disease. Together, patients get the care they need to do well.
Conclusion: Integrated Approach to IHD Management
Managing ischemic heart disease well needs a complete plan. This includes lifestyle changes, medicines, and specific treatments for each patient. We’ve talked about different ways to treat it, from making lifestyle changes and taking medicine to using advanced treatments.
Using a complete plan for IHD helps doctors make treatment plans that fit each patient. This way, we can help patients live better and longer. It also lowers the chance of serious problems and helps patients survive longer.
As healthcare workers, we play a big role in helping patients with IHD. We guide them through their treatment and make sure they get the best care. By using a complete plan for IHD, we can really help our patients.
What is ischemic heart disease (IHD)?
Ischemic heart disease, also known as coronary artery disease, happens when the heart muscle doesn’t get enough oxygen. This is because the coronary arteries are narrowed or blocked.
What are the common signs and symptoms of IHD?
Symptoms include chest pain (angina), shortness of breath, and fatigue. Some people might not feel any symptoms or feel them very mildly.
How is IHD diagnosed?
Doctors use a few methods to diagnose IHD. They look at your medical history, do a physical exam, and use tests like an electrocardiogram (ECG). They might also do stress tests and imaging tests.
What are the traditional risk factors for IHD?
Risk factors include high blood pressure, diabetes, and abnormal lipid profiles. Family history of heart disease also plays a role.
How can lifestyle modifications help manage IHD?
Making healthy lifestyle changes can help manage IHD. This includes eating well, exercising, keeping a healthy weight, and quitting smoking.
What pharmacological therapies are used to treat IHD?
Doctors use several medications to treat IHD. These include drugs for chest pain, preventing blood clots, lowering cholesterol, and controlling blood pressure.
What are revascularization procedures, and when are they used?
Revascularization procedures, like PCI and CABG, help restore blood flow to the heart. They are used for severe coronary artery disease or when medical therapy doesn’t work.
What is cardiac rehabilitation, and how does it help?
Cardiac rehabilitation is a program that includes exercise, education, and support. It helps patients recover from heart conditions like IHD and improves their heart health.
Can IHD be managed long-term?
Yes, IHD can be managed long-term with the right treatment and lifestyle changes. Regular monitoring and adjusting treatment plans are key to preventing complications.
What is the role of enhanced external counterpulsation (EECP) in treating IHD?
EECP is a non-invasive procedure that improves blood flow to the heart. It’s used to treat angina and other symptoms of IHD.
Are there any advanced treatment approaches for IHD?
Yes, treatments like stem cell and gene therapy are being researched. They aim to repair and regenerate the heart.
How can I assess my risk of developing IHD?
To assess your risk, look at traditional risk factors, lifestyle habits, and family history. Talking to a healthcare provider can help determine your risk and create a plan to lower it.
Reference:
- “2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease” — American Heart Association / Circulation. (AHA Journals)
- “Chronic Ischemic Heart Disease: Selection of Treatment Modality” — NCBI Bookshelf. (NCBI)
- “ESC Guidelines for the management of chronic coronary syndromes” — European Society of Cardiology (ESC). (European Society of Cardiology)
- “Treatment of Stable Ischemic Heart Disease: Recommendations” — American Academy of Family Physicians (AAFP). (American Academy of Family Physicians)
- “Diagnosis of Stable Ischemic Heart Disease” — AAFP. (American Academy of Family Physicians)
“Ischemic Heart Disease – Cardiovascular Disability” — NCBI Bookshelf. (NCBI)









