Last Updated on November 13, 2025 by
Immune thrombocytopenia, or ITP disease, is an autoimmune disorder. It happens when the body’s immune system attacks platelets. This leads to low platelet counts and a higher risk of bleeding. What causes ITP in children (Immune Thrombocytopenia)? Learn the causes and the amazing prognosis. Powerful facts to reassure parents about this condition.
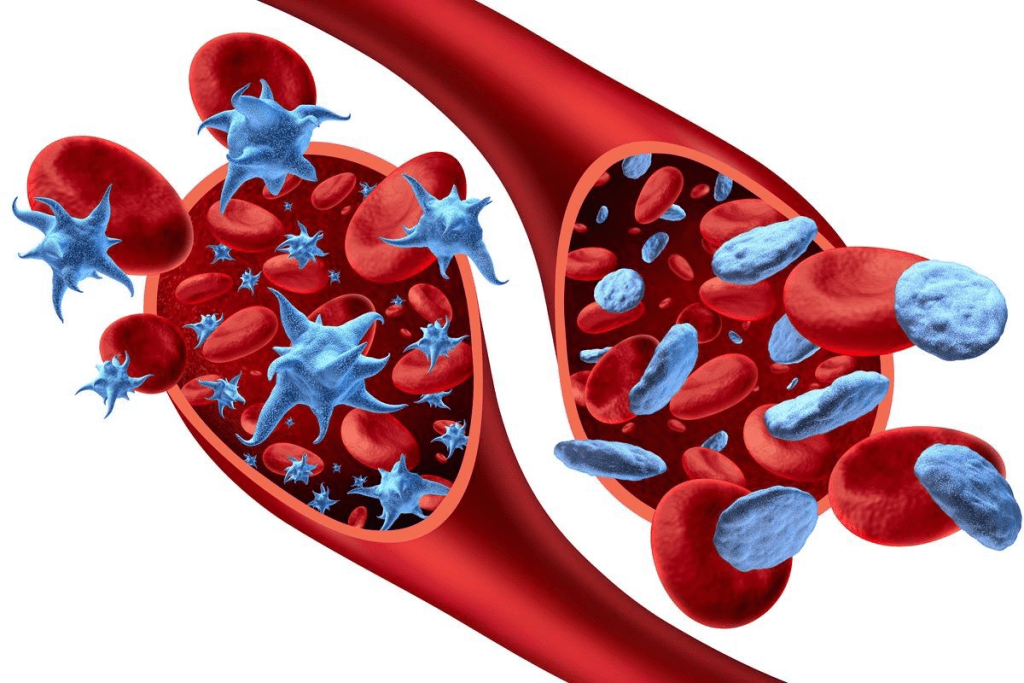
Platelets are key in stopping bleeding. When their count goes down, it can cause easy bruising, bleeding gums, and internal bleeding. Knowing what causes ITP is important for helping children with this condition.
We at our institution are dedicated to top-notch healthcare. We offer full support for international patients. Understanding what is itp helps us give the best care to children with this condition.
It’s key to understand immune thrombocytopenic purpura to help kids with this condition. This disorder, known as ITP, causes low platelet counts. This can lead to bruising and bleeding.

ITP comes in two main types: acute and chronic. Each type affects kids differently. Acute ITP is common in young kids, usually between 2 to 6 years old. It often starts after a viral illness and symptoms show up quickly.
ITP symptoms can be scary for kids and their parents. Kids might bruise easily, have bleeding gums, and get small spots on their skin. In acute ITP, these signs usually go away in a few weeks to six months.
Chronic ITP is harder to deal with because it lasts longer. It needs ongoing care and sometimes more treatment. Knowing if it’s acute or chronic helps decide how to treat it and what to expect.
We know how tough ITP can be for families. Our team is here to help. We offer support and advice to manage symptoms and improve life for kids with ITP.
ITP in children is caused by the immune system attacking platelets. It sees platelets as foreign and destroys them. This happens after a viral infection, when the body makes antibodies that attack platelets.
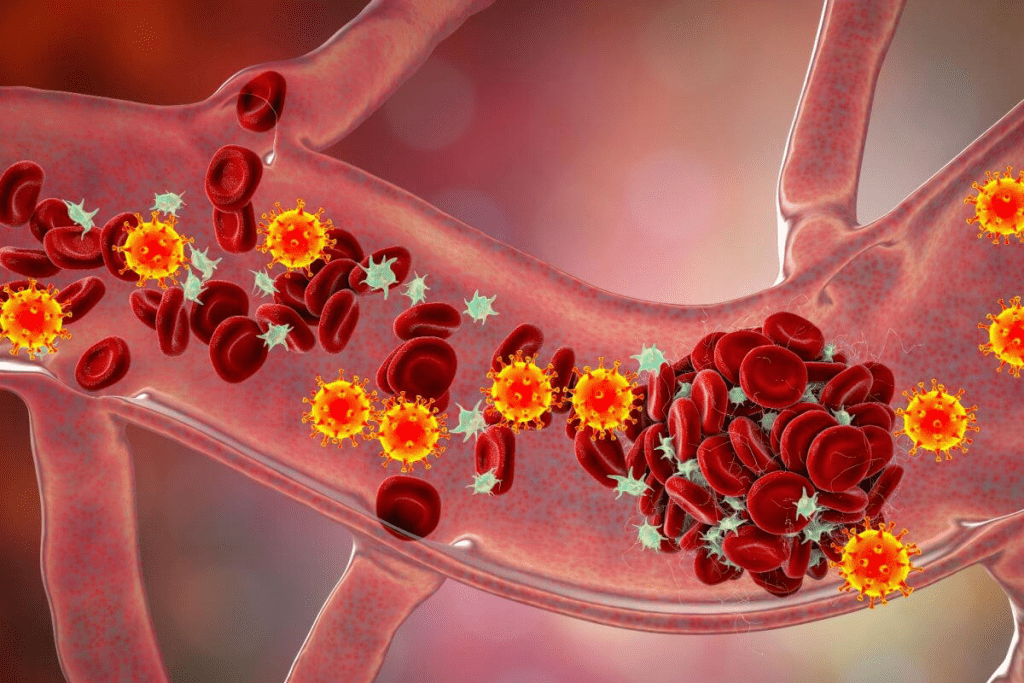
Antibodies mark platelets for destruction. This happens in the spleen, where immune cells remove them. This leads to fewer platelets, causing symptoms like bruising and bleeding.
Key factors contributing to this process include:
ITP also affects how platelets are made. The bone marrow can’t keep up with platelet loss. Autoantibodies might also harm the cells that make platelets, making it harder to have enough.
Understanding these mechanisms is key to finding better treatments. Treatments should help reduce platelet destruction and support production.
Understanding the causes of immune thrombocytopenia (ITP) in kids is key to managing it well. ITP is a complex condition. Knowing what causes it helps doctors create better treatment plans for kids.
Usually, ITP starts in kids after a viral infection, often within weeks. This shows a possible link between viruses and ITP.
Viral infections often lead to ITP in kids. The immune system might attack platelets by mistake, causing ITP. Common viruses that can trigger ITP include:
Vaccinations can also trigger ITP in kids, though it’s rare. It’s important for parents and doctors to know this. ITP might happen after a vaccine because of how the immune system reacts.
Studies are ongoing to understand the link between vaccines and ITP. They aim to find ways to lower the risk of ITP after getting vaccinated.
Understanding the genetic factors behind Immune Thrombocytopenia (ITP) in kids is key. ITP is not contagious, but genetics might play a big role in it.
Research shows that family history and hereditary factors can increase a child’s risk of ITP. Kids with a family history of autoimmune diseases might be more likely to get ITP.
Family history can give clues about genetic risks for ITP. Kids with relatives who have autoimmune diseases, like ITP, might be at higher risk. This hints at a possible genetic link that affects the immune system.
Key considerations include:
Researchers are looking into genetic markers linked to ITP risk. Finding these markers could help us understand ITP better and find new treatments.
They’re studying genes related to immune response and platelet production. Knowing these genetic factors can help us manage ITP in kids better.
By studying ITP’s genetic roots, we can better diagnose and treat it. Our team is dedicated to leading in research and care for kids with ITP.
Studying ITP in kids helps us improve how we diagnose and treat it. ITP, or Immune Thrombocytopenia, is when the immune system attacks platelets, leading to low counts. Knowing how common it is helps doctors find better ways to manage it.
ITP can happen at any age in kids, but it’s more common in some groups. The average age when kids are diagnosed with chronic ITP is about 7 years old. In the U.S., it affects around four to eight kids per 100,000 under 15 each year.
Boys and girls are equally likely to get ITP. But, different groups might be at higher risk. Knowing this helps doctors find and help those most in need.
Looking into ITP in kids helps us understand its effects and find new ways to help. This research is key to making diagnosis and treatment better for kids with ITP.
It’s important to know the difference between acute and chronic ITP in kids. Immune thrombocytopenic purpura (ITP) is an autoimmune disorder that lowers platelet counts. This leads to bleeding symptoms.
Acute ITP starts suddenly. Symptoms often show up quickly. Usually, it goes away within six months.
Chronic ITP lasts more than six months. It needs ongoing treatment and care.
How ITP moves from acute to chronic can depend on several things. These include the child’s age and any other health issues. We watch children with ITP to see if it will turn chronic.
There are a few things that can tell us if a child might have chronic ITP. These include:
Knowing these factors helps us manage ITP better. We work with families to keep an eye on the condition and change treatment plans if needed.
Children with chronic ITP need to see a hematologist regularly. We offer full support and advice to help families deal with chronic ITP.
It’s important to know the symptoms of primary thrombocytopenic purpura to manage it well. Kids with Immune Thrombocytopenia (ITP) show different signs that worry parents and doctors.
The main signs are purpura, bruising, petechiae, nosebleeds, and bleeding in the mouth or gums. These happen because the platelet count is low. This makes it hard for the body to clot blood.
While we know the usual signs, there are rarer ones too. Doctors need to watch out for these:
These rare signs show why a full check-up is key for kids with ITP. Spotting the right diagnosis helps avoid serious problems.
We stress the need for a detailed look at each child’s case. This includes a full medical history and physical check-up. It helps us give the right care and support to kids and their families.
Diagnosing ITP in kids starts with a detailed medical history and physical check-up. This first step helps find any possible reasons for the condition.
ITP is marked by low platelet counts, causing bruising and bleeding. The diagnosis of ITP is mainly by ruling out other causes of low platelets.
A complete blood count (CBC) is key in diagnosing ITP. It checks the number and health of blood cells. A low platelet count is a key sign of ITP, but the CBC might show other issues, too.
Other tests might include:
A leading hematologist says, “Diagnosing ITP needs both clinical checks and lab tests to confirm low platelets and rule out other causes.”
“The diagnosis of ITP is not just about the platelet count; it’s about understanding the patient’s overall clinical picture.”
When diagnosing ITP, it’s important to think of other conditions that might look similar. We must look at other reasons for low platelets, like leukemia. A detailed diagnostic process helps us accurately diagnose ITP and rule out serious conditions.
In summary, diagnosing pediatric ITP requires a detailed approach. This includes a thorough medical history, physical exam, and key lab tests. By understanding the diagnostic process and considering other conditions, we can give accurate diagnoses and effective care to kids with ITP.
Managing ITP in children is complex. It involves finding the right balance between treatment and waiting for the body to heal itself. The decision to treat or not depends on several things. These include how bad the symptoms are, the platelet count, and the child’s overall health.
Not every child with ITP needs treatment. For many, just watching their platelet levels and taking steps to avoid bleeding is enough. Guidelines suggest watching closely if symptoms are mild and platelet counts are high. But, if symptoms are severe or there’s a lot of bleeding, treatment is needed.
“The goal of treatment is to achieve a safe platelet count to prevent bleeding complications, not to get it back to normal,” guidelines say. We look at different treatments like corticosteroids, IVIG, and sometimes thrombopoietin receptor agonists.
New studies show promise with treatments like avatrombopag. It’s a thrombopoietin receptor agonist that can help up to 28% of children who didn’t respond to other treatments.
Avatrombopag boosts platelet production, giving hope to children who didn’t get better with usual treatments. We’re excited about the chance for better care for kids with ITP.
In conclusion, treating ITP in children is very specific. It’s all about finding the right balance between treatment and waiting for the body to heal. As new treatments come along, we keep working to make life better for our young patients.
ITP in kids is a complex mix of immune system factors and the chance for spontaneous recovery. Knowing this natural path is key for managing hopes and making smart treatment choices.
About one-third of chronic ITP cases in kids see spontaneous remissions in three years. This shows why constant monitoring and support are so important. The body stops making antibodies that attack platelets, and the disorder goes away by itself.
A study in the Yonsei Medical Journal found that knowing the pathophysiology of ITP helps predict outcomes.
Several things can affect a child’s chance of spontaneous recovery from ITP. These include the child’s age at diagnosis, the first platelet count, and other health issues. Kids with milder thrombocytopenia symptoms might have a better chance of getting better on their own.
We know every child’s fight with ITP is different. Our team is committed to giving full support on their journey. By understanding what affects spontaneous recovery, we can tailor our care to meet each child’s needs.
Children with ITP can live active lives with the right care. A good plan includes lifestyle changes, safety steps, and education. This helps them join in daily life and social events.
Children with ITP should avoid some activities to prevent bleeding. Contact sports like football or hockey are not safe because they raise injury and bleeding risks. Also, activities that could cause head injuries, like biking or skateboarding, should be carefully thought about.
It’s important to use caution with activities. Supervision and safety gear can help, but each activity needs to be checked for safety.
Medicines like aspirin or ibuprofen can increase bleeding risks. Parents and caregivers should talk to their healthcare provider before giving these medicines to their child.
ITP affects a child’s school and social life. Talking to teachers and school staff is important to meet the child’s needs. This might mean changing physical education to reduce injury risks.
Children with ITP should join in safe social activities. Support from family, friends, and groups helps with the emotional side of ITP. Connecting with others who understand can build a supportive community.
With the right precautions, children with ITP can have a full life. They can fully participate in school and social activities. Our team offers support and guidance to families dealing with ITP.
We’ve looked into immune thrombocytopenia, a condition where the immune system attacks platelets. This leads to thrombocytopenic purpura in kids. New research has helped us understand this better and find new ways to treat it.
At liv hospital.com, we’re all about top-notch healthcare for international patients. New studies show therapies like Avatrombopag work well for kids with ITP. We’re here to give the best care to kids with ITP and support their families every step of the way.
We keep up with the latest in medical research to help our patients. Our goal is to give every child the best treatment and support they need. We’re all about caring for kids with ITP and helping them thrive.
ITP is an autoimmune disorder. It causes low platelet counts. This leads to symptoms like easy bruising and bleeding gums.
Symptoms include easy bruising and bleeding gums. Petechiae and severe bleeding can also occur. Our team is skilled in identifying these symptoms.
Viral infections and vaccinations can trigger ITP. Knowing these triggers is key to managing the condition.
There’s evidence of genetic predispositions. But the exact hereditary factors are being researched. Our experts are leading this research.
Acute ITP usually gets better quickly. Chronic ITP lasts longer. Knowing these differences is important for managing the condition.
Diagnosis involves medical history, physical exam, and lab tests. Tests like a Complete Blood Count (CBC) are used. They help rule out other conditions.
Treatment options range from watching the condition to using new therapies like avatrombopag. Our team keeps up with the latest treatments.
Some children get better on their own. Others need ongoing care. Understanding ITP’s natural course helps in making decisions.
With the right management, children with ITP can live active lives. Our team offers full support for this.
The outlook depends on whether it’s acute or chronic. Our team is dedicated to providing the best care and support.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!