Last Updated on November 13, 2025 by
Quickly raising platelet counts is key for patients with immune thrombocytopenia (ITP). This is true before surgery or in emergencies. We need treatments that work fast and reliably. Why IVIG for thrombocytopenia? Discover the amazing benefits of IVIG for ITP (Immune Thrombocytopenia). A powerful and crucial treatment explained simply.
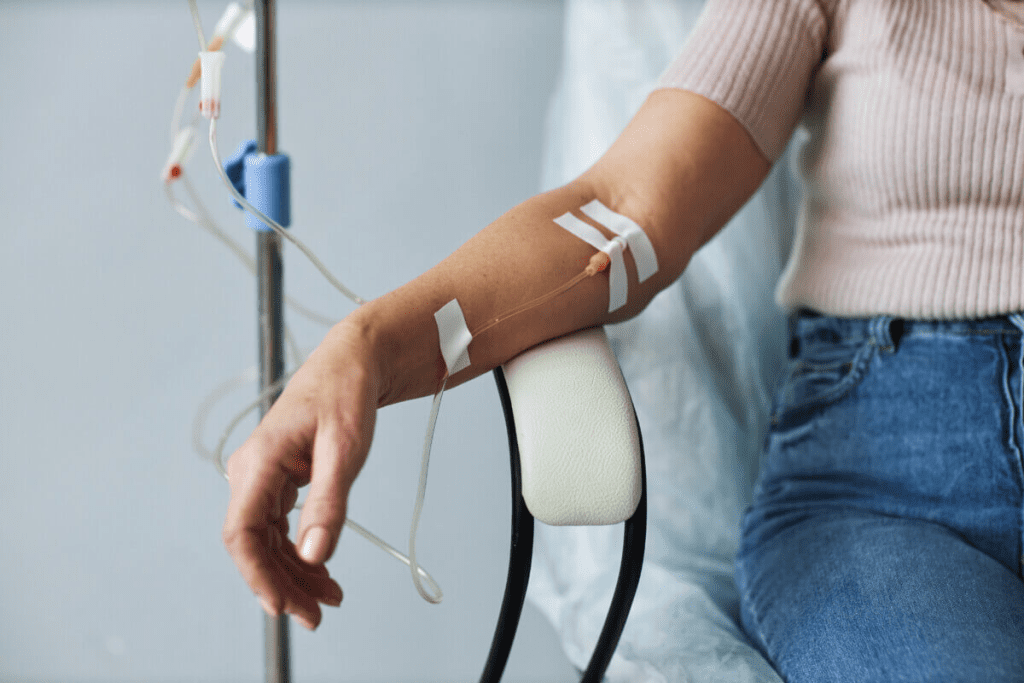
Intravenous Immunoglobulin (IVIG) is a top choice for treatment. It has been shown to be very effective, with success rates up to 80%. IVIG is made from blood products gathered from many donors.
Using IVIG, doctors can give a treatment plan backed by top medical groups.
Thrombocytopenia is when you have too few platelets in your blood. It’s a big challenge for doctors to handle. We’ll look into what it is, how it’s classified, and why it’s important.
Thrombocytopenia means you have less than 100 × 10^9/L platelets. It falls into different types, like immune thrombocytopenia (ITP), thrombotic thrombocytopenic purpura (TTP), and heparin-induced thrombocytopenia (HIT). Knowing the exact type is key to treating it right.
ITP happens when your body attacks and destroys platelets. This makes it hard to make more. Autoantibodies mark platelets for destruction, mainly in the spleen. This lowers your platelet count and raises your risk of bleeding.
Studies show IVIG can boost platelet counts in ITP patients. The success rate ranges from 63% to 89% in clinical trials.
People with ITP might have spots on their skin, bruises, and bleeding in their mouth. The risk of serious bleeding goes up when platelet counts drop. It’s important to figure out how likely you are to bleed to decide if treatment is needed.
IVIG is often the first choice to quickly raise platelet counts. This is very helpful in urgent situations.
IVIG therapy is key in treating Immune Thrombocytopenia (ITP). It’s vital to grasp IVIG’s role in this condition.
IVIG comes from human plasma, collected from many donors. It’s made through a careful process to ensure safety. This product has many antibodies, which help treat the condition.
IVIG was first used for ITP in the 1980s. It’s now a mainstay for managing severe bleeding and for patients not helped by other treatments. Its history shows how it has grown in importance in treating ITP.
Today, IVIG is recommended for ITP patients facing severe bleeding or as a last resort. For example, Liv Hospital in Turkey focuses on quality and ethical care, supporting the use of IVIG. We stick to proven protocols for the best patient results.
The main advantages of IVIG therapy for ITP are:
By knowing about IVIG’s makeup, history, and current use, we see its importance in treating ITP.
IVIG is effective in treating ITP through several mechanisms. It works in many ways to help manage ITP well.
IVIG blocks Fc receptors on immune cells. This prevents the removal of antibody-coated platelets. It helps increase platelet count.
IVIG also stops the production of antiplatelet antibodies. This adds to its effectiveness in treating ITP.
Key benefits of Fc receptor blockade include:
IVIG also changes the cytokine network and the complement system. These systems are key to ITP’s development. By reducing inflammation and preventing platelet destruction, IVIG helps platelets recover and survive.
This modulation is important for:
IVIG also affects regulatory T cells (Tregs) and dendritic cells. These cells are important for immune balance. IVIG boosts Tregs, helping to reduce autoimmune responses. It also changes how dendritic cells work, helping to regulate the immune system.
Understanding these mechanisms shows how IVIG treats ITP. It’s a key treatment for patients with this condition.
IVIG is proven to be effective in treating ITP. Recent studies show response rates from 63% to 89%. Platelet counts rise to ≥50 × 10^9/L in just 3 days. This quick action is key to managing bleeding risks and preparing for surgery.

Phase III trials have shown IVIG’s strong effectiveness in ITP treatment. Response rates range from 63% to 89%, showing a clear benefit. Platelet counts start to rise within 3 days, which is vital for urgent care.
Early treatment with IVIG is key. It quickly boosts platelet counts, reducing severe bleeding risks.
The British Journal of Haematology has explored the best IVIG dosing for ITP. The research found that the right dose is critical for success. Tailoring the dose to each patient can improve results and reduce side effects.
Personalized treatment is essential. Factors like age, weight, and health status are important. This approach helps tailor IVIG therapy for better results.
Long-term studies have shown how long IVIG’s effects last and when relapse happens. While IVIG quickly raises platelet counts, how long it lasts varies. Some patients need ongoing treatment to stay well.
Knowing how long IVIG works and when it might fail is key. This helps doctors plan better treatment. It also helps predict who will need more IVIG therapy, improving care.
IVIG is a big help for ITP patients because it quickly raises platelet counts. This is very important in hospitals where fast platelet increases are needed to stop bleeding.
Research shows IVIG therapy quickly boosts platelet counts. The median time to reach a platelet count of ≥50 × 10^9/L is within 3 days after IVIG is given. This quick rise is key to handling bleeding emergencies and getting patients ready for surgery.
Getting a platelet count of ≥50 × 10^9/L in 3 days is a big win for ITP treatment with IVIG. Clinical trials confirm, “IVIg rapidly increases platelet counts, with median counts rising ≥50 × 10^9/L within 3 days.” This fast action shows IVIG therapy works well.
“The rapid increase in platelet count following IVIG administration is a critical advantage in the management of ITP, particular in emergency situations.”
The fast recovery of platelets is very important. It lowers the chance of bleeding and lets doctors manage patients needing surgery on time. The quick action of IVIG makes it a key treatment for ITP patients.
We see how vital IVIG therapy is in medical care. Its ability to quickly raise platelet counts is a big plus. It’s a key part in treating ITP, where fast action is needed.
Administering IVIG for ITP requires careful thought. It’s important to have effective treatment plans for the best results.
IVIG dosing can vary, with the usual amount being 1g/kg. Alternative regimens are being tested to improve results and reduce side effects. We look at these options based on how well they work and what doctors recommend.
IVIG can be given in one day or over several days. Each method has its benefits. Giving it all at once is easier, but spreading it out might lessen side effects.
Using pre-medications and controlling the infusion rate are key to avoiding bad reactions. We talk about how these steps help make treatments safer and more comfortable for patients.
Knowing about these dosing and administration methods helps doctors tailor IVIG treatment for each patient. This way, they can better manage ITP.
Using IVIG in clinical practice requires careful thought about patient characteristics. It’s key in managing Immune Thrombocytopenia (ITP), for those with severe low platelet counts or at high risk of bleeding. Choosing the right patients for IVIG therapy is essential.
In emergencies or before surgery, quickly raising platelet counts is vital. IVIG is advised for ITP patients facing critical bleeding situations. It acts as an emergency rescue. “IVIG can quickly raise platelet counts, often in 24-48 hours,” making it critical in urgent cases. We give IVIG at 1g/kg, and may repeat if needed.
Some patients need special care when getting IVIG for ITP. Kids might need adjusted doses based on their weight and how they react. Pregnant women with ITP, facing severe low platelet counts or bleeding risks, may also benefit from IVIG. Elderly patients with possible health issues need close monitoring for any side effects.
It’s hard to guess who will benefit from IVIG therapy. Research points to biomarkers and certain patient traits that might help. For example, those with ITP for a shorter time and more severe low platelet counts tend to do better with IVIG. Ongoing studies aim to improve our ability to predict who will benefit, making IVIG therapy more effective.
By carefully choosing patients and tailoring IVIG therapy, we can improve treatment results and reduce risks. As we learn more about ITP and IVIG, we’ll be able to better care for our patients.
IVIG is a treatment for ITP that works differently from others. It’s important to know the good and bad of each treatment when choosing one for ITP.
Corticosteroids are often the first choice for ITP. They help by making more platelets and fewer antibodies. But, they can cause serious side effects like osteoporosis, diabetes, and increased infection risk.
How well corticosteroids work can vary. Some people see results quickly, but it’s hard to keep the platelet count up without taking them all the time.
Thrombopoietin receptor agonists (TPO-RAs) are for those who don’t respond well to first treatments. They help make more platelets and can work well for many patients. TPO-RAs are good for people with ITP that lasts a long time, when other treatments don’t work.
Rituximab is a second-line treatment for ITP. It targets B cells to reduce antibodies against platelets. It can help some patients for a long time, but it can cause reactions and weaken the immune system.
Other second-line treatments include splenectomy and more immunosuppressive drugs. Each has its own benefits and risks.
Choosing between IVIG and other treatments depends on several things. How fast you need the platelet count to rise, your health, and the chance of side effects are important. IVIG is great for quick needs, like before surgery. But treatments like TPO-RAs and rituximab might be better for long-term use.
IVIG is usually safe for treating ITP. But it’s key to manage its side effects well. Knowing the risks and taking steps to avoid them is important.
Infusion-related reactions are common with IVIG. Symptoms can be mild, like headaches, or severe, like fever. Watching patients closely during the infusion helps reduce these issues.
Though rare, serious problems like blood clots and aseptic meningitis can happen. Identifying high-risk patients is vital. Using preventive steps and careful monitoring can lower these risks.
For those at high risk, we can take steps to lower risks. This includes adjusting the dose and infusion rate of IVIG. We also use pre-medication and watch for serious signs. This approach makes treatment safer and more effective.
IVIG therapy has changed how we treat Immune Thrombocytopenia (ITP). It offers a quick and effective way to prevent serious bleeding. We’ve looked into how IVIG works, its uses, and its benefits for ITP patients.
The use of IVIG for ITP helps platelet counts recover fast. This makes it a key treatment option. It works well for 70-80% of patients, helping those at high risk of bleeding or who haven’t responded to other treatments.
At places like Liv Hospital, we support using treatments like IVIG wisely. By improving IVIG therapy, we can give better care to ITP patients. This helps improve their quality of life.
IVIG (Intravenous Immunoglobulin) is a treatment for ITP (Immune Thrombocytopenia). It involves giving antibodies from human plasma. This helps increase platelet counts in patients with low platelets.
IVIG works in several ways. It blocks Fc receptors, stops antiplatelet antibodies, and changes the immune system. These actions help treat ITP.
Studies show IVIG works well for ITP patients. It has a response rate of 63% to 89%. This makes it a good first choice for treatment.
IVIG can quickly raise platelet counts. Often, it reaches levels of ≥50 ×10^9/L in just 3 days. This is important for emergencies or before surgery.
For ITP, IVIG is usually given at 1g/kg. The dose can be spread over one or more days. Pre-medication and infusion rates are also important.
IVIG is compared to other treatments for ITP. It quickly raises platelet counts, making it great for emergencies. Corticosteroids and rituximab work differently and are chosen based on what the patient needs.
IVIG therapy can cause common side effects like infusion reactions. Serious issues like thrombosis or hemolysis can also happen. But these risks can be lowered with careful patient selection and monitoring.
Yes, IVIG can be used in special groups, like kids and pregnant women. It’s important to adjust the dose and watch the patient closely to ensure safety and effectiveness.
Predicting how well IVIG will work involves looking at patient factors and clinical details. While specific predictors are being studied, results can vary from person to person.
Immunoglobulin therapy for ITP uses IVIG to fight the immune system’s attack on platelets. This helps increase platelet counts.
Yes, IVIG is effective for thrombocytopenia, mainly in ITP. It quickly raises platelet counts and is often the first treatment choice.
Cines, D. B., & Blanchette, V. S. (2002). Immune thrombocytopenic purpura. New England Journal of Medicine, 346(13), 995“1008. https://pubmed.ncbi.nlm.nih.gov/11907253/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!