Knowing about kappa light chain amyloidosis is vital for both patients and doctors. This rare disease needs quick diagnosis and special care. It happens when plasma cells make too many kappa light chains.kappa light chain amyloidosisBone Marrow Diseases List: 15 Common Disorders and Their Key Features
Amyloidosis is when proteins called fibrils build up outside cells. Immunoglobulin light chain (AL) amyloidosis is a big reason for amyloid neuropathy. This is when proteins damage important organs.
With the right diagnosis and treatments, patients can live longer. We will dive into the details of this disease and how it affects life span.
Key Takeaways
- Kappa light chain amyloidosis is a rare plasma cell disorder.
- Early detection is critical for effective treatment.
- AL amyloidosis is a major cause of amyloid neuropathy.
- Modern treatment protocols improve survival outcomes.
- Understanding the condition is key to determining life expectancy.
The Nature of Kappa Light Chain Amyloidosis
Kappa light chain amyloidosis is marked by amyloid fibrils in organs, causing them to fail. It’s caused by abnormal immunoglobulin light chains from plasma cell dyscrasias.
Definition and Pathophysiology
Kappa light chain amyloidosis, or AL amyloidosis, is when light chains build up in tissues, harming organs. It starts with a plasma cell making a monoclonal serum protein. This protein then misfolds and forms amyloid fibrils.
AL amyloidosis is systemic, affecting many organs like the kidneys, heart, liver, and nerves. The disease’s impact and symptoms vary based on the organs affected and how much amyloid is present.
How It Differs from Other Types of Amyloidosis
AL amyloidosis is different from AA and ATTR amyloidosis in cause and symptoms. AA is linked to chronic inflammation, and ATTR is about transthyretin protein. But AL amyloidosis comes from plasma cell dyscrasias.
Knowing how kappa light chain amyloidosis is unique helps doctors diagnose and treat it better. By understanding its differences, we can create better treatment plans for patients with this complex disease.
Causes and Mechanisms of Kappa Light Chain Amyloidosis

Kappa light chain amyloidosis starts with abnormal plasma cells in the bone marrow. These cells make too many light chains. The light chains then misfold and form amyloid fibrils, damaging organs.
Plasma Cell Dyscrasia Explained
Plasma cell dyscrasia means plasma cells make too much of one light chain type. In kappa light chain amyloidosis, it’s kappa light chains. This leads to too many light chains that misfold into amyloid fibrils. Genetics and environment play a role in this condition.
The table below summarizes the key aspects of plasma cell dyscrasia in the context of kappa light chain amyloidosis:
|
Characteristics |
Description |
|---|---|
|
Abnormal Plasma Cells |
Proliferation of plasma cells that produce excess kappa light chains |
|
Light Chain Production |
Overproduction of kappa light chains by abnormal plasma cells |
|
Misfolding and Aggregation |
Misfolded light chains aggregate into amyloid fibrils |
Process of Amyloid Fibril Formation
Amyloid fibril formation is key in kappa light chain amyloidosis. Kappa light chains misfold into beta-pleated sheets and form fibrils. This misfolding is often due to mutations or other changes in the light chain structure. These fibrils harm organs like the heart, kidneys, and liver.
Knowing how kappa light chain amyloidosis works is vital for better treatments. By focusing on the plasma cell dyscrasia and amyloid fibril formation, we can help patients live better lives.
Epidemiology and Risk Factors
The study of kappa light chain amyloidosis shows us how common it is and who is at risk. It’s a rare disease, so knowing these details helps doctors catch it early and treat it better.
Incidence and Prevalence Statistics
Kappa light chain amyloidosis, or AL amyloidosis, happens to less than 1 person per 100,000 each year. It mainly affects a certain group of people, based on their genes and age.
Most people with AL amyloidosis are over 60, with the biggest number between 60 and 70. It’s a bit more common in men than in women.
|
Age Group |
Incidence Rate (per 100,000) |
|---|---|
|
50-59 |
0.5 |
|
60-69 |
1.2 |
|
70+ |
1.8 |
Demographic and Genetic Risk Factors
There are several things that make some people more likely to get kappa light chain amyloidosis. These include:
- Age: The risk goes up a lot after 50.
- Gender: Men are a bit more likely to get it than women.
- Family History: If your family has had plasma cell dyscrasias or amyloidosis, you might be at higher risk.
- Genetic Predisposition: Some genetic mutations can make you more likely to get AL amyloidosis.
Knowing these risk factors helps doctors spot people who might get it and start checking them early.
By understanding who is at risk for kappa light chain amyloidosis, we can help patients get better sooner. This is through early diagnosis and treatment plans that fit each person’s needs.
Clinical Manifestations and Organ Involvement
Kappa light chain amyloidosis can affect several organs, including the heart, kidneys, and gastrointestinal tract. This leads to complex clinical presentations. The extent and severity of organ involvement significantly impact patients’ quality of life and life expectancy.
Cardiac Manifestations
Cardiac involvement is a major determinant of survival in patients with kappa light chain amyloidosis. Amyloid deposition in the heart can lead to restrictive cardiomyopathy, arrhythmias, and orthostatic hypotension. We will discuss the various cardiac manifestations and their implications on patient outcomes.
The symptoms of cardiac amyloidosis include shortness of breath, fatigue, and palpitations. Early diagnosis is key to manage these symptoms effectively and improve al amyloidosis life expectancy.
Renal Manifestations
Renal involvement is another common feature of kappa light chain amyloidosis, often presenting as nephrotic syndrome or renal failure. The deposition of amyloid fibrils in the kidneys can lead to progressive kidney damage. Understanding the renal manifestations is vital for managing renal amyloidosis effectively.
Patients with renal amyloidosis may exhibit proteinuria, hematuria, and decreased renal function. Monitoring renal function closely is essential for timely intervention.
Gastrointestinal, Nervous System, and Liver Involvement
Gastrointestinal symptoms can include weight loss, diarrhea, and abdominal pain due to amyloid deposition in the GI tract. Nervous system involvement may manifest as peripheral neuropathy or autonomic dysfunction. Liver involvement, though less common, can lead to hepatomegaly and abnormal liver function tests.
We must consider these varied manifestations when diagnosing and managing kappa light chain amyloidosis. A thorough assessment is necessary to address the multi-organ involvement effectively.
The following table summarizes the clinical manifestations and organ involvement in kappa light chain amyloidosis:
|
Organ/System |
Common Manifestations |
Clinical Implications |
|---|---|---|
|
Cardiac |
Restrictive cardiomyopathy, arrhythmias |
Impacts survival, necessitates early diagnosis |
|
Renal |
Nephrotic syndrome, renal failure |
Requires close monitoring of renal function |
|
Gastrointestinal |
Weight loss, diarrhea, abdominal pain |
Affects nutritional status and quality of life |
|
Nervous System |
Peripheral neuropathy, autonomic dysfunction |
Impacts patient mobility and autonomic function |
|
Liver |
Hepatomegaly, abnormal liver function tests |
Less common, but significant when present |
Understanding these clinical manifestations and organ involvements is key for managing kappa light chain amyloidosis effectively. This improves patient outcomes.
Diagnosis of Kappa Light Chain Amyloidosis
Diagnosing kappa light chain amyloidosis is complex. It involves several steps. Accurate diagnosis is key to starting the right treatment and helping patients.
Serum Free Light Chain Assays
Serum free light chain (FLC) assays are very important. They check the levels of free kappa and lambda light chains in the blood. This helps find the abnormal light chain production seen in this condition.
An abnormal kappa to lambda ratio can show a plasma cell dyscrasia. This means there’s a problem with plasma cells.
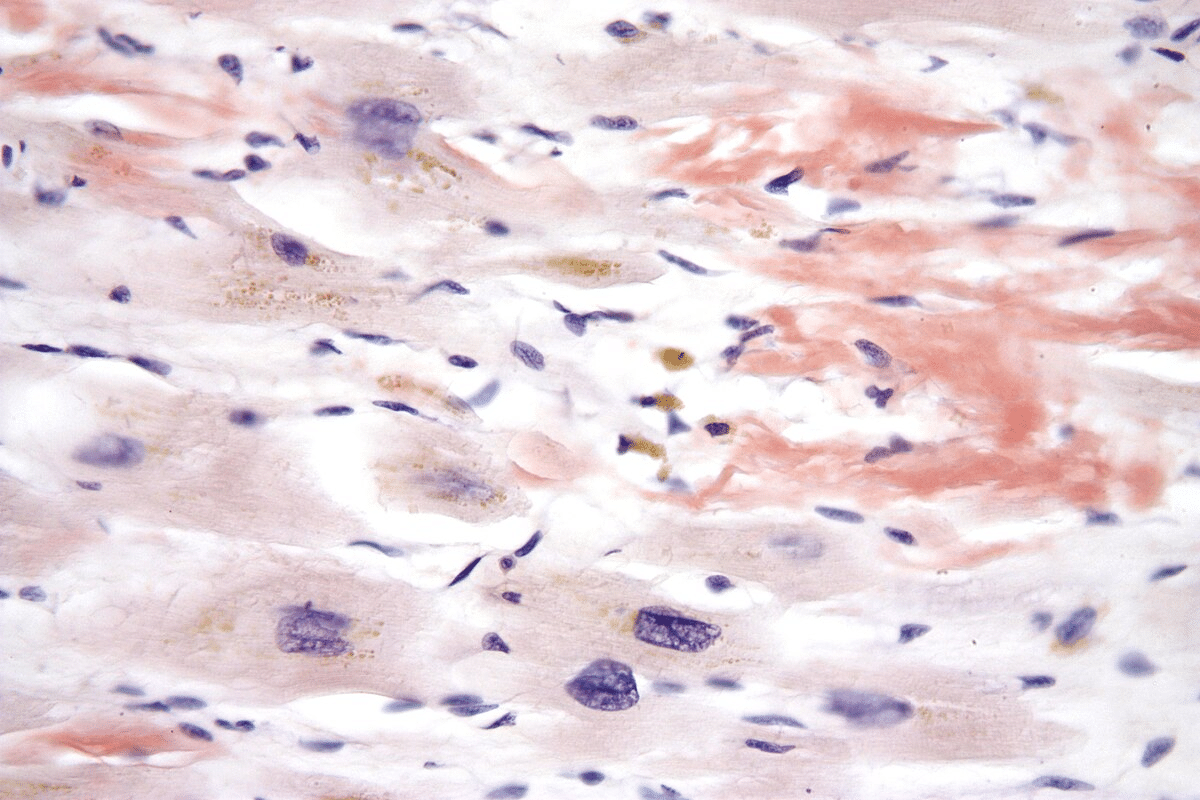
Tissue Biopsy and Congo Red Staining
Tissue biopsy is the top way to diagnose amyloidosis. The biopsy is stained with Congo red dye. Under polarized light, amyloid fibrils show apple-green birefringence.
This special staining is a clear sign of amyloidosis. It shows there are amyloid deposits in the tissues.
Organ Function Assessment
Checking how well organs work is key in diagnosing and managing kappa light chain amyloidosis. Tests are done to see how much organs are affected. These include echocardiography for the heart, serum creatinine and urine protein for the kidneys, and liver function tests.
These tests help understand how the disease affects different organs. They guide treatment choices.
Early and accurate diagnosis of kappa light chain amyloidosis is vital. It leads to better management and improves patients’ quality of life. By using serum free light chain assays, tissue biopsy with Congo red staining, and organ function tests, doctors can diagnose more accurately.
Staging Systems and Disease Classification
Getting the right stage of kappa light chain amyloidosis is key. It helps doctors predict how well a patient will do and what treatment to use. Staging systems show how far the disease has spread, which is vital for choosing the best treatment.
Medical organization Staging System
The Medical organization staging system is well-known for classifying kappa light chain amyloidosis. It uses certain biomarkers to figure out the disease stage. This helps doctors guess how well a patient will do.
Key components of the Medical organization staging system:
- Cardiac troponin T (cTnT) levels
- N-terminal pro-b-type natriuretic peptide (NT-proBNP) levels
- Serum free light chain levels
Doctors use these biomarkers to sort patients into different risk groups. This helps them make better treatment choices and improve patient results.
Biomarkers and Prognostic Indicators
Besides the Medical organization system, other biomarkers and indicators are important for managing kappa light chain amyloidosis. These include:
- Cardiac biomarkers: High levels of cardiac troponins and NT-proBNP mean the heart is involved and the outlook is worse.
- Serum free light chains: The gap between involved and uninvolved free light chains (dFLC) is a big factor in predicting how well a patient will do.
- Renal function: Checking serum creatinine and estimated glomerular filtration rate (eGFR) shows how much the kidneys are affected.
Using these biomarkers with the Medical organization system makes disease classification and prediction more accurate. This leads to more tailored and effective treatments for patients.
Life Expectancy with Kappa Light Chain Amyloidosis
The outlook for those with kappa light chain amyloidosis depends on several key factors. These include the disease stage and how well treatment works. Knowing these factors helps doctors give a better prognosis and make treatment plans.
Median Survival Rates by Stage
Survival rates for kappa light chain amyloidosis change based on the disease stage at diagnosis. Research shows that early diagnosis leads to better survival rates. Early treatment is key to a longer life.
Recent data shows that patients with this condition can live about 3 years with treatment. Without treatment, the survival time drops to less than 2 years. The disease stage is a big factor in how long someone can live.
Impact of Free Light Chain Levels on Survival
Free light chain levels are important for predicting survival in kappa light chain amyloidosis. High levels mean a worse prognosis. Keeping free light chain levels low is a big part of treatment.
Studies show that patients with lower free light chain levels do better. So, lowering these levels through treatment is a main goal in managing the disease.
Factors That Influence Life Expectancy
Many things affect how long someone with kappa light chain amyloidosis can live. These include how much the disease affects organs, how well treatment works, and the patient’s overall health. How much the heart is affected is very important.
- Disease stage at diagnosis
- Response to treatment
- Levels of free light chains
- Extent of organ involvement
Understanding these factors helps doctors make treatment plans that fit each patient’s needs. This can lead to better outcomes.
Treatment Approaches for AL Amyloidosis
AL amyloidosis treatment aims to stop the production of bad proteins and fix organ damage. The main goal is to get rid of the plasma cell clone that makes these proteins.
Chemotherapy Regimens
Chemotherapy is a key part of AL amyloidosis treatment. It uses drugs like cyclophosphamide, bortezomib, and dexamethasone. The choice of treatment depends on the patient’s health and how much the organs are affected.
Chemotherapy’s goal is to stop the production of bad proteins. We use different chemotherapy plans. We check how well the treatment is working by looking at serum free light chains and organ function.
Autologous Stem Cell Transplantation
Autologous stem cell transplantation (ASCT) is an option for some patients with AL amyloidosis. It collects the patient’s stem cells, then uses high-dose chemotherapy to kill the bad plasma cells. Then, the stem cells are put back to help the bone marrow recover.
ASCT can offer a strong and lasting response for eligible patients. But, it’s only for those with little organ damage and good health.
Novel Agents and Targeted Therapies
New treatments and targeted therapies are changing how we treat AL amyloidosis. Daratumumab, a monoclonal antibody, has shown great promise. Other new treatments include proteasome inhibitors and immunomodulatory drugs.
These new treatments give hope to patients who don’t respond well to traditional therapies. We’re studying these agents to see how they can help in treating AL amyloidosis, alone or with other treatments.
How Treatment Affects Life Expectancy
Understanding how treatment impacts life expectancy is key for managing Kappa Light Chain Amyloidosis. Treatment plays a big role in how well patients do and their quality of life.
Survival Rates With and Without Treatment
There’s a big difference in survival rates between treated and untreated patients. Effective treatments can greatly improve survival rates and outcomes. For example, a study found that treated patients lived longer than those without treatment.
Untreated patients usually live 6-12 months. But, treated patients can live up to 5 years or more. This depends on the treatment’s success and the disease’s stage.
“The introduction of novel therapies has revolutionized the management of AL Amyloidosis, improving survival rates.”
Response Assessment and Its Correlation with Outcomes
Checking how well treatment works is vital in managing Kappa Light Chain Amyloidosis. The better the treatment response, the better the long-term results. A deeper response to therapy means better survival rates and organ function.
Regular checks with serum free light chain assays help adjust treatments for better results. For instance, a complete hematologic response leads to better survival and less organ damage. But, a poor response might mean changing the treatment plan.
We stress the need for a treatment plan that fits each patient’s needs. This approach can greatly improve life expectancy and outcomes.
Recent Advances in Research and Emerging Therapies
Medical research has made big strides in finding new treatments for Kappa Light Chain Amyloidosis. We’re seeing a big change in how we treat this disease. This change comes from a better understanding of what causes it.
“The future of Kappa Light Chain Amyloidosis treatment lies in targeted therapies that can effectively reduce amyloid burden and improve patient outcomes,” says Medical Expert, a leading researcher in the field.
Monoclonal Antibodies and Immunotherapies
Monoclonal antibodies and immunotherapies are showing great promise in treating Kappa Light Chain Amyloidosis. These treatments aim to target specific parts of the amyloid fibrils. They can either bind directly to the fibrils or change how the immune system reacts to them.
Monoclonal antibodies are special because they can target only the diseased cells or proteins. This could mean fewer side effects compared to traditional chemotherapy. Early results from clinical trials are looking good, showing these therapies can improve organ function and survival rates.
Amyloid Fibril-Targeting Approaches
Research is also focusing on amyloid fibril-targeting approaches. These strategies aim to stop or remove amyloid deposits. The goal is to directly tackle the disease by targeting the amyloid fibrils.
Early studies suggest compounds that can bind to and stabilize amyloid fibrils are showing promise. They might prevent more deposits and help clear them out. These treatments are just starting out, but they could be a game-changer for Kappa Light Chain Amyloidosis treatment.
As research keeps moving forward, we’ll see more treatment options for Kappa Light Chain Amyloidosis. This could bring hope for better outcomes and a better quality of life for patients.
Conclusion
We’ve looked into kappa light chain amyloidosis, a serious condition needing quick diagnosis and specific treatments. These steps are key to better life expectancy and treatment results. Understanding the disease’s causes, symptoms, and how treatments work is vital.
New research and treatments bring hope to those with this condition. Using new medicines, targeted therapies, and better tests can improve care. This could also help patients live longer.
As we learn more about kappa light chain amyloidosis, a team effort is needed for the best care. Healthcare teams working together can provide the detailed care patients need. This approach helps manage the complex challenges of this condition.
FAQ
What is kappa light chain amyloidosis?
Kappa light chain amyloidosis, also known as AL amyloidosis, is a condition. It happens when plasma cells make too many light chains. These chains then form amyloid fibrils and deposit in organs, causing damage.
What are the causes of kappa light chain amyloidosis?
Kappa light chain amyloidosis is caused by abnormal plasma cells. These cells produce too many light chains. The light chains then misfold and form amyloid fibrils, which damage organs.
How is kappa light chain amyloidosis diagnosed?
Diagnosing kappa light chain amyloidosis involves several steps. Serum free light chain assays and tissue biopsy with Congo red staining are used. Also, checking organ function is important. Early diagnosis is key to starting treatment and improving life expectancy.
What is the Medical organization staging system for kappa light chain amyloidosis?
The Medical organization staging system is a way to classify kappa light chain amyloidosis. It uses biomarkers to determine the disease stage and prognosis. This helps in choosing the right treatment.
How does treatment impact life expectancy in kappa light chain amyloidosis?
Treatment greatly affects life expectancy in kappa light chain amyloidosis. Effective treatments can improve survival rates and quality of life. It’s important to assess how well the treatment is working.
What are the treatment approaches for AL amyloidosis?
Treatment for kappa light chain amyloidosis aims to reduce abnormal light chains and manage organ damage. It includes conventional chemotherapy, autologous stem cell transplantation, and newer targeted therapies.
What are the emerging therapies for kappa light chain amyloidosis?
Research is ongoing for kappa light chain amyloidosis. New therapies are being explored. Monoclonal antibodies, immunotherapies, and amyloid fibril-targeting approaches show promise.
What are the factors that influence life expectancy in kappa light chain amyloidosis?
Life expectancy in kappa light chain amyloidosis depends on several factors. Disease stage at diagnosis, response to treatment, and free light chain levels are important. Understanding these factors helps in giving a more accurate prognosis.
Is kappa light chain amyloidosis considered a cancer?
Kappa light chain amyloidosis is linked to a plasma cell dyscrasia, which is related to cancer. But it’s not classified as a traditional cancer. It shares similarities with multiple myeloma and other plasma cell disorders.
What is the life expectancy for patients with AL amyloidosis?
Life expectancy for patients with AL amyloidosis varies. It depends on the disease stage, response to treatment, and organ involvement. Understanding these factors is key to determining a more accurate prognosis.
References
Government Health Resource. Kappa Light Chain Amyloidosis: Diagnosis and Life Expectancy. Retrieved from https://www.cedars-sinai.org/health-library/diseases-and-conditions/a/al-amyloidosis.html






