Last Updated on December 3, 2025 by mcelik

Learn about epidural steroid limits and how many injections are safe for managing chronic spinal pain.. Millions of people worldwide get epidural steroid injections each year to ease spinal pain. These injections are often effective, but worries about their long-term safety are growing. Doctors are debating this issue a lot.
We need to know how many times these injections are safe to use. It’s key to look at the latest studies and advice. We’ll dive into the knowledge on safe epidural injections and share expert tips on their use.
Key Takeaways
- Understanding the risks associated with epidural steroid injections.
- Current guidelines for safe epidural injection practices.
- Expert recommendations for managing spinal pain.
- The importance of personalized treatment plans.
- Future directions in epidural steroid injection research.
Understanding Epidural Steroid Injections

Epidural steroid injections are a treatment for back pain. They are popular because they work well for chronic pain. This pain doesn’t get better with usual treatments.
What Are Epidural Steroid Injections?
Epidural steroid injections put a mix of a corticosteroid and a local anesthetic near the spinal cord. This area is outside the sac that holds spinal fluid and nerves. The corticosteroid cuts down inflammation, and the anesthetic numbs the area, giving quick pain relief.
The doctor uses X-rays to guide the injection. This makes sure the injection is placed right. This accuracy helps the treatment work better and lowers side effects.
How Epidural Injections Work
Epidural steroid injections work by reducing inflammation. The steroids in the injection cut down the swelling around the nerves. This is often where pain comes from in cases like herniated discs and spinal stenosis.
- Reducing inflammation around the nerves
- Decreasing pain signals to the brain
- Improving mobility and function
By tackling the pain’s source, these injections can give a lot of relief. This lets patients do better in physical therapy and other rehab programs.
Types of Steroids Used in Epidural Injections
The steroids used most often are triamcinolone, methylprednisolone, and dexamethasone. Each steroid has its own strengths and how long it lasts. This affects which steroid is best for a patient.
Choosing a steroid depends on the patient’s health, the condition being treated, and the doctor’s choice. For example, dexamethasone starts working fast, while triamcinolone lasts longer.
Medical Conditions Treated with Epidural Steroid Injections
Epidural steroid injections are a versatile treatment for many spinal conditions. They help manage pain and discomfort caused by several spinal disorders. These injections reduce inflammation and pain.
Spinal Stenosis
Spinal stenosis is when the spinal canal narrows. This puts pressure on the spinal cord and nerves. It leads to pain, numbness, and weakness in the back, legs, or arms. Epidural steroid injections can ease symptoms by reducing swelling and inflammation.
Herniated Discs
A herniated disc happens when the soft inner gel leaks out. This can irritate nearby nerves. Epidural steroid injections help by reducing inflammation caused by herniated discs. This relieves pain and discomfort.
Radiculopathy and Sciatica
Radiculopathy is a nerve root disease causing pain, numbness, or weakness. Sciatica is a type of radiculopathy affecting the sciatic nerve. Epidural steroid injections can manage pain by reducing nerve root inflammation.
Other Conditions
Epidural steroid injections also treat other spinal disorders. These include degenerative disc disease, spondylolisthesis, and facet joint syndrome. These conditions involve inflammation and pain, which can be managed with targeted steroid injections.
The following table summarizes the medical conditions treated with epidural steroid injections and their characteristic symptoms:
| Condition | Symptoms | Treatment Benefit |
| Spinal Stenosis | Pain, numbness, weakness in back, legs, or arms | Reduces inflammation, relieves pressure on spinal cord |
| Herniated Discs | Pain, inflammation, nerve irritation | Decreases inflammation, alleviates nerve irritation |
| Radiculopathy and Sciatica | Pain, numbness, weakness in arms or legs | Reduces nerve root inflammation, relieves pain |
| Degenerative Disc Disease | Chronic pain, inflammation | Manages pain and inflammation |
Epidural Steroid Limits
Doctors follow strict rules when they give epidural steroid shots. These rules are key to keeping patients safe and making sure the treatment works.
FDA Recommendations
The FDA has set rules for using epidural steroid injections. The FDA says to limit injections to three per year to avoid risks from too much steroid. This rule helps prevent side effects from the steroids.
American Society of Interventional Pain Physicians Guidelines
The American Society of Interventional Pain Physicians (ASIPP) also has guidelines. According to ASIPP, how often to give injections depends on how the patient responds and the doctor’s judgment. They advise spacing out injections to avoid too much steroid.
| Organization | Guideline | Key Recommendation |
| FDA | Limit on Injection Frequency | Maximum of 3 injections per year |
| ASIPP | Patient Response-Based Frequency | Spacing injections based on clinical judgment |
| International Standards | Varying Guidelines | Differing recommendations based on regional practices |
International Standards and Variations
Guidelines for epidural steroid injections vary worldwide. Countries and medical groups have their own rules based on local practices and data. Healthcare providers need to keep up with both national and international guidelines to give the best care.
By following these guidelines, doctors can make sure epidural steroid injections are safe and work well.
Research on Safe Frequency of Epidural Injections
Research has given us important insights into how often epidural steroid injections should be given. These injections are used to treat many spinal problems. Knowing the best frequency is key.
Clinical Studies on Injection Frequency
Many studies have looked into how often these injections should be given. A study in the Spine Journal found that giving injections every 3 months is safe and effective. Another study said that the frequency should depend on each patient’s needs and how they react to the injections.
These studies show that there’s no one right answer for everyone. The condition being treated, the patient’s health, and how they’ve reacted to injections before are all important. They help decide how often injections should be given.
Long-term Safety Research
Long-term studies have raised concerns about the effects of these injections on the body. They can affect bone density and the body’s stress response system. Giving injections too often may increase these risks.
A study in the Journal of Pain Research said it’s important to choose patients carefully and watch them closely. For some, other treatments might be safer in the long run.
Evidence-Based Recommendations
Guidelines based on research suggest using these injections wisely. Doctors should think about the patient’s condition, how they’ve reacted to injections before, and the possible risks. The American Society of Interventional Pain Physicians (ASIPP) recommends spacing out injections and limiting their number.
We suggest that doctors tailor their approach to each patient. They should consider individual factors and the latest research. This way, we can make the most of these injections while keeping risks low.
Factors Affecting Safe Injection Limits
The safety of epidural steroid injections depends on several factors. These include the patient’s age and overall health. It’s important to consider these factors to find the safe injection limits for each person.
Patient Age and Health Status
Patient age and health status are key in setting safe injection limits. Older patients or those with health issues may face more risks from steroids. We adjust the treatment to meet each person’s needs.
For instance, older adults may experience conditions such as diabetes or osteoporosis. These can be made worse by steroid injections. So, we carefully check the patient’s health before starting treatment.
Underlying Medical Conditions
Medical conditions can affect how safe and effective epidural steroid injections are. Issues like spinal stenosis or herniated discs can influence the treatment’s success and how the patient responds.
We take these conditions into account when deciding on safe injection limits. For instance, those with severe spinal stenosis might need more careful dosing and injection frequency.
Previous Response to Injections
A patient’s past response to epidural steroid injections is very telling. If they’ve had a good response, we might continue the treatment, adjusting as needed.
But if there have been bad effects or no improvement, we might need to rethink the treatment plan. We could look into other options.
Anatomical Injection Location
The location of the injection is also very important. Injections in different areas, like the neck, chest, or lower back, have different risks and benefits.
For example, injections in the neck might have higher risks than those in the lower back. We consider these differences when planning the treatment.
| Factor | Considerations | Impact on Safe Injection Limits |
| Patient Age | Older patients may have more comorbidities | May require reduced frequency or dosage |
| Health Status | Compromised health may increase susceptibility to side effects | Careful assessment needed before treatment |
| Underlying Medical Conditions | Conditions like spinal stenosis or herniated discs | May affect injection success and patient response |
| Previous Response to Injections | Positive or negative response to previous injections | Informs future treatment plans and adjustments |
| Anatomical Injection Location | Cervical, thoracic, or lumbar regions | Varying risks and benefits based on location |
Short-Term vs. Long-Term Epidural Steroid Injection Safety
Epidural steroid injections are used to treat chronic pain. They are safe in the short term but have long-term risks. It’s important to know about these risks to help patients.
Immediate Safety Concerns
These injections are safe when done by experts. But, there are risks like infection and allergic reactions. There’s also a chance of temporary pain increase.
Common short-term side effects include:
- Temporary pain flare-up
- Facial flushing
- Insomnia
- Increased blood sugar levels
Cumulative Effects Over Time
Getting many injections can lead to steroid buildup in the body. This can harm bone density and affect blood sugar and hormones. We must watch for these effects to keep patients safe.
Lifetime Exposure Considerations
Younger patients might need many injections over years. The long-term effects of these injections are not fully known. We must think about risks like osteoporosis and hormonal imbalances when planning treatment.
| Safety Consideration | Short-Term Implications | Long-Term Implications |
| Infection Risk | Low, but possible with any invasive procedure | Increased with multiple procedures over time |
| Temporary, such as facial flushing or insomnia | Potential for systemic effects like bone density loss or hormonal changes | |
| Pain Relief Efficacy | Effective for many patients in the short term | May diminish over time with repeated injections |
Knowing the safety of epidural steroid injections helps us care for patients better. We can make better treatment plans with this knowledge.
Common Epidural Steroid Injection Side Effects
It’s important to know about the side effects of epidural steroid injections. This treatment can help with pain but comes with risks.
Minor Side Effects
Minor side effects are common and usually go away by themselves. These might include:
- Temporary increase in pain
- Insomnia or sleep disturbances
- Facial flushing
- Minor bleeding or bruising at the injection site
- Headaches
Most people only get mild side effects, if any. But, it’s key to watch for them and talk to your doctor if you notice anything.
Moderate Complications
Moderate complications can happen and need medical help. These might include:
- Infection at the injection site
- Nerve damage or irritation
- Allergic reactions to the steroid or other parts of the injection
- Changes in blood sugar levels, which can be a problem for diabetics
These complications are not as common as minor side effects. But, they can really affect your life.
Severe Adverse Events
Severe adverse events are rare but can be serious. These might include:
- Paralysis or loss of sensation in the limbs
- Severe allergic reactions, including anaphylaxis
- Spinal cord injury or damage
- Stroke or other heart problems
It’s vital to know about these risks. Talk to your doctor about your own risk factors.
The table below shows the common side effects of epidural steroid injections:
| Side Effect Category | Examples | Frequency |
| Minor | Temporary pain increase, insomnia, facial flushing | Common |
| Moderate | Infection, nerve damage, allergic reactions | Less Common |
| Severe | Paralysis, severe allergic reactions, spinal cord injury | Rare |
Risks of Repeated Epidural Steroid Injections
Epidural steroid injections can help with pain, but they can also cause problems if used too much. It’s key to know the risks of using them over and over again.
Steroid-Related Systemic Effects
When you get these injections often, steroids can get into your blood. This can cause:
- Suppression of the hypothalamic-pituitary-adrenal axis, which might lead to adrenal insufficiency
- Hyperglycemia, which is bad for people with diabetes
- Osteoporosis and a higher chance of breaking bones
- Fluid retention and weight gain
These effects show why it’s important to choose patients carefully and keep an eye on them.
Local Tissue Changes
Using these injections a lot can also change the tissue around them. This can include:
- Tissue atrophy at the injection site
- Adhesions or scar tissue formation
- Nerve damage or neuropathy
Diminishing Returns and Tachyphylaxis
Using these injections too often can make them less effective. This is called tachyphylaxis. You might need more or more frequent injections to feel the same relief.
| Injection Frequency | Effectiveness | Potential Risks |
| Initial Injections | Highly effective | Minimal risks |
| Repeated Injections | Diminishing effectiveness | Increased risk of systemic effects and local tissue changes |
Psychological Dependence on Injections
There’s also a risk of becoming too dependent on these injections. People might feel they can’t live without them, leading to anxiety or fear of stopping treatment.
We need to think about the good and bad of these injections. Looking for other treatments can help avoid these problems.
Minimum Waiting Periods
Guidelines suggest a minimum wait time between injections. This wait is usually one to three weeks. It lets the first injection work and checks how the patient reacts before the next one.
A study in the Journal of Pain Research found waiting at least two weeks helps avoid complications. “
Optimal Spacing for Effectiveness
The best spacing between injections varies by patient and condition. Research shows four to six weeks apart can help with long-term pain from spinal issues.
- For sudden pain, injections every 1-2 weeks might be needed.
- For ongoing pain, spacing every 4-6 weeks is better for keeping pain under control.
Recovery Time Considerations
How long it takes to recover after an injection is important. Patients should avoid hard activities for 24 to 48 hours after. This helps the body heal and lowers the chance of problems.
Healthcare providers can make treatment better and safer by planning injection timing well. It’s important to adjust the schedule for each patient and watch how they do. This ensures safe and effective pain relief.
Special Considerations for Different Patient Populations
Administering epidural steroid injections requires careful thought for different patient groups. Some patients have health conditions, age, or other factors that affect treatment safety and success. We must tailor our approach to meet each patient’s needs. This ensures the best results and reduces risks.
Elderly Patients
Elderly patients often have many health issues. They might be more likely to experience side effects from epidural steroid injections. We must check their overall health, including conditions like osteoporosis or diabetes, before treatment.
We also need to adjust the dosage and how often to give injections. This is because their health might be more fragile.
Patients with Diabetes
Diabetes patients might see their blood sugar levels change with epidural steroid injections. We should watch their blood sugar closely before and after the procedure.
Also, we should talk to their primary care doctor or endocrinologist. This ensures the treatment fits with their diabetes care plan.
Immunocompromised Individuals
Patients with weakened immune systems face a higher risk of infections from epidural steroid injections. We must use strict sterile techniques and screen patients carefully.
We also need to think about the treatment’s benefits and risks for these patients.
Patients with Osteoporosis
Patients with osteoporosis are at a higher risk of bone fractures from epidural steroid injections. We should use imaging studies to check bone density before treatment.
We might also need to adjust the injection technique and the type of steroid used. This helps reduce the risk of complications for these patients.
Monitoring Patients Receiving Multiple Epidural Injections
When patients get multiple epidural steroid injections, we need to watch them closely. This is to keep them safe and make sure the treatment works. We use a few different ways to do this.
Clinical Assessment Methods
Checking in with patients is key when they get these injections. We see them regularly to check how they’re doing and if there are any side effects. We also change their treatment plan if needed.
We use special tools to measure their pain and check their nerves. This helps us see if the treatment is working. We also look at their overall health, including their medical history and what medicines they take.
Laboratory Monitoring
We do blood tests to see how the injections affect the body. For people with diabetes, we watch their blood sugar levels closely. We also check their cortisol levels to see if their adrenal glands are working right.
Other tests might include a complete blood count (CBC) and liver function tests. These help us catch any problems early. This way, we can act fast if something goes wrong.
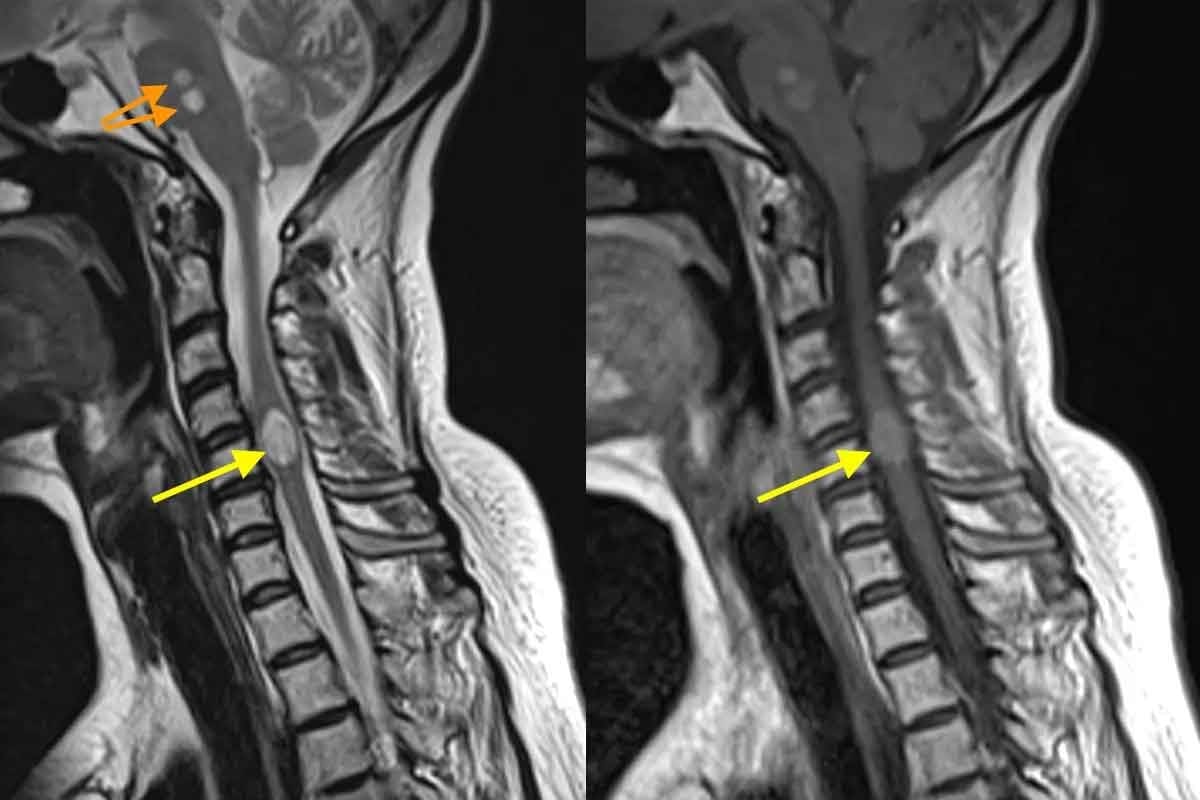
Imaging Follow-up
We also use X-rays, MRI, or CT scans to check the spine. This helps us see if there are any problems with the spine itself. For example, we might look for fractures or disc problems.
By using clinical checks, blood tests, and imaging, we can keep a close eye on patients. This makes sure the benefits of the injections are worth the risks. Here’s a quick summary of how we monitor:
| Monitoring Component | Description | Frequency |
| Clinical Assessment | Regular check-ups to evaluate treatment response and side effects | Every 1-3 months |
| Laboratory Tests | Blood glucose, cortisol levels, CBC, liver function tests | As needed, based on patient condition |
| Imaging Studies | X-rays, MRI, CT scans to assess spinal integrity | Baseline and as needed |
Alternative Treatments to Consider
Exploring options beyond epidural steroid injections is key for managing spinal conditions long-term. Many strategies can help manage pain and improve life quality.
Non-Steroid Injections
Looking for steroid injection alternatives? Non-steroid injections are a good choice. They include:
- Platelet-rich plasma (PRP) injections: Using your own platelets to heal.
- Hyaluronic acid injections: Adds lubrication and cushioning to joints.
- Nerve blocks: Blocks pain signals with local anesthetics or other meds.
“Non-steroid injections are gaining popularity. They offer a lasting pain management solution without steroids’ side effects.”
Physical Therapy Approaches
Physical therapy is vital for spinal conditions. It’s a non-invasive way to ease pain and improve function. Techniques include:
- Manual therapy: Hands-on methods to enhance joint mobility and reduce pain.
- Exercise programs: Custom exercises to build muscle and boost flexibility.
- Modalities: Heat, cold, or electrical stimulation to help recovery.
| Therapy Type | Benefits | Duration |
| Manual Therapy | Improved joint mobility, pain reduction | 30 minutes |
| Exercise Programs | Strengthened muscles, improved flexibility | Varied |
| Modalities | Aids in recovery, pain relief | 15-30 minutes |
Minimally Invasive Procedures
Some patients find relief in minimally invasive procedures. These include:
- Radiofrequency ablation: Uses heat to disable pain nerves.
- Spinal cord stimulation: Implants a device to send impulses to the spinal cord.
- Intradiscal therapies: Targets the intervertebral discs.
These options are considered when other treatments fail to provide relief.
Surgical Options
Surgery is a last resort but can be effective for some spinal conditions. Surgical options include:
- Discectomy: Removes a herniated disc.
- Spinal fusion: Fuses vertebrae for spine stability.
- Laminectomy: Removes part of the vertebra to relieve pressure.
Considering the benefits and risks of these alternatives shows a multi-faceted approach is often best.
Decision-Making Process for Repeated Injections
Deciding on repeated epidural steroid injections needs careful thought. We must look at the benefits and risks. It’s important to check how well past injections worked and talk about the next steps with the patient.
Evaluating Treatment Effectiveness
To see if more injections are needed, we look at past results. This means:
- Checking how much pain relief the patient got
- Seeing if their ability to function has improved
- Looking at any betterments in their quality of life
If past injections helped a lot, more might be considered. But if they didn’t help much or didn’t last, other options might be better.
Risk-Benefit Analysis
When thinking about more injections, weighing risks and benefits is key. We consider:
- The chance of more side effects with more injections
- The possibility of getting less help from each treatment
- The effects of steroids on the patient’s health
By looking at these points, we can decide if the benefits of more injections are worth the risks.
Patient-Doctor Shared Decision Making
Good decision-making comes from working together. We talk with patients to:
- Set treatment goals and what they hope to achieve
- Share the good and bad of more injections
- Look at other treatment choices
This way, we create a plan that fits the patient’s needs and wants.
Real-World Epidural Steroid Limits in Clinical Practice
Studies show that how often and how many epidural steroid injections patients get can really vary. This depends on the patient’s health, the condition being treated, and the doctor’s judgment.
Survey of Pain Management Specialists
A survey of pain management doctors shows different views on epidural steroid injections. Doctors consider how well a patient has responded to past injections, their overall health, and any other health issues when deciding on treatment.
We looked at how doctors practice and found:
- Most doctors follow guidelines but adjust them for each patient.
- Doctors tend to be more careful with patients who have other health problems.
- Using imaging and checking how the patient is doing is key in making decisions.
Common Clinical Approaches
Doctors often mix following guidelines with making treatment plans that fit each patient. They start with a careful approach and then adjust based on how the patient is doing.
| Clinical Approach | Description | Frequency of Use |
| Conservative | Start with fewer injections and adjust based on how the patient responds. | High |
| Guideline-Based | Follow official guidelines but also consider each case individually. | Moderate |
| Personalized | Make treatment plans that fit each patient’s specific needs and conditions. | High |
Case Studies and Examples
Many case studies show how epidural steroid injections are used in real life. For example, a patient with chronic back pain might get several injections. How many they get depends on how they respond and how the doctor assesses them.
We found that good results often come from choosing the right patient, using the right technique, and keeping a close eye on the patient.
Looking at real-world practices and case studies helps us understand how to use epidural steroid injections safely and effectively. This knowledge helps doctors make better decisions and improve patient care.
Conclusion
When we talk about epidural steroid injections, it’s all about finding a balance. We need to make sure we’re getting pain relief without risking our health. The rules for using these injections safely depend on many things. These include the patient’s health, any medical conditions they have, and how well they’ve responded to the injections before. We’ve looked at how these injections work and the risks of using them too much. Healthcare providers play a big role in making sure patients get the pain relief they need. They follow guidelines to keep risks low. This way, patients can get the most out of these injections while staying safe. It’s all about looking at each patient as an individual. By doing this, we can make sure they get the best results from their injections. And we keep their safety in mind at the same time.
FAQ
What are epidural steroid injections used for?
Epidural steroid injections help manage spinal pain. This includes pain from spinal stenosis, herniated discs, and sciatica.
How do epidural steroid injections work?
These injections deliver corticosteroids to the epidural space. This space is around the spinal cord. It reduces inflammation and relieves pain.
What are the common side effects of epidural steroid injections?
Side effects can be minor or severe. Minor ones include pain at the injection site and headaches. Severe reactions include infections and nerve damage.
How many epidural steroid injections can be safely administered in a lifetime?
The number of safe injections varies. It depends on health, response to treatment, and the condition being treated. Guidelines suggest 3-4 injections a year, up to 6-8 in a lifetime.
What are the risks associated with repeated epidural steroid injections?
Risks include systemic effects and local tissue changes. They can also lead to diminishing returns and psychological dependence. Long-term side effects include osteoporosis and adrenal suppression.
How often can epidural steroid injections be administered?
Injection frequency varies. It depends on the condition’s severity and treatment response. Injections are usually 1-3 weeks apart, with a minimum 1-2 week wait.
Are there alternative treatments to epidural steroid injections?
Yes, alternatives include non-steroid injections and physical therapy. Minimally invasive procedures and surgery are also options. These depend on individual needs and condition severity.
What factors affect the safe limits of epidural steroid injections?
Safe limits depend on age, health, and medical conditions. Previous injection response and injection location also play a role. These factors guide safe injection frequency and number.
How are patients receiving multiple epidural injections monitored?
Patients are monitored through clinical assessments and lab tests. Imaging follow-up also ensures safe treatment and detects complications or side effects.
Can epidural steroid injections be used for chronic pain management?
Yes, they can manage chronic pain. But, careful planning and monitoring are essential to minimize risks and ensure safe treatment.
What are the guidelines for epidural steroid injections recommended by medical organizations?
Guidelines vary but generally limit injections and space them out. The FDA and other organizations provide recommendations on safe usage limits.
Are there special considerations for different patient populations?
Yes, elderly patients, those with diabetes, immunocompromised individuals, and patients with osteoporosis need special care. These conditions may affect injection safety and efficacy.
References
- Cohen, S. P., et al. (2021). Safety of epidural steroid injections for lumbosacral radicular pain: An FDA advisory committee report review. Pain Medicine, 22(10), 2253-2256. https://pmc.ncbi.nlm.nih.gov/articles/PMC8360670/