Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that nearly 20% of patients who undergo a laminectomy may experience some form of failed back surgery syndrome? This is a condition where the surgery doesn’t alleviate the original symptoms.
Choosing to have a laminectomy is a big decision. It’s important to know the possible outcomes, including post laminectomy syndrome. If the surgery doesn’t work, it’s key to look into the next steps and possible laminectomy complications.
We know the challenges you’re facing and are here to help. In this article, we’ll look at the issues that might come up after a laminectomy. We’ll also guide you on what to do next.
Learn the crucial next steps if a laminectomy doesn’t work or if laminectomy complications occur. Understand further surgical or non-surgical options clearly.
Key Takeaways
- Understanding the risks and possible complications of laminectomy surgery.
- Recognizing the signs of failed back surgery syndrome.
- Exploring alternative treatments for post laminectomy syndrome.
- The importance of follow-up care after laminectomy.
- Support options available for patients experiencing laminectomy complications.
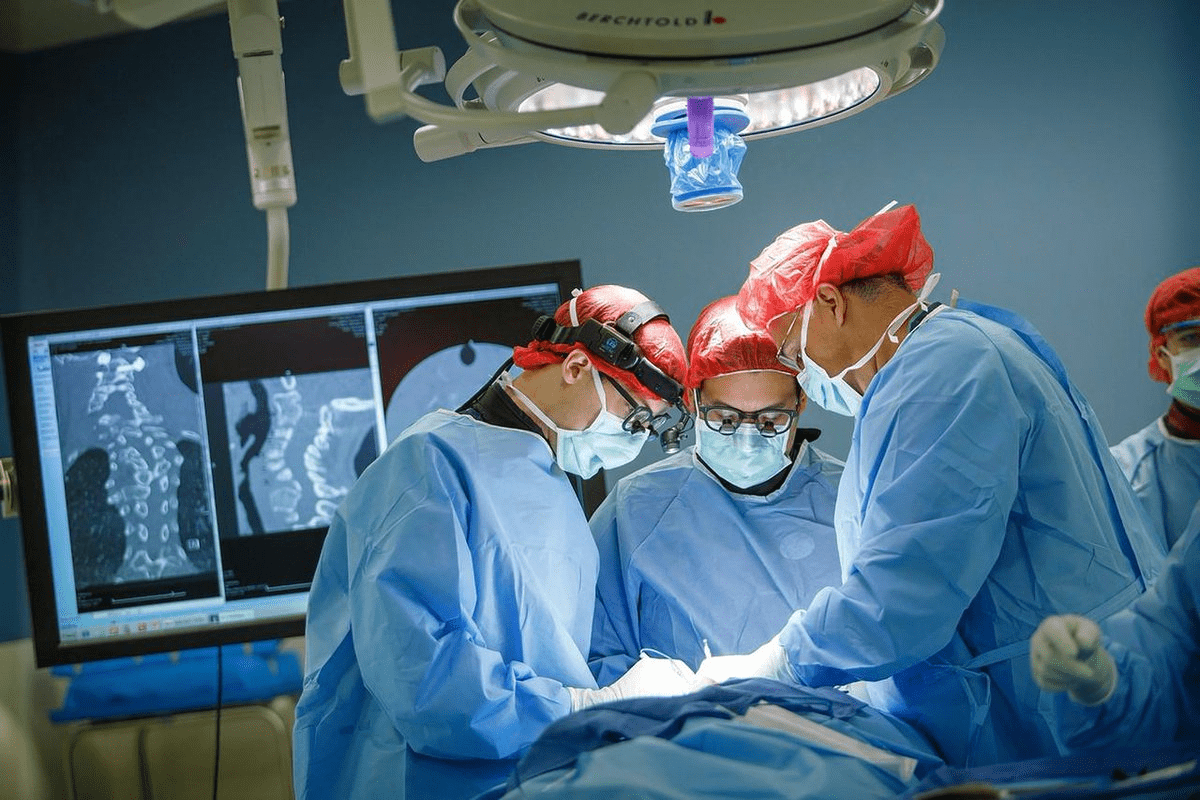
The Basics of Laminectomy Surgery
For those facing laminectomy surgery, knowing the basics is key. This surgery aims to ease pressure on the spinal cord or nerves. It’s often needed for conditions like spinal stenosis or herniated discs.
Definition and Purpose of Laminectomy
Laminectomy removes part of the vertebra called the lamina. Its main goal is to give nerves more space. This helps to reduce pain, numbness, and weakness.
By understanding laminectomy, patients can see its importance in treating spinal issues.
“The goal of laminectomy is to decompress the spinal canal and relieve pressure on the spinal cord or nerves, improving symptoms and quality of life.”
Types of Laminectomy Procedures
There are various laminectomy procedures, like cervical and lumbar laminectomies. Cervical laminectomy targets the neck, while lumbar laminectomy focuses on the lower back. Each type is chosen based on the spinal condition’s location and nature.
| Type of Laminectomy | Region of the Spine | Common Indications |
| Cervical Laminectomy | Neck Region (Cervical Spine) | Spinal stenosis, herniated discs |
| Lumbar Laminectomy | Lower Back (Lumbar Spine) | Spinal stenosis, degenerative disc disease |
Expected Recovery Timeline
The recovery time for laminectomy surgery varies. Patients usually stay in the hospital for a few days. Full recovery can take weeks to months, with physical therapy being key.
Knowing the recovery timeline helps patients prepare for the post-surgery period. It ensures a smoother recovery.
Signs Your Laminectomy Was Unsuccessful
It’s important for patients to know when a laminectomy might not have worked. This surgery aims to ease pressure on the spinal cord or nerves. If your symptoms don’t get better or even get worse after surgery, it could mean the procedure didn’t succeed.
Persistent or Worsening Pain
If your pain doesn’t get better or gets worse after laminectomy surgery, it might be a sign of failure. Persistent pain can be back pain, leg pain, or both. It depends on the original condition and the surgery details.
It’s key to tell if your pain is normal after surgery or if it’s a sign of a problem. If you’re in pain and it’s not getting better, talk to your doctor. They can help figure out if the surgery was successful.
- Pain that lasts longer than expected
- Pain that’s severe and affects daily life
- Pain that gets worse over time
Mobility Limitations After Recovery Period
Some mobility issues are normal right after a laminectomy. But if you’re having trouble walking, standing, or doing daily tasks without pain, it might be a sign of a problem. This could mean the surgery didn’t work as planned.
If your mobility hasn’t improved or has gotten worse, talk to your doctor. They can check if the surgery is the cause or if there’s something else going on.
Neurological Symptoms That Don’t Improve
Laminectomy surgery aims to ease nerve pressure. This should help with symptoms like numbness, tingling, or weakness in the legs. If these symptoms persist or worsen after surgery, it might mean the surgery didn’t fully work.
Neurological symptoms that don’t get better or get worse need quick medical attention. If you’re experiencing:
- Persistent numbness or tingling
- Increasing weakness in the legs
- Changes in bowel or bladder function
Talking to your healthcare provider about these signs is important. They can help figure out what to do next. This could include more tests, surgery, or other treatments. Finding out why your symptoms are not improving is the first step to getting better.
Understanding Laminectomy Complications
It’s important for patients to know about the possible complications of laminectomy. This surgery is usually safe, but problems can happen. These issues can affect how well you recover. We’ll look at the different complications, like immediate problems, infections, and spinal instability.
Immediate Post-Surgical Complications
Right after surgery, you might face bleeding, infection, or issues with anesthesia. These are rare but serious and need quick medical help.
Infection and Wound Healing Issues
Infection is a risk after laminectomy. Look out for redness, swelling, more pain, and fever. Taking good care of your wound and seeing your doctor can help avoid this.
Spinal Instability After Lamina Removal
Removing part or all of the lamina can cause spinal instability. This can put more stress on your spine, leading to more problems.
To understand laminectomy complications better, let’s look at a summary of risks and what they mean:
| Complication | Description | Potential Impact |
| Immediate Post-Surgical Complications | Bleeding, infection, reaction to anesthesia | Serious health risks requiring immediate medical attention |
| Infection and Wound Healing Issues | Signs include redness, swelling, increased pain, fever | Delayed recovery, possible more problems |
| Spinal Instability | Removing lamina can cause instability | More stress on the spine, might need more surgery |
Knowing how laminectomy changes your body can help you understand the risks better.
In conclusion, laminectomy is a good option for many, but knowing the risks is key. By understanding these risks and working with your doctor, you can reduce them. This way, you can get the best results from your surgery.
Post-Laminectomy Syndrome: Causes and Diagnosis
When laminectomy surgery doesn’t work as hoped, patients might get post-laminectomy syndrome. This condition is also known as failed back surgery syndrome. It includes a mix of symptoms that don’t go away after surgery.
Clinical Definition and ICD-10 Classification
Post-laminectomy syndrome is when pain or discomfort lasts after surgery. The ICD-10 code for it is M96.1. This code helps doctors worldwide to track and treat the condition.
“The diagnosis of post-laminectomy syndrome needs a full check of symptoms and medical history,” says recent guidelines. Knowing the definition and ICD-10 code is key for the right treatment.
Risk Factors for Developing Failed Back Syndrome
Several things can lead to post-laminectomy syndrome. These include:
- Conditions like degenerative disc disease or spinal instability
- Bad surgery technique or not enough decompression
- Complications after surgery like infection or healing problems
- Factors like smoking, being overweight, or not being in good shape
Knowing these risk factors helps doctors figure out the chance of post-laminectomy syndrome. They can then plan the best treatment.
Diagnostic Criteria and Evaluation
To diagnose post-laminectomy syndrome, doctors look at symptoms, medical history, and imaging. They use:
- Looking at the patient’s history and symptoms
- Scans like MRI or CT to see the spine
- Tests like electromyography to check nerves
A detailed check is important. It helps find the cause of pain and plan the best treatment for post-laminectomy syndrome.
Nerve Damage After Spinal Surgery
Spinal surgery can sometimes lead to nerve damage. This can greatly affect a patient’s recovery and life quality. It’s important to know about the different nerve injuries, their signs, and how to tell if damage is temporary or permanent.
Types of Nerve Injuries
Nerve damage from laminectomy can take several forms. Neuropraxia is the least severe, causing temporary nerve block without harm to the nerve itself. Axonotmesis damages the nerve’s axon but keeps the surrounding tissue intact, leading to a longer recovery. Neurotmesis is the worst, where the nerve is completely cut, often causing permanent harm.
Symptoms of Post-Surgical Nerve Damage
The signs of nerve damage after surgery vary. They can include numbness, tingling, weakness, and pain in certain areas. Some people might also feel radicular pain, which spreads along the nerve’s path.
Differentiating Between Temporary and Permanent Damage
Telling temporary from permanent nerve damage is key for treatment. Temporary damage might heal in weeks or months, while permanent damage needs more serious care. Tests like electromyography (EMG) and nerve conduction studies (NCS) help figure out the damage’s extent and future.
Dealing with nerve damage after spinal surgery is tough. Knowing about the different injuries and their signs helps doctors give better care and support to patients.
Comprehensive Diagnostic Evaluation
Understanding why pain or neurological symptoms last after a laminectomy is key. We use many tools and techniques to find the cause. This helps us understand what’s happening.
Advanced Imaging Techniques
Imaging is very important in finding the cause of symptoms. We use MRI, CT scans, and X-rays to see the spine. This helps us spot any problems.
- MRI (Magnetic Resonance Imaging): Shows soft tissues like nerves and discs in detail.
- CT (Computed Tomography) scans: Gives clear images of bones and can find bone spurs or spinal stenosis.
- X-rays: Helps check spinal alignment and find fractures or bone issues.
Electromyography and Nerve Conduction Studies
We also check nerve function with electromyography (EMG) and nerve conduction studies (NCS). These tests look at muscle and nerve activity. They help us see if nerves are damaged.
- Electromyography (EMG): Checks muscle electrical activity to find damage or nerve problems.
- Nerve Conduction Studies (NCS): Tests how fast and strong nerve signals are, helping find nerve damage or compression.
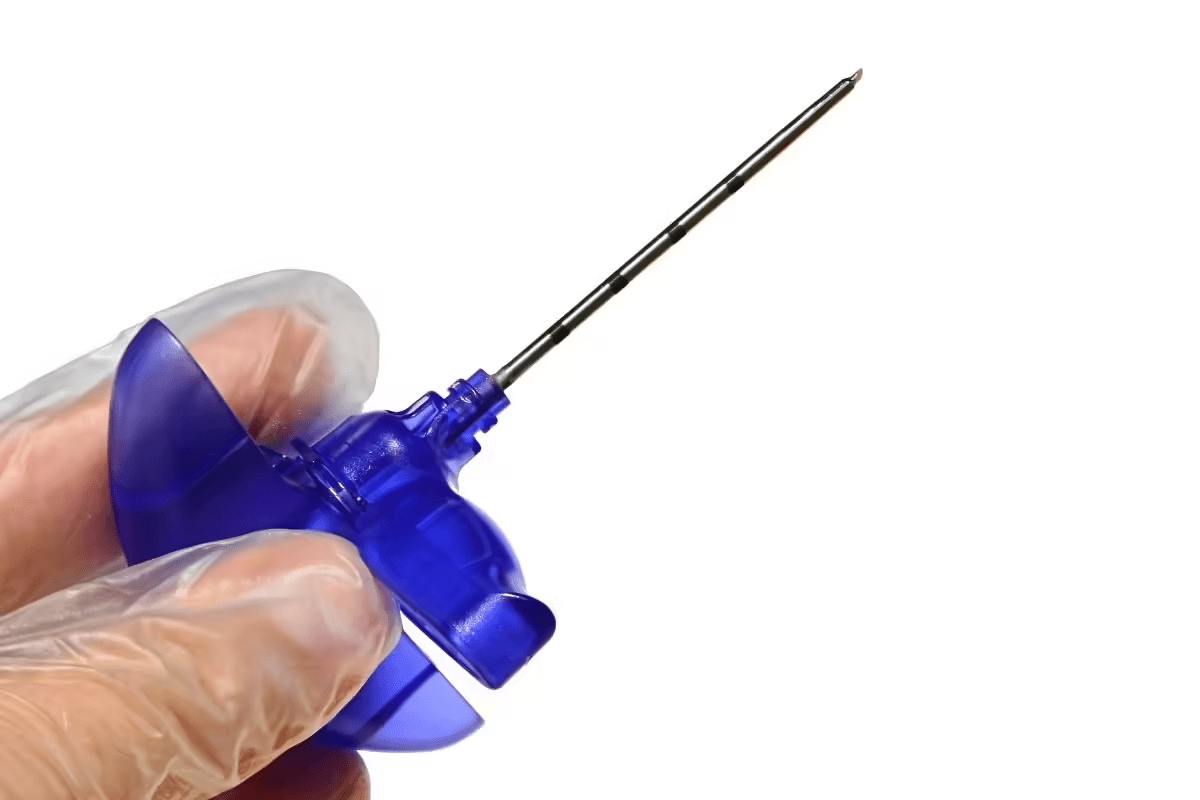
Diagnostic Nerve Blocks
Diagnostic nerve blocks are used to find specific nerves causing pain. We inject a local anesthetic around the nerve to see if it helps.
By using all these methods, we can fully understand why symptoms last after a laminectomy. Then, we can create a treatment plan that works for each person.
Non-Surgical Pain Management Strategies
Non-surgical methods are key in helping patients manage pain after laminectomy surgery. Effective pain management is vital for recovery and improving life quality. We will look at non-surgical ways to manage pain, including prescription drugs, over-the-counter options, and topical treatments.
Prescription Medications for Post-Surgical Pain
Prescription drugs are often needed for severe pain after laminectomy surgery. Opioids are strong pain relievers but are used for short-term pain due to dependency risks. Other options include muscle relaxants and gabapentinoids for muscle spasms and neuropathic pain, respectively.
It’s important for patients to work with their healthcare provider to find the right medication and dosage. They should also watch for any side effects.
Over-the-Counter Options and Supplements
For those not wanting prescription drugs, over-the-counter (OTC) options are a good alternative. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can reduce inflammation and pain. Acetaminophen can also manage pain, but it’s important to follow the dosage to avoid liver damage.
Certain supplements, such as glucosamine and chondroitin, may help some patients. But, it’s important to talk to a healthcare provider before adding supplements to your routine.
Topical Treatments and Patches
Topical treatments are another way to manage pain. Topical NSAIDs in creams, gels, or patches can be applied directly to the painful area for localized relief. Lidocaine patches numb the skin to reduce pain perception.
These treatments are great for patients who can’t take oral medications or prefer a targeted approach to pain management.
Physical Therapy and Rehabilitation Approaches
Physical therapy is key in helping patients get back their strength and mobility after laminectomy surgery. A good rehabilitation plan is vital for the best recovery and to avoid complications.
Core Strengthening Exercises
Core strengthening is a big part of recovery after laminectomy. Exercises for the abdominal and back muscles help keep the spine stable. This reduces the chance of future injuries and eases pain. Some examples are:
- Planks
- Bridges
- Pelvic tilts
Start these exercises slowly, with a physical therapist’s help. This ensures you do them right and don’t push too hard.
Flexibility and Mobility Programs
Along with core strengthening, exercises for flexibility and mobility are also important. They help keep the range of motion and prevent stiffness. Some methods include:
- Gentle stretching
- Yoga
- Pilates
These programs help patients get back to their daily activities and improve their life quality.
Aquatic Therapy and Low-Impact Options
Aquatic therapy is a gentle way for patients to recover. Water-based exercises are easy on the spine but help build strength and flexibility. Other low-impact choices are:
- Cycling
- Elliptical trainer
- Low-impact aerobics
These activities can be adjusted to fit each patient’s needs and likes, making sure they get a full recovery plan.
Interventional Pain Management Procedures
When laminectomy doesn’t work, interventional pain management can help. These methods aim to find and treat pain that lasts after surgery. They offer many effective ways to manage pain.
Epidural Steroid Injections
Epidural steroid injections are a common method to reduce inflammation and pain. Steroids are injected into the space around the spinal cord. This can help lessen swelling and irritation that cause pain.
“Epidural steroid injections have been shown to provide significant pain relief for many patients,” says a leading pain management specialist.
The procedure is done under fluoroscopic guidance for accurate placement. While generally safe, patients might feel some temporary side effects like increased pain or numbness.
Facet Joint Injections and Medial Branch Blocks
Facet joint injections and medial branch blocks target pain from the facet joints. These small joints are between and behind vertebrae. When inflamed or irritated, they can cause a lot of pain.
Facet joint injections involve injecting a local anesthetic, and sometimes a steroid, into the joint. Medial branch blocks target the nerves that supply the facet joints. These procedures help diagnose and treat pain. A study in the Journal of Pain Research found that facet joint injections can significantly reduce pain in patients with facet joint syndrome.
Radiofrequency Ablation Techniques
Radiofrequency ablation (RFA) uses heat from radiofrequency waves to target and ablate specific nerves. It’s useful for chronic pain that hasn’t responded to other treatments.
The procedure uses fluoroscopy to guide a needle electrode to the targeted nerve. The electrode then emits radiofrequency energy, heating the nerve and disrupting its pain signals. RFA can offer long-term pain relief, though it may need to be repeated as the effects can wear off over time.
The American Society of Interventional Pain Physicians notes, “radiofrequency ablation has become an increasingly popular treatment option for chronic pain management, providing a minimally invasive alternative to surgery.”
Advanced Neuromodulation Options
Neuromodulation therapies are a new hope for those with ongoing pain after laminectomy surgery. These treatments aim to change how the nervous system sends pain signals. This can help when other methods don’t work.
Spinal Cord Stimulation Systems
Spinal cord stimulation (SCS) systems are a type of neuromodulation therapy. They involve putting a device that sends electrical impulses to the spinal cord. These impulses can block or change pain signals to the brain, giving relief to some patients.
Key Features of SCS Systems:
- Implantable pulse generator
- Lead placement near the spinal cord
- Programmable stimulation parameters
A study in the Journal of Neurosurgery: Spine showed SCS helps a lot with pain for those with failed back surgery syndrome. This is a common problem after unsuccessful laminectomy.
Dorsal Root Ganglion Stimulation
Dorsal root ganglion (DRG) stimulation targets specific pain pathways. It aims to give precise pain relief, mainly for those with complex regional pain syndrome or other specific pain issues.
| Therapy | Target Area | Primary Benefit |
| SCS | Spinal Cord | Broad pain coverage |
| DRG Stimulation | Dorsal Root Ganglion | Targeted pain relief |
Intrathecal Drug Delivery Pumps
Intrathecal drug delivery uses a pump to send medication into the spinal fluid. It offers targeted pain management with possibly less medication than oral forms.
“Intrathecal therapy has revolutionized the management of chronic pain, providing a powerful tool for those who haven’t found relief with other treatments.” – A Pain Management Specialist
These advanced neuromodulation options are a big step forward in pain management for those who had laminectomy surgery but didn’t get enough relief. Knowing about these options helps both patients and doctors choose the best treatment.
Considering Revision Surgery
Revision surgery might help if you’re not feeling better after a laminectomy. If the first surgery didn’t work, you and your doctor need to think about what to do next.
Deciding on another surgery is tough. But for some, it could really help and make life better.
Patient Selection Criteria
To see if you’re right for revision surgery, doctors look at a few things. They check why you’re not feeling better, your health, and the area of your spine involved.
- Presence of recurrent disc herniation or spinal stenosis
- Incomplete resolution of the initial condition
- Development of new spinal instability
- Presence of scar tissue or adhesions
Doctors use tests and scans to figure out if you’re a good candidate for surgery.
Types of Corrective Procedures
Revision surgery can include different procedures, based on what the tests show.
| Procedure | Description | Indications |
| Revision Discectomy | Removal of recurrent disc herniation | Recurrent disc herniation causing symptoms |
| Spinal Fusion | Stabilization of the spine through fusion | Spinal instability or deformity |
| Revision Laminectomy | Further decompression of neural elements | Incomplete initial decompression or new stenosis |
Success Rates and Recovery Expectations
How well revision surgery works depends on the problem and your health. For the right patients, it can really help.
How long it takes to get better varies. It depends on the surgery and your health. A good rehab plan is key for the best results.
We help our patients make a recovery plan that’s just for them. This way, they get the best results from surgery.
Alternative and Complementary Therapies
There are many options for managing pain and improving well-being after laminectomy surgery. These include alternative and complementary therapies. They can work alongside traditional treatments for a more complete care plan.
Acupuncture and Traditional Chinese Medicine
Acupuncture is a part of traditional Chinese medicine. It involves putting fine needles into certain body points to help heal and relieve pain. Studies show it can reduce chronic pain and improve function in spinal surgery patients.
Benefits of Acupuncture: It can lessen pain and swelling, boost mood, and improve overall health.
Massage and Manual Therapies
Massage and manual therapies can ease muscle tension, improve blood flow, and relax the body. They are great for those with chronic pain or stiffness after laminectomy surgery.
- Types of massage therapy: Swedish massage, deep tissue massage, and myofascial release.
- Benefits: Reduced muscle tension, better range of motion, and more relaxation.
Mind-Body Approaches for Pain Management
Mind-body therapies like meditation, yoga, and cognitive-behavioral therapy help manage chronic pain. They focus on the psychological and emotional sides of pain.
Mind-body benefits: Less stress, better mood, and better ways to cope with pain.
Adding alternative and complementary therapies to a care plan can help individuals manage pain better. It can also improve their quality of life after laminectomy surgery.
Psychological Support for Chronic Pain
Managing chronic pain after a laminectomy is more than just medical treatment. It needs a full approach that includes psychological support. Chronic pain can really affect a person’s life, not just their body but their mind too. It’s key to tackle the mental side of chronic pain to offer complete care.
Cognitive Behavioral Therapy for Pain Management
Cognitive Behavioral Therapy (CBT) is a big help in managing chronic pain. It helps people see pain differently and find ways to deal with it. CBT is not about getting rid of pain completely but about learning to handle it well, which can greatly improve life quality.
“CBT gives patients the tools to manage their pain,” says Medical Expert, a pain management expert. “It’s about realizing we can’t always control pain, but we can control how we react to it.”
Addressing Depression and Anxiety
Chronic pain often comes with depression and anxiety. It’s very important to tackle these mental health issues to manage pain well. Therapy, including medication and counseling, can really help people cope with chronic pain.
A study in the Journal of Pain Research showed that treating depression and anxiety in people with chronic pain greatly reduced their pain.
Support Groups and Community Resources
Support groups are very important for people with chronic pain. They offer a sense of community and understanding. Sharing experiences and strategies with others facing similar issues can be very empowering.
- Connecting with others who understand the challenges of chronic pain
- Learning new coping strategies and techniques
- Finding emotional support and reducing feelings of isolation
Lifestyle Modifications for Long-Term Management
Success after laminectomy surgery depends on lifestyle choices. By changing daily habits, people can live better and manage pain. Making smart choices about daily life can greatly improve well-being.
Ergonomic Considerations for Daily Activities
Making ergonomic changes in daily life can ease back pain. Keeping good posture and using supportive furniture helps. Taking breaks to stretch also helps.
Adjusting computer monitor heights and using ergonomic keyboards can help a lot. For those who sit a lot, using chairs with lumbar support is key. When lifting, bend at the knees to avoid back strain.
Weight Management and Nutrition
Keeping a healthy weight is important for spine health and pain management. Eating a balanced diet supports recovery. Include fruits, veggies, whole grains, and lean proteins in your meals.
Drinking plenty of water is also important for spinal health. Avoiding processed foods and sugary items helps too. Getting advice from a nutritionist can be very helpful.
Sleep Optimization Strategies
Good sleep is key for healing and pain control. A cool, dark, quiet bedroom helps sleep. A supportive mattress and proper pillows are also important.
Having a regular sleep schedule and avoiding bedtime activities helps. Relaxation techniques like deep breathing can also improve sleep.
Working With Your Healthcare Team
Building a strong healthcare team is key to tackling persistent pain after laminectomy. Working well with your healthcare providers can greatly improve your life and health outcomes.
Assembling a Multidisciplinary Pain Management Team
A team for pain management includes experts like pain specialists, physical therapists, and psychologists. They work together to create a treatment plan that fits your needs.
The benefits of this team are many:
- They give a full check-up of your condition
- They coordinate care from different fields
- You get to try many treatment options
| Team Member | Role |
| Pain Specialist | Creates and carries out pain management plans |
| Physical Therapist | Improves your mobility and strength |
| Psychologist | Offers support for dealing with chronic pain |
When to Seek Second Opinions
Getting a second opinion is very helpful if you’re not sure about your diagnosis or treatment. It’s important to ask for more advice if you’re not getting better.
Here are some times to get a second opinion:
- If your diagnosis is unclear or different
- If you’re not getting better with current treatment
- If you’re thinking about surgery or invasive treatments
Advocating for Your Care Needs
Being involved in your care is vital for the best results. This means talking openly with your healthcare team, asking questions, and sharing your worries.
Here are some tips for being a good patient advocate:
- Keep a record of your symptoms and treatments
- Ask about your diagnosis and treatment choices
- Look for support from patient advocacy groups
By working closely with your healthcare team and speaking up for yourself, you can better handle post-laminectomy pain.
Conclusion
Managing laminectomy complications well needs a detailed and varied plan. Knowing the possible issues and looking at different treatments helps patients handle pain better. This improves their life quality.
We talked about ways to manage pain after laminectomy. This includes non-surgical methods, physical therapy, and advanced treatments. It’s key to work with a healthcare team to find the right treatment.
Patients can help their recovery by working with a team of pain management experts. This team approach is vital for tackling complications and improving results. It shows how important a detailed plan is for better patient care.
FAQ
What is a laminectomy, and what is its purpose?
A laminectomy is a surgery that removes part of the vertebra called the lamina. It aims to relieve pressure on the spinal cord or nerves. This is done to ease pain, numbness, or weakness caused by nerve compression.
What are the signs that a laminectomy was unsuccessful?
Signs of a failed laminectomy include ongoing or worsening pain. You might also face mobility issues or unresolved neurological symptoms like numbness or weakness.
What are the possible complications of laminectomy surgery?
Complications from laminectomy surgery can include immediate issues, infections, and spinal instability. Nerve damage and post-laminectomy syndrome are also possible.
What is post-laminectomy syndrome, and how is it diagnosed?
Post-laminectomy syndrome is a condition with persistent pain after surgery. It’s diagnosed through clinical evaluation, medical history, and tests like imaging and nerve studies. The ICD-10 code for it is M96.1.
How is nerve damage after spinal surgery diagnosed and managed?
Nerve damage is diagnosed with clinical evaluation, electromyography, and nerve studies. Treatment includes non-surgical pain management, physical therapy, and interventional procedures.
What are the non-surgical pain management strategies for post-laminectomy pain?
Non-surgical strategies include prescription and over-the-counter medications, topical treatments, and alternative therapies like acupuncture and massage.
What is the role of physical therapy in laminectomy recovery?
Physical therapy is key in recovery by improving strength, flexibility, and mobility. It includes exercises, flexibility programs, and aquatic therapy.
What are interventional pain management procedures, and how are they used in post-laminectomy pain management?
Interventional procedures include injections and radiofrequency ablation to manage pain. They reduce inflammation and relieve nerve pressure.
What are advanced neuromodulation options for managing chronic pain after laminectomy surgery?
Advanced options include spinal cord stimulation and intrathecal drug delivery. These technologies deliver impulses or medications to manage chronic pain.
When is revision surgery considered after a laminectomy?
Revision surgery is considered for ongoing issues like pain, instability, or nerve compression. The decision is based on a thorough evaluation of the patient’s condition.
How can lifestyle modifications help manage pain and improve quality of life after laminectomy surgery?
Lifestyle changes like ergonomic considerations, weight management, and sleep optimization can help. They reduce spine strain, promote health, and improve sleep.
Why is it important to work with a multidisciplinary healthcare team in managing post-laminectomy pain?
Working with a multidisciplinary team is vital for managing pain. It offers a range of expertise and treatment options. This team includes pain specialists, physical therapists, and psychologists.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539777/[3