Last Updated on December 2, 2025 by Bilal Hasdemir

Bariatric surgery is a surgical procedure that aims to promote weight loss by altering the digestive system. The most common types include gastric sleeve, gastric bypass, and adjustable gastric banding. Each of these procedures has its own characteristics and potential benefits Least Painful Bariatric Surgery Options.
Understanding the differences between these procedures is crucial for patients considering bariatric surgery. Factors such as the complexity of the procedure, recovery time, and individual pain tolerance play significant roles in determining the overall experience.
Key Takeaways
- Common types of bariatric surgeries include gastric sleeve, gastric bypass, and adjustable gastric banding.
- The level of pain experienced can vary significantly between procedures.
- Individual factors such as pain tolerance and overall health influence the perception of pain.
- Understanding the characteristics of each procedure is essential for making an informed decision.
- Consulting with a healthcare professional is crucial for determining the best option.
Understanding Bariatric Surgery and Pain Considerations
When considering bariatric surgery, it’s essential to delve into the various procedures available and their implications on pain levels. Bariatric surgery encompasses a range of surgical procedures designed to aid in weight loss by altering the digestive system. The primary goal is to help individuals achieve significant weight loss when other methods have failed.
Types of Bariatric Procedures Available Today
There are several types of bariatric surgical procedures, each with its unique characteristics and potential for pain. The most common include:
- Gastric Sleeve Surgery: Involves removing a large portion of the stomach, leaving a narrow ‘sleeve’.
- Gastric Bypass Surgery: Creates a small pouch from the stomach and connects it directly to the small intestine.
- Adjustable Gastric Banding: Involves placing a band around the upper part of the stomach to create a small pouch.
Each of these procedures has different implications for pain and recovery. Understanding these differences is crucial for managing expectations.
How Pain is Measured in Surgical Procedures
Pain measurement in surgical procedures, including bariatric surgery, is inherently subjective. It varies significantly from one patient to another based on individual pain thresholds, the extent of the surgery, and psychological factors.
Several methods are used to measure pain, including:
- Visual Analog Scale (VAS): Patients rate their pain on a scale from 0 to 10.
- Numerical Rating Scale (NRS): Similar to VAS, but uses numbers to quantify pain.
- McGill Pain Questionnaire: Assesses the quality and intensity of pain.
These measurement tools help healthcare providers understand the level of pain a patient is experiencing and tailor pain management strategies accordingly.
Factors That Influence Pain Perception After Weight Loss Surgery
The experience of pain following bariatric surgery varies significantly among individuals due to several key factors. Understanding these factors is crucial for patients to have realistic expectations about their recovery process.
Individual Pain Thresholds and Sensitivity
Every individual has a unique pain threshold, which is influenced by a combination of genetic, environmental, and psychological factors. Research has shown that people with a higher pain tolerance tend to report less pain after surgery. Understanding one’s pain threshold can help in managing post-operative pain more effectively.
- Genetic predisposition to pain sensitivity
- Previous experiences with pain
- Psychological state, including anxiety and stress levels
Pre-existing Medical Conditions
Pre-existing medical conditions can significantly impact how an individual perceives pain after bariatric surgery. Conditions such as diabetes, fibromyalgia, and chronic pain syndrome can alter pain perception and may require specialized pain management strategies.
- Diabetes: Can lead to neuropathy, affecting pain perception
- Fibromyalgia: Characterized by widespread musculoskeletal pain
- Chronic pain syndrome: Ongoing pain that can complicate post-surgical pain management
Psychological Factors Affecting Pain Experience
Psychological factors, including anxiety, depression, and stress, play a significant role in how pain is experienced after surgery. Patients with a positive outlook and effective coping mechanisms tend to report lower levels of pain. Pre-operative counseling and post-operative support can be beneficial in managing these psychological factors.
- Anxiety and fear about the surgery and recovery
- Depression and its impact on pain perception
- Coping strategies and support systems
By understanding these factors, healthcare providers can offer more personalized care, potentially reducing the pain experienced by patients after bariatric surgery.
Least Painful Bariatric Surgery Options
Different bariatric procedures have distinct pain profiles that patients should be aware of before making a decision. Understanding these differences is crucial for managing expectations and making an informed choice.
How Different Procedures Compare on the Pain Scale
Bariatric surgeries vary in their invasiveness and technique, which directly impacts the level of pain experienced by patients. Minimally invasive procedures tend to result in less tissue damage and, consequently, less pain.
A comparative analysis of common bariatric procedures reveals that:
Procedure | Pain Level (Scale of 1-10) | Recovery Time |
Laparoscopic Adjustable Gastric Banding | 4-6 | 1-2 weeks |
Gastric Sleeve Surgery | 6-8 | 2-4 weeks |
Gastric Bypass Surgery | 7-9 | 3-6 weeks |
Short-term vs. Long-term Pain Considerations
Pain associated with bariatric surgery can be categorized into short-term and long-term. Short-term pain is typically managed with medication and subsides within a few weeks. Long-term pain, if experienced, is often related to complications or adjustments to the body’s new anatomy.
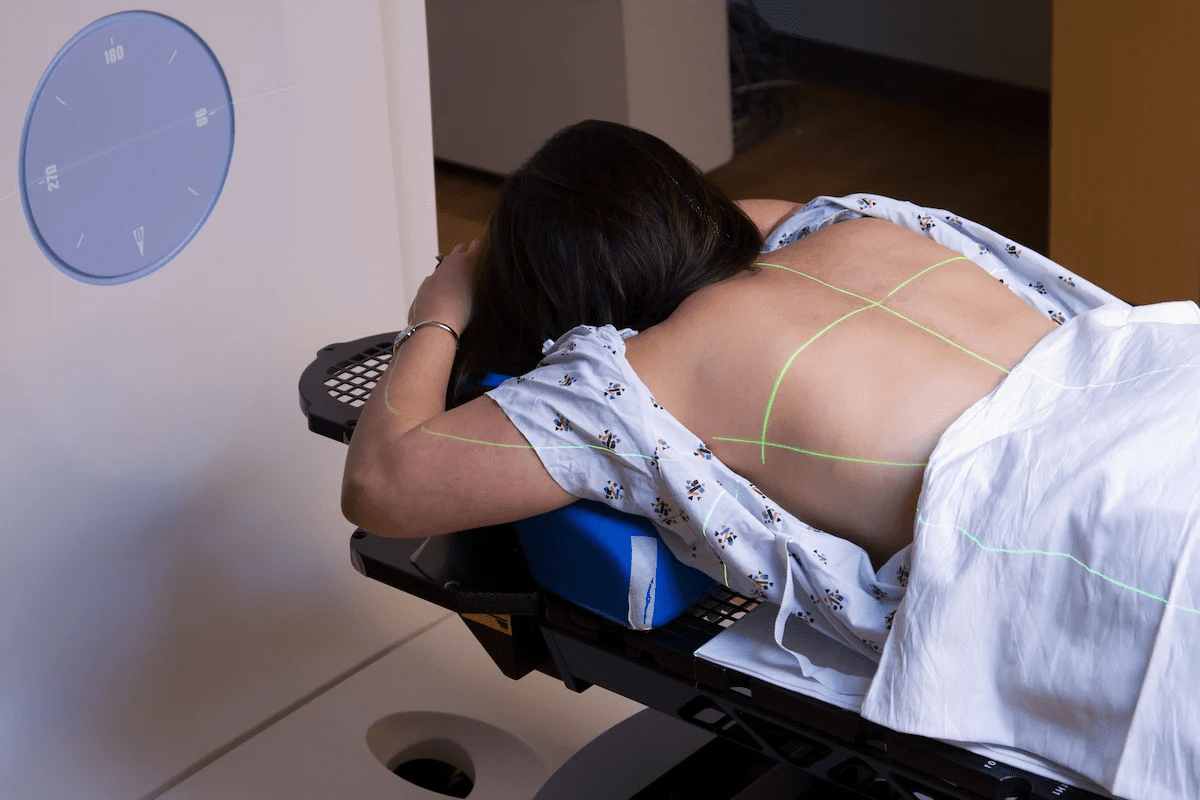
Minimally Invasive Approaches and Pain Reduction
Minimally invasive bariatric surgeries, such as laparoscopic procedures, have become increasingly popular due to their benefits in reducing pain and recovery time. These techniques involve smaller incisions, less tissue damage, and often result in fewer complications.
By choosing a minimally invasive approach, patients can potentially reduce their post-operative pain and return to normal activities more quickly.
Laparoscopic Adjustable Gastric Band (LAP-BAND): Pain Profile
The Laparoscopic Adjustable Gastric Band, commonly referred to as LAP-BAND, has gained attention for its potential to provide significant weight loss with relatively less discomfort. This procedure involves the placement of an adjustable band around the upper part of the stomach, creating a small pouch to restrict food intake.
Surgical Technique and Invasiveness
The LAP-BAND procedure is considered less invasive compared to other bariatric surgeries, such as gastric bypass or duodenal switch. It is performed laparoscopically, meaning it requires only small incisions through which surgical instruments and a camera are inserted. This minimally invasive approach contributes to less tissue damage and trauma, potentially reducing post-operative pain.
The surgical technique involves:
- Creating small incisions in the abdomen to insert laparoscopic instruments.
- Dissecting the area around the upper stomach to place the LAP-BAND.
- Adjusting the band to create a small stomach pouch.
- Securing the band in place.
Typical Pain Levels During Recovery
Pain levels during recovery from LAP-BAND surgery can vary among individuals. However, most patients report experiencing less pain compared to more invasive bariatric procedures. The pain is typically managed with over-the-counter or prescription pain medications.
Common pain experiences include:
- Mild to moderate discomfort at the incision sites.
- Soreness in the upper abdomen.
- Discomfort when swallowing or eating.
Patient Testimonials on LAP-BAND Pain Experience
Patient testimonials provide valuable insights into the real-world experience of undergoing LAP-BAND surgery. Many patients report that the pain was less than expected and manageable with medication.
“I was surprised by how little pain I experienced after the LAP-BAND surgery. The recovery was smoother than I anticipated.”
— A LAP-BAND patient
Overall, the LAP-BAND procedure is recognized for its potential to offer a relatively pain-free weight loss surgery experience, making it an attractive option for individuals considering bariatric surgery.
Gastric Sleeve Surgery: Pain Assessment
For many individuals struggling with obesity, gastric sleeve surgery offers a viable solution, but understanding its pain profile is crucial. Gastric sleeve surgery, also known as sleeve gastrectomy, involves the removal of a significant portion of the stomach, leaving a narrow “sleeve” or tube-like stomach.
Procedure Details and Impact on Pain
The gastric sleeve procedure is performed laparoscopically, meaning it involves several small incisions through which surgical instruments and a camera are inserted. This minimally invasive approach can reduce recovery time and potentially decrease the level of post-operative pain compared to open surgery. The removal of a large portion of the stomach can lead to discomfort due to the reduction in stomach size and the healing process of the staple lines.
Recovery Timeline and Pain Progression
The recovery timeline for gastric sleeve surgery typically involves a gradual decrease in pain over several weeks. Immediately following surgery, patients may experience discomfort due to the surgical incisions and the internal healing process. Pain management strategies, including medication, are usually employed to manage this initial discomfort. As patients progress in their recovery, typically within 2-4 weeks, the pain significantly subsides, allowing for a return to normal activities.
Real Patient Experiences with Gastric Sleeve Pain
Patient experiences with gastric sleeve surgery pain can vary significantly. Some patients report manageable pain levels throughout their recovery, while others may experience more severe discomfort, particularly in the first few days post-surgery. “I was surprised by how quickly my pain decreased after the first week,” shared one patient. Effective pain management and support from healthcare providers play a crucial role in minimizing discomfort and ensuring a smooth recovery.
Understanding the pain associated with gastric sleeve surgery is essential for setting realistic expectations and preparing for the recovery process. By considering the procedure details, recovery timeline, and real patient experiences, individuals can make informed decisions about their weight loss surgery options.
Gastric Bypass Surgery: Pain Expectations
Understanding the pain expectations associated with gastric bypass surgery is crucial for patients considering this weight loss option. Gastric bypass surgery, a complex procedure involving the rerouting of the digestive system, can result in significant pain during the initial recovery period.
Surgical Complexity and Pain
The complexity of gastric bypass surgery is a significant factor in the level of pain experienced during recovery. This procedure involves creating a small pouch from the stomach and connecting it directly to the small intestine, which can lead to discomfort and pain due to the invasive nature of the surgery.
The surgical complexity can be broken down into several key aspects that influence pain levels:
- The extent of the surgical incision and the technique used
- The amount of manipulation required to reroute the digestive system
- The overall duration of the surgery
Post-operative Pain Management
Effective post-operative pain management is critical for patients undergoing gastric bypass surgery. Various strategies are employed to manage pain, including:
Pain Management Approach | Description |
Medication | Use of pain relief medications to manage post-operative pain |
Non-pharmaceutical methods | Techniques such as breathing exercises, physical therapy, and relaxation techniques |
Patient Experiences with Gastric Bypass Recovery
Patient reports on their gastric bypass recovery experience vary, but many highlight the importance of a comprehensive pain management plan. Some common themes include:
“The first few days were the most painful, but with the help of my pain management team, I was able to recover relatively quickly.” –
Patient testimonial
By understanding the factors that influence pain and implementing effective pain management strategies, patients can better navigate their recovery from gastric bypass surgery.
Duodenal Switch: Understanding the Pain Profile
Duodenal switch surgery, known for its complexity, raises important questions about post-operative pain and recovery. This bariatric procedure involves both stomach reduction and intestinal rerouting, making it a significant undertaking for patients.
Procedure Complexity and Pain Correlation
The complexity of the duodenal switch procedure is a significant factor in determining the level of post-operative pain. The surgery involves a partial gastrectomy and an intestinal bypass, which can lead to a more challenging recovery compared to less invasive bariatric surgeries.
Recovery Experience and Pain Timeline
Patients undergoing duodenal switch surgery typically experience a varied recovery timeline, with pain levels fluctuating over the initial weeks. The immediate post-operative period is usually the most painful, with discomfort gradually subsiding as the patient heals.
- Pain is generally most intense in the first few days following surgery.
- Patients are often prescribed pain management medication to help cope with discomfort.
- The overall recovery experience can be influenced by the patient’s pre-operative health and adherence to post-operative instructions.
Long-term Pain Considerations
While the duodenal switch is associated with significant short-term pain, the long-term pain considerations are generally more favorable. Many patients report a reduction in pain over time as their body adapts to the changes made during surgery.
It’s essential for patients to discuss their individual pain profile and recovery expectations with their healthcare provider to ensure they are prepared for the challenges and benefits associated with duodenal switch surgery.
The Role of Anesthesia in Controlling Surgical Pain
Modern anesthesia techniques have revolutionized pain management in bariatric surgery. The administration of anesthesia is a critical component of the surgical process, directly influencing the patient’s pain experience both during and after the procedure.
Modern Anesthesia Techniques for Bariatric Surgery
Advances in anesthesia have led to the development of more effective and safer pain management strategies for bariatric surgery patients. Techniques such as total intravenous anesthesia (TIA) and the use of multimodal analgesia have become increasingly popular. “The use of modern anesthesia techniques has significantly improved patient outcomes by reducing pain and minimizing the risk of complications,” notes a leading anesthesiologist.
Pre-emptive Pain Management Strategies
Pre-emptive pain management involves administering analgesia before the surgical incision to reduce the intensity of postoperative pain. This approach can include the use of nonsteroidal anti-inflammatory drugs (NSAIDs), gabapentinoids, or other analgesics. By starting pain management early, patients tend to have a smoother recovery with less discomfort.
Key benefits of pre-emptive pain management include:
- Reduced postoperative pain
- Lower opioid consumption
- Faster recovery times
Anesthesia Options and Their Effects on Recovery
The choice of anesthesia can significantly impact the recovery process. Different anesthesia options, such as general anesthesia versus regional anesthesia, have varying effects on postoperative pain and patient recovery. For instance, regional anesthesia techniques, including epidural and spinal anesthesia, can provide effective pain relief with potentially fewer systemic side effects compared to general anesthesia.
“The type of anesthesia used can greatly influence not only the immediate surgical experience but also the overall recovery trajectory of the patient,” says a renowned expert in anesthesiology.
By understanding the different anesthesia options and their implications for pain management, patients can make more informed decisions about their care.
Post-Operative Pain Management Protocols
Post-operative pain management plays a vital role in ensuring the success of bariatric surgery. Effective pain management not only enhances patient comfort but also contributes to a smoother and more efficient recovery process.
Medication-Based Pain Control Strategies
Medication-based pain control is a cornerstone of post-operative pain management. Various medications are used to manage pain, including opioids, NSAIDs, and acetaminophen. The choice of medication depends on the type of surgery, the patient’s medical history, and the severity of pain.
Commonly used pain medications include:
- Opioids (e.g., morphine, fentanyl)
- NSAIDs (e.g., ibuprofen, ketorolac)
- Acetaminophen
Medication Type | Examples | Primary Use |
Opioids | Morphine, Fentanyl | Severe pain management |
NSAIDs | Ibuprofen, Ketorolac | Moderate pain, anti-inflammatory |
Acetaminophen | Tylenol | Mild to moderate pain, fever reduction |
Non-Pharmaceutical Pain Management Approaches
In addition to medication, several non-pharmaceutical approaches can help manage post-operative pain. These include:
- Breathing exercises and relaxation techniques
- Physical therapy and gentle mobilization
- Cold therapy and compression garments
Hospital vs. Home Pain Management
Pain management strategies differ between hospital and home settings. In the hospital, patients have access to a range of pain management options, including epidural anesthesia and PCA (Patient-Controlled Analgesia) pumps. At home, patients rely on oral medications and non-pharmaceutical approaches.
Key differences between hospital and home pain management include:
- Availability of medical staff
- Access to advanced pain management technologies
- Patient education and support
By understanding the different pain management protocols available, patients can better navigate their recovery journey and achieve optimal outcomes.
Emotional and Psychological Aspects of Pain Management
Bariatric surgery patients often face a complex interplay between physical pain and emotional distress during recovery. The emotional and psychological aspects of pain management are crucial for a holistic recovery.
Anxiety and Its Impact on Pain Perception
Anxiety can significantly amplify the perception of pain. When patients are anxious, their bodies are more tense, which can make pain feel more intense. Pre-operative anxiety is common among bariatric surgery patients, and it can affect post-operative pain levels.
Coping with anxiety through relaxation techniques, such as deep breathing or meditation, can help mitigate its impact on pain perception. Mindfulness practices have also been shown to reduce anxiety and improve pain management.
Coping Strategies for Pain-Related Stress
Developing effective coping strategies is vital for managing pain-related stress. Patients can benefit from:
- Keeping a pain journal to track pain levels and identify patterns.
- Engaging in gentle physical activities, like walking, to reduce stiffness and improve mood.
- Practicing relaxation techniques, such as progressive muscle relaxation or guided imagery.
These strategies can help patients feel more in control of their pain and reduce overall stress levels.
Support Groups and Mental Health Resources
Support groups provide a community for patients to share their experiences and receive support from others who are going through similar challenges. Mental health resources, including counseling and therapy, can also play a critical role in managing the emotional aspects of pain.
Access to these resources can significantly improve a patient’s ability to cope with pain and navigate the recovery process. Professional guidance can help patients develop personalized coping strategies and address any underlying mental health concerns.
Recovery Timeline and Pain Progression After Bariatric Surgery
The recovery process following bariatric surgery is characterized by distinct stages of pain progression. Understanding these stages is essential for patients to manage their expectations and recovery effectively.
First 24-48 Hours Post-Surgery
The initial 24 to 48 hours after bariatric surgery are typically the most uncomfortable, with patients experiencing significant pain. This discomfort is usually managed with a combination of pain medications and rest. It’s crucial for patients to follow their healthcare provider’s instructions for pain management during this period.
Key considerations during the first 24-48 hours include:
- Adhering to prescribed pain medication schedules
- Maintaining adequate hydration
- Gradually increasing mobility as advised by healthcare professionals
First Week of Recovery
During the first week, the intensity of pain generally decreases, but some discomfort may persist. Patients are usually advised to continue pain management strategies and start introducing light activities into their routine.
Notable aspects of the first week include:
- Gradual reduction in pain levels
- Introduction to a liquid diet, progressing to soft foods
- Increased mobility, with a focus on gentle exercises
Gradual Return to Normal Activities
As patients progress beyond the first week, they can start resuming more normal activities. However, it’s essential to do so gradually to avoid complications and manage pain effectively.
Tips for a smooth return to normal activities:
- Listen to your body and rest when needed
- Follow dietary guidelines to avoid discomfort
- Engage in physical activities as recommended by your healthcare provider
By understanding the recovery timeline and pain progression after bariatric surgery, patients can better prepare themselves for the journey ahead, ensuring a smoother and more comfortable recovery process.
Nutritional Considerations and Their Impact on Recovery Pain
The role of nutrition in recovery pain after weight loss surgery cannot be overstated. A well-planned diet helps in managing pain and supporting the healing process. Nutritional considerations are crucial for a smooth and comfortable recovery.
Dietary Progression and Discomfort Levels
After bariatric surgery, patients typically follow a staged dietary progression, starting with liquids, then moving to pureed foods, and eventually to solid foods. This progression helps minimize discomfort and allows the digestive system to heal.
A study published in a Journal found that patients who adhered to their post-operative dietary plan experienced less pain and fewer complications. The dietary progression is designed to reduce the risk of discomfort and complications.
Diet Stage | Foods Allowed | Expected Discomfort Level |
Liquid Diet | Clear broths, electrolyte-rich beverages | Low |
Pureed Diet | Pureed fruits, vegetables, and proteins | Moderate |
Solid Foods | Soft, then regular foods | Variable |
Hydration and Pain Management
Proper hydration is essential for managing pain and supporting the healing process. Dehydration can lead to increased pain and discomfort. Patients are advised to drink plenty of water and limit caffeinated and sugary beverages.
“Staying hydrated is crucial for recovery. I was advised to drink at least 8 cups of water a day, and it really helped me manage my pain.” – Rachel, gastric sleeve patient
Adequate hydration helps in reducing the risk of complications and promotes overall well-being. It is also important to avoid dehydration, as it can exacerbate pain.
Supplements and Their Role in Healing
After bariatric surgery, patients may require supplements to ensure they get essential nutrients. Vitamins and minerals such as vitamin B12, iron, and calcium are commonly recommended. These supplements support the healing process and help prevent deficiencies.
A registered dietitian or healthcare provider can advise on the necessary supplements and their dosages. It’s essential to follow their recommendations to ensure proper nutrition and minimize potential complications.
In conclusion, nutritional considerations play a significant role in managing recovery pain after bariatric surgery. By following a staged dietary progression, staying hydrated, and taking necessary supplements, patients can minimize discomfort and support their overall healing process.
Physical Activity and Pain Levels During Recovery
The relationship between physical activity and pain during the recovery period is a critical consideration for bariatric surgery patients. Understanding how to manage physical activity can significantly impact pain levels and overall recovery experience.
Safe Exercise Introduction Timeline
Introducing exercises safely after bariatric surgery is crucial for minimizing pain and ensuring a smooth recovery. Generally, patients are advised to start with gentle movements and gradually increase the intensity based on their comfort and pain levels.
Typically, the timeline for introducing exercises looks like this:
Time Post-Surgery | Recommended Activities | Expected Pain Levels |
First 24-48 hours | Gentle stretching, short walks | High |
1-2 weeks | Light aerobic exercises, such as walking | Moderate |
2-6 weeks | Progressive resistance training, more intense aerobics | Low to Moderate |
Activities That May Increase or Decrease Pain
Certain activities can significantly impact pain levels during recovery. Understanding these can help patients manage their pain more effectively.
- Activities that may increase pain: Lifting heavy objects, bending, high-impact exercises.
- Activities that may decrease pain: Gentle stretching, yoga, short walks.
Building Strength Without Increasing Discomfort
Building strength is an essential part of the recovery process, but it should be done in a way that does not increase discomfort. Patients are advised to start with low-intensity exercises and gradually increase the intensity.
For example, beginning with isometric exercises can help build strength without putting too much strain on the body. As recovery progresses, patients can move on to more dynamic exercises.
It’s also crucial to listen to the body and stop if pain increases. Consulting with healthcare providers or physical therapists can provide personalized guidance on safe exercises.
Potential Complications and Their Impact on Pain Levels
Understanding potential complications after bariatric surgery is crucial for managing pain. While bariatric surgery is generally safe, as with any surgical procedure, there are risks involved, and complications can occur.
Common Complications That May Increase Pain
Some common complications that may arise after bariatric surgery include infection, bleeding, and internal hernias. These complications can significantly increase pain levels and may require additional medical intervention. For instance, an infection can cause severe pain, swelling, and redness at the surgical site, while internal hernias can lead to sharp, cramping pains.
Infection is a serious complication that can occur after bariatric surgery. Signs of infection include fever, increased pain, and redness or swelling around the incision site. Prompt treatment with antibiotics is usually necessary to manage the infection and prevent further complications.
Warning Signs That Pain May Indicate a Problem
It’s essential for patients to be aware of the warning signs that pain may indicate a complication. Severe or worsening pain, pain that doesn’t respond to medication, and pain accompanied by other symptoms like fever or vomiting are all red flags. Patients should be vigilant and report any unusual or concerning symptoms to their healthcare provider.
- Severe or worsening pain
- Pain not relieved by medication
- Pain accompanied by fever, vomiting, or other concerning symptoms
When to Contact Your Healthcare Provider
If patients experience any of the warning signs mentioned, they should not hesitate to contact their healthcare provider. Early detection and treatment of complications can significantly improve outcomes and reduce the risk of long-term issues. Patients are encouraged to reach out to their healthcare team with any questions or concerns about their pain or overall recovery.
Prompt communication with healthcare providers is key to addressing potential complications effectively.
Conclusion: Making an Informed Decision About Bariatric Surgery
Making an informed decision about bariatric surgery involves understanding the different procedures, their associated pain levels, and the factors that influence pain perception. By considering these elements, individuals can better prepare themselves for the surgical experience and subsequent recovery.
Bariatric surgery options, including LAP-BAND, gastric sleeve, gastric bypass, and duodenal switch, each have unique characteristics that impact pain levels. Understanding these differences is crucial for setting realistic expectations and choosing the most suitable procedure.
An informed decision is rooted in a comprehensive understanding of not only the surgical techniques and pain management strategies but also the emotional and psychological aspects of the journey. By being aware of these factors, individuals can navigate their recovery more effectively.
Ultimately, the goal of bariatric surgery is to improve overall health and well-being. By carefully considering the available options and their implications, individuals can make a decision that aligns with their needs and promotes a successful outcome.
FAQ
What are the different types of bariatric surgeries available?
The most common types of bariatric surgeries include Laparoscopic Adjustable Gastric Band (LAP-BAND), Gastric Sleeve Surgery, Gastric Bypass Surgery, and Duodenal Switch. Each procedure has its unique characteristics and implications for pain.
How is pain measured in bariatric surgical procedures?
Pain is typically measured using subjective pain scales, such as the Visual Analog Scale (VAS) or the Numeric Rating Scale (NRS), where patients rate their pain from 0 to 10 or 0 to 100.
What factors influence pain perception after weight loss surgery?
Individual pain thresholds, pre-existing medical conditions, and psychological factors, such as anxiety and stress, can significantly impact pain perception after bariatric surgery.
Which bariatric procedure is considered the least painful?
The LAP-BAND procedure is often considered one of the least painful bariatric surgeries due to its minimally invasive nature and relatively simple surgical technique.
How does the role of anesthesia impact pain control during bariatric surgery?
Modern anesthesia techniques, including pre-emptive pain management strategies, play a crucial role in controlling surgical pain during bariatric surgery, reducing the need for post-operative pain medication.
What are the typical pain management protocols after bariatric surgery?
Post-operative pain management protocols typically involve a combination of medication-based pain control strategies and non-pharmaceutical approaches, such as relaxation techniques and breathing exercises.
How can nutritional considerations impact recovery pain after bariatric surgery?
Dietary progression, hydration, and the use of supplements can significantly impact recovery pain, with a balanced diet and adequate hydration helping to minimize discomfort.
What is the relationship between physical activity and pain levels during recovery?
Gradually introducing physical activity, such as walking, can help reduce pain levels during recovery, while avoiding strenuous activities can prevent discomfort and complications.
What are the warning signs that pain may indicate a problem after bariatric surgery?
Severe or worsening pain, fever, vomiting, or difficulty swallowing are warning signs that may indicate a complication, and patients should contact their healthcare provider immediately if they experience any of these symptoms.
How can support groups and mental health resources help with pain management?
Support groups and mental health resources can provide emotional support, coping strategies, and stress management techniques, helping patients to better manage their pain and overall well-being.
What is the typical recovery timeline and pain progression after bariatric surgery?
The recovery timeline and pain progression vary depending on the individual and the type of surgery, but most patients can expect to experience significant pain reduction within the first week after surgery, with gradual improvement over the following weeks.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32440778/