
Pregnancy brings many changes to the body. While these changes are needed for a healthy pregnancy, they also raise the risk of problems like blood clots. It’s important for pregnant women to know about the risks and signs of blood clots.Don’t ignore leg pain during pregnancy. This critical warning sign could indicate a serious problem. Get powerful, essential information now.
Blood clots often form in the deep veins of the legs. This is called Deep Vein Thrombosis (DVT). It’s key to spot the signs of DVT, like leg pain or swelling, to get help quickly.
Key Takeaways
- Blood clots are a possible problem during pregnancy.
- DVT is a common issue with blood clots in the legs.
- Symptoms of DVT include leg pain and swelling.
- Knowing these symptoms is important for pregnant women.
- Quick medical help is needed if DVT symptoms show up.
Understanding Blood Clots During Pregnancy
Pregnancy brings many changes to the body, some of which raise the risk of blood clots. It’s key to know what causes these clots.
Why Pregnant Women Are at Higher Risk
Pregnant women face a higher risk of blood clots for several reasons. Changes in blood composition and increased blood volume play a part. Also, the growing uterus puts pressure on veins, helping clots form.
During pregnancy, hormonal changes lead to an increased tendency for blood clotting, which helps prevent excessive bleeding during childbirth. This is to prevent too much bleeding during childbirth.
| Risk Factor | Description |
| Changes in Blood Composition | Increased clotting factors and decreased anticoagulant proteins. |
| Increased Blood Volume | Greater blood volume puts more pressure on veins. |
| Pressure on Veins | The growing uterus can compress veins, specially in the legs and pelvis. |
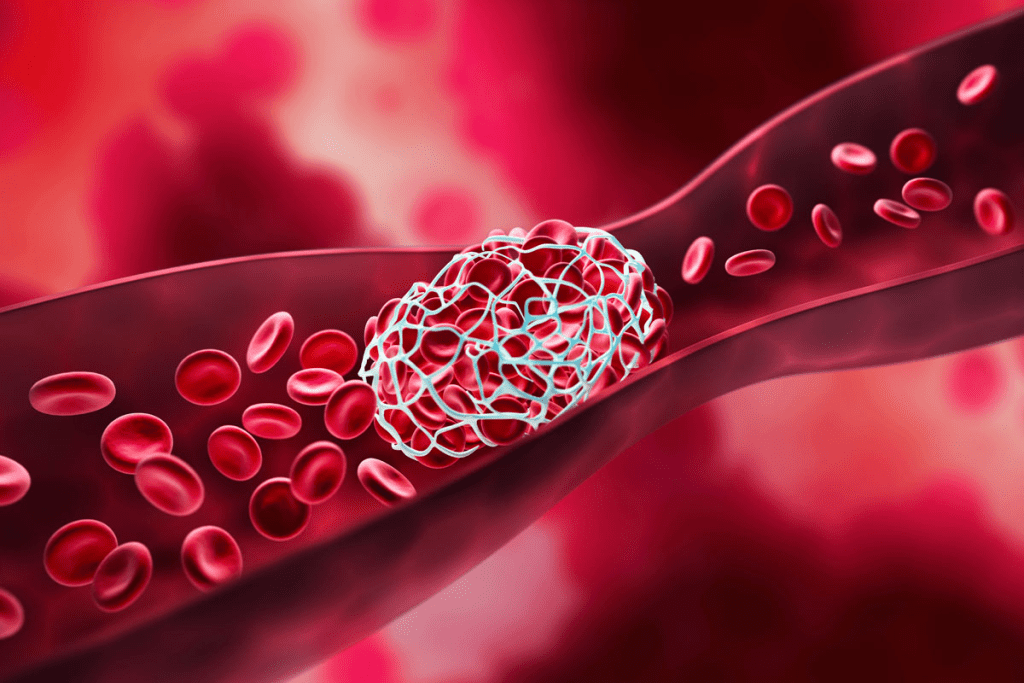
Types of Blood Clots That Can Occur During Pregnancy
There are two main types of blood clots in pregnancy: Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). DVT is a clot in the deep veins, usually in the legs. PE happens when a clot travels to the lungs, which can be deadly.
Knowing about these risks and types of clots is vital for safe pregnancy management. We’ll look at symptoms, diagnosis, and treatments next.
Common Symptoms of Deep Vein Thrombosis (DVT) During Pregnancy
It’s important to know the signs of Deep Vein Thrombosis (DVT) during pregnancy. DVT is a blood clot in the deep veins, usually in the legs. Spotting its symptoms early can prevent serious problems.
Leg Pain and Swelling
Leg pain or tenderness, often with swelling, is a main symptom of DVT. This pain can be mild or very sharp. It’s key to tell normal pregnancy leg pain from DVT symptoms. Look out for:
- Pain or tenderness in one leg (rarely in both)
- Swelling in the affected leg
- Warmth or redness of the skin
If you have these symptoms, seek medical help right away, if they’re severe or get worse.
Skin Changes and Temperature Differences
DVT can also cause skin changes in the affected leg. You might see redness or discoloration, and the skin could feel warm or hot. Watch these signs closely, as they might mean a blood clot is present.
Some women notice a temperature difference between their legs. If you see unusual skin changes or temperature differences, talk to your healthcare provider.
Knowing these symptoms and telling your healthcare provider can help manage and treat DVT during pregnancy.
Leg Pain During Pregnancy: When to Worry About Blood Clots
Leg pain is common in pregnancy, but it’s key to know the difference between normal pain and signs of deep vein thrombosis (DVT). We’ll look at the signs of normal pregnancy pain and when to worry about blood clots. We’ll also talk about when you should see a doctor right away.
Normal Pregnancy Leg Pain vs. DVT Pain
Women often feel leg pain during pregnancy due to weight gain and posture changes. But not all pain is the same. Normal pregnancy leg pain is usually mild and gets better with rest or at the end of the day.
DVT pain, on the other hand, is severe and doesn’t get better with rest. It can also cause swelling, redness, or warmth. It’s important to watch for any severe or worsening pain in your legs.
- Normal pregnancy leg pain often improves with rest or elevation of the legs.
- DVT pain usually doesn’t improve with rest and may worsen over time.
- Pain from DVT is often unilateral, affecting one leg.
Red Flags That Require Immediate Attention
Some symptoms with leg pain in pregnancy are warning signs for DVT and need quick medical help. These include:
- Swelling of the leg, ankle, or foot.
- Pain or tenderness in the leg, specially when standing or walking.
- Redness or discoloration of the skin.
- Warmth or tenderness to the touch.
- Visible veins or a palpable cord.
“If you experience any of these symptoms, it’s vital to seek medical care quickly. Early treatment of DVT can greatly improve outcomes and prevent serious problems.”
Knowing these differences and warning signs helps pregnant women take care of their health. It also helps them know when to get medical help.
Pulmonary Embolism Symptoms in Pregnant Women
It’s key for pregnant women to know the signs of pulmonary embolism. This condition is a blockage in the lungs’ arteries, often caused by blood clots. Spotting these symptoms early is vital for quick medical help.
Breathing Difficulties and Chest Pain
Shortness of breath or trouble breathing is a main symptom. Chest pain can also happen, getting worse with deep breaths or coughs. This pain might be confused with heart attacks or muscle pain.
These symptoms can pop up suddenly and be quite severe. If you find yourself having trouble breathing or chest pain, get help right away.
Other Warning Signs of Pulmonary Embolism
Other signs include:
- Rapid heartbeat
- Coughing up blood
- Lightheadedness or dizziness
- Fainting
These signs can be different in how bad they are. But, if you notice any, get medical help fast.
| Symptom | Description |
| Shortness of Breath | Sudden trouble breathing or feeling winded even when sitting |
| Chest Pain | Pain or discomfort in the chest that gets worse with deep breaths or coughing |
| Rapid Heartbeat | A heart that beats too fast |
We stress the need to know these symptoms for quick medical care. If you see any, call your doctor or go to the emergency room.
Risk Factors for Developing Blood Clots While Pregnant
It’s important for pregnant women to know about blood clot risks. We’ll look at what increases the chance of blood clots during this time.
Pre-existing Medical Conditions
Some health issues before pregnancy can raise blood clot risks. These include:
- Genetic Blood Clotting Disorders: Conditions like Factor V Leiden and Prothrombin G20210A mutation can make blood more prone to clotting.
- Autoimmune Disorders: Diseases such as lupus and antiphospholipid syndrome can increase clotting risk.
- Heart Disease: Pre-existing heart conditions can complicate pregnancy and increase the risk of blood clots.
- Diabetes: Uncontrolled diabetes can lead to vascular complications, increasing the risk of clot formation.
Women with these conditions need close monitoring by their healthcare providers to manage risks effectively.
Pregnancy-Specific Risk Factors
Pregnancy brings changes that can raise blood clot risks. Some of these include:
| Risk Factor | Description |
| Multiple Pregnancy | Carrying twins, triplets, or more increases the risk due to higher blood volume and greater pressure on veins. |
| Age Over 35 | Women over 35 years old are at a higher risk of developing blood clots during pregnancy. |
| Immobility | Prolonged bed rest or immobility during pregnancy can increase the risk of clot formation. |
| Preeclampsia | This condition, characterized by high blood pressure and often protein in the urine, can increase clotting risk. |
Knowing these risk factors helps expectant mothers and their healthcare providers prevent blood clots.
How Blood Clots Are Diagnosed During Pregnancy
When a pregnant woman shows signs of a blood clot, doctors use many tools to find and check the clot. Finding blood clots in pregnancy is hard because of the body’s changes. But it’s key to keep both mom and baby safe.
Safe Diagnostic Tests for Pregnant Women
Pregnant women need tests that are safe for them and their babies. The main tests are:
- Ultrasound: This is often the first test for deep vein thrombosis (DVT). It’s safe and doesn’t hurt.
- D-dimer test: It’s not always sure because it can show false positives in pregnancy. But it’s used with other tests and checks.
- Ventilation-perfusion (V/Q) scan or CT pulmonary angiography (CTPA): These are for pulmonary embolism. The choice depends on the baby’s age and what tests are available.
What to Expect During Diagnosis
During diagnosis, you’ll get a full check-up. This includes talking about your health and a physical exam. Doctors will look at your symptoms and risk factors and do tests to confirm the diagnosis.
Talking openly with your doctor about your symptoms and worries is very important. This makes the process smoother and safer for you.
Diagnosing blood clots in pregnancy involves many steps. It includes a check-up, lab tests, and imaging. Knowing what to expect can help reduce stress and make sure you get the right care.
Treatment Options for Blood Clots in Pregnancy
Pregnancy makes treating blood clots more complex. Doctors must find a balance between treating the mother and protecting the baby. The main goal is to stop the clot from getting bigger, avoid pulmonary embolism, and prevent complications.
Anticoagulant Medications Safe for Pregnancy
Anticoagulant medications are key in treating blood clots during pregnancy. They stop new clots from forming and prevent existing ones from growing. Low Molecular Weight Heparin (LMWH) is often chosen because it’s safe for the fetus and works well.
Using these medications requires close monitoring. This is to make sure they work right and don’t cause too much bleeding. Doctors will check blood tests regularly to adjust the dosage as needed.
Non-Medication Treatments and Interventions
There are also non-medication ways to manage blood clots in pregnancy. Compression stockings help improve blood flow and reduce swelling in the legs. In some cases, inferior vena cava (IVC) filters might be used for women who can’t take anticoagulants or have clots that keep coming back.
Moving around and avoiding sitting for too long is also important. Pregnant women should try to stay active, but only as much as they can comfortably. Being active helps keep blood flowing and lowers the chance of clots.
Every treatment plan is different. It depends on the specific situation of each pregnancy. This includes the clot’s location and size, how far along the pregnancy is, and any other health issues.
Preventing Blood Clots During Pregnancy
During pregnancy, hormonal changes lead to an increased tendency for blood clotting, which helps prevent excessive bleeding during childbirth.
Lifestyle Changes for Prevention
There are some lifestyle changes that can help prevent blood clots. These include drinking lots of water, keeping a healthy weight, and exercising regularly.
- Drink plenty of water throughout the day to stay hydrated.
- Engage in low-impact exercises like walking or swimming.
- Avoid prolonged periods of standing or sitting.
Wearing compression stockings can also help. They improve blood flow and lower the chance of clots.
Medical Prevention Strategies
In some cases, medical help is needed to prevent blood clots. This is usually for women at high risk.
| Prevention Strategy | Description | Benefits |
| Anticoagulant Medications | Medications that prevent blood clot formation. | Reduces risk of clot formation, safe for use during pregnancy. |
| Compression Stockings | Stockings that improve blood circulation. | Improves circulation, reduces swelling. |
| Regular Monitoring | Regular check-ups to monitor clotting risks. | Early detection of possible issues. |
Talking to your healthcare provider is a good idea. They can help figure out the best plan for you.
By making lifestyle changes and using medical help when needed, pregnant women can lower their risk of blood clots.
Managing Discomfort in Legs During Pregnancy
As pregnancy goes on, leg pain can become a big problem. But, there are ways to feel better. We’ll look at safe exercises and home remedies to help.
Safe Exercises for Improving Circulation
Exercise is good for pregnant women, helping blood flow and easing pain. Safe exercises during pregnancy include:
- Walking: A simple and effective way to improve circulation.
- Prenatal yoga: Helps maintain flexibility and reduces muscle tension.
- Swimming: A low-impact exercise that can help alleviate leg pain.
- Leg swings: Standing or sitting, gently swinging your legs can improve blood flow.
Always talk to your doctor before starting new exercises to make sure they’re safe for you.
Home Remedies for Pregnancy Leg Pain
There are also home remedies for leg pain to try:
- Elevating your legs: Regularly elevating your legs above the level of your heart can help reduce swelling.
- Warm compresses: Applying a warm compress to the affected area can help relax muscles.
- Massage: Gentle massage can help improve circulation and reduce muscle cramps.
- Staying hydrated: Drinking plenty of water is essential for maintaining good circulation.
To manage leg pain during pregnancy, mix safe exercises, home remedies, and lifestyle changes. These steps can help you feel better and have a healthier pregnancy.
Blood Clots in Unusual Locations During Pregnancy
Blood clots often show up in the legs during pregnancy. But they can also appear in other places, which is risky. Knowing these spots is key to getting help fast.
Cerebral Venous Sinus Thrombosis
Cerebral venous sinus thrombosis (CVST) is a rare but serious issue. It happens when a blood clot forms in the brain’s sinuses. Symptoms include severe headaches, confusion, and seizures.
CVST needs quick medical care because it can lead to serious problems. Finding CVST can be hard because its signs are similar to other conditions. But, quick use of MRI or CT scans is vital for the right treatment.
Treatment usually involves medicines to stop the clot from getting bigger. It also helps prevent more clots from forming.
Pelvic and Abdominal Vein Thrombosis
Pelvic and abdominal vein thrombosis means blood clots in the pelvis or abdomen. It can cause pain in the abdomen and flank, and fever. This is a serious issue that needs medical attention.
This condition is linked to pregnancy problems. Ultrasound and CT scans are used to diagnose it. Treatment might include medicines to prevent clotting and other steps to manage symptoms.
It’s important for pregnant women and doctors to know about these unusual blood clot locations. By understanding the risks and signs, we can work together for the best results.
Postpartum Blood Clot Risks and Symptoms
The risk of blood clots doesn’t stop after the baby is born. In fact, it continues into the postpartum period. It’s important to understand why this risk persists and what new mothers can watch out for.
Why the Risk Continues After Delivery
Several factors contribute to the increased risk of blood clots during the postpartum period. Changes in blood clotting factors and increased venous pressure in the legs and pelvis during pregnancy can persist after delivery. Also, cesarean delivery and immobility during the postpartum recovery period can further increase this risk.
Signs to Watch for After Childbirth
New mothers should be aware of the following symptoms that could indicate a blood clot:
- Leg pain or swelling, which could be a sign of deep vein thrombosis (DVT).
- Chest pain or difficulty breathing, which could indicate a pulmonary embolism (PE).
- Severe headache or neurological symptoms, which could be signs of a cerebral venous sinus thrombosis (CVST).
When to Seek Emergency Medical Care
Knowing when to seek emergency care for blood clots during pregnancy is key. Blood clots can be deadly if not treated fast. It’s vital to know the symptoms that need quick action.
Symptoms That Shouldn’t Wait
Certain symptoms mean serious risks and should not be ignored. These include:
- Severe leg pain or swelling that doesn’t get better with rest or elevation.
- Chest pain or trouble breathing, which could mean a pulmonary embolism.
- Severe headache or confusion, possibly from a cerebral venous sinus thrombosis.
- Abdominal pain or tenderness, possibly from a clot in the pelvic or abdominal veins.
If you have these symptoms, get medical help right away. Don’t wait to see if symptoms go away on their own. Quick action can greatly improve your chances.
What to Tell Your Healthcare Provider
When you seek emergency care, give your healthcare provider all the details. Be ready to:
- Tell them about your symptoms, when they started, and what makes them better or worse.
- Share your medical history, including any past blood clots, family clotting disorders, and current meds.
- Talk about any recent travel, being immobile, or surgery, as these can raise clot risks.
The American College of Obstetricians and Gynecologists (ACOG) stresses the importance of quick diagnosis and treatment. Being informed and ready can greatly help your care.
By knowing the symptoms that need quick medical help and what to tell your healthcare provider, you can protect your health during pregnancy.
Long-Term Implications of Blood Clots During Pregnancy
Pregnant women with blood clots face a higher risk of heart problems later on. They need to keep an eye on their health. Doctors say blood clots during pregnancy can lead to serious health issues.
We’ll look at the long-term effects, including risks in future pregnancies. It’s important to talk to doctors about these risks. This way, they can help manage them.
Future Pregnancy Considerations
Women who had blood clots during pregnancy should know the risks for future pregnancies. Studies show they’re more likely to have blood clots again. It’s key to:
- Tell doctors about the previous blood clot
- Discuss ways to prevent blood clots
- Watch for signs of blood clots in future pregnancies
Long-Term Health Monitoring
Women with blood clots during pregnancy need to keep an eye on their health. They should see doctors regularly. This helps catch any long-term problems early.
One study found women with blood clots during pregnancy should watch their heart health. It’s wise to work with doctors to plan for ongoing health checks.
Understanding the risks of blood clots during pregnancy is key. Taking steps now can help avoid future problems. This ensures the best health outcomes for women.
Conclusion
It’s vital for pregnant women to know about blood clot risks and symptoms. We talked about different types of blood clots and who might be at higher risk. This includes deep vein thrombosis and pulmonary embolism.
Knowing the symptoms like leg pain, swelling, and trouble breathing is key. If you notice these, get medical help right away. Taking steps to prevent blood clots can help keep you and your baby safe.
Being informed and proactive is the best way to handle blood clot risks in pregnancy. By understanding the risks and taking action, you can have a healthier pregnancy. Always talk to your healthcare provider for advice tailored to you.
FAQ
What are the common symptoms of a blood clot during pregnancy?
Symptoms include leg pain or swelling, skin changes, and temperature differences in the affected leg. Some women may also experience breathing difficulties or chest pain if the clot breaks loose and travels to the lungs.
How can I differentiate between normal leg pain during pregnancy and pain caused by a blood clot?
Normal pregnancy-related leg pain is usually mild and manageable. Pain from a blood clot can be severe, persistent, and accompanied by swelling or skin changes. If you’re experiencing severe or unusual pain, it’s essential to consult your healthcare provider.
What are the risk factors for developing blood clots during pregnancy?
Risk factors include pre-existing medical conditions, such as thrombophilia. Pregnancy-specific factors like multiple pregnancy, cesarean delivery, or a family history of blood clots also increase the risk.
How are blood clots diagnosed during pregnancy?
Diagnosis involves a combination of physical examination, ultrasound, and sometimes blood tests. Your healthcare provider will determine the best diagnostic approach based on your individual situation.
What are the treatment options for blood clots during pregnancy?
Treatment usually involves anticoagulant medications that are safe for use during pregnancy. In some cases, non-medication interventions like compression stockings or bed rest may be recommended.
Can blood clots be prevented during pregnancy?
Yes, there are steps you can take to reduce your risk. Staying active, maintaining a healthy weight, and avoiding prolonged periods of immobility are important. Your healthcare provider may also recommend medical prevention strategies if you have a high-risk profile.
What are the symptoms of pulmonary embolism during pregnancy?
Symptoms include sudden onset of breathing difficulties, chest pain, rapid heartbeat, and sometimes coughing up blood. If you experience any of these symptoms, seek immediate medical attention.
Are there any long-term implications of having a blood clot during pregnancy?
Yes, having a blood clot during pregnancy may increase your risk of future blood clots. Your healthcare provider will discuss the implications for future pregnancies and provide guidance on managing your risk.
Can I exercise with leg pain during pregnancy?
Gentle exercises like walking or stretching can help alleviate leg pain and improve circulation. It’s important to consult your healthcare provider before starting any new exercise program, as severe or persistent pain may require special attention.
What are the signs of blood clots in unusual locations, such as cerebral venous sinus thrombosis?
Symptoms can vary depending on the location of the clot. For cerebral venous sinus thrombosis, symptoms may include severe headache, confusion, or seizures. If you experience any unusual or severe symptoms, seek immediate medical attention.
Do blood clot risks continue after delivery?
Yes, the risk of blood clots persists after delivery, even in the postpartum period. Be aware of the signs and symptoms, and seek medical attention if you experience anything unusual.
References
NHS. (2025, August 13). Deep vein thrombosis in pregnancy. https://www.nhs.uk/pregnancy/related-conditions/complications/deep-vein-thrombosis


































