Last Updated on November 20, 2025 by Ugurkan Demir

Getting a leukemia diagnosis can be tough. Knowing about the chemotherapy drugs and regimens for Acute Lymphoblastic Leukemia (ALL) is key. At Liv Hospital, we focus on our patients and offer top-notch leukemia care. We use international-quality treatments and provide expert help.
For ALL, treatment often includes leukaemia chemotherapy. The goal is to get the patient into remission and prevent the disease from returning. Our detailed guide covers the main drugs and treatment plans for managing ALL.

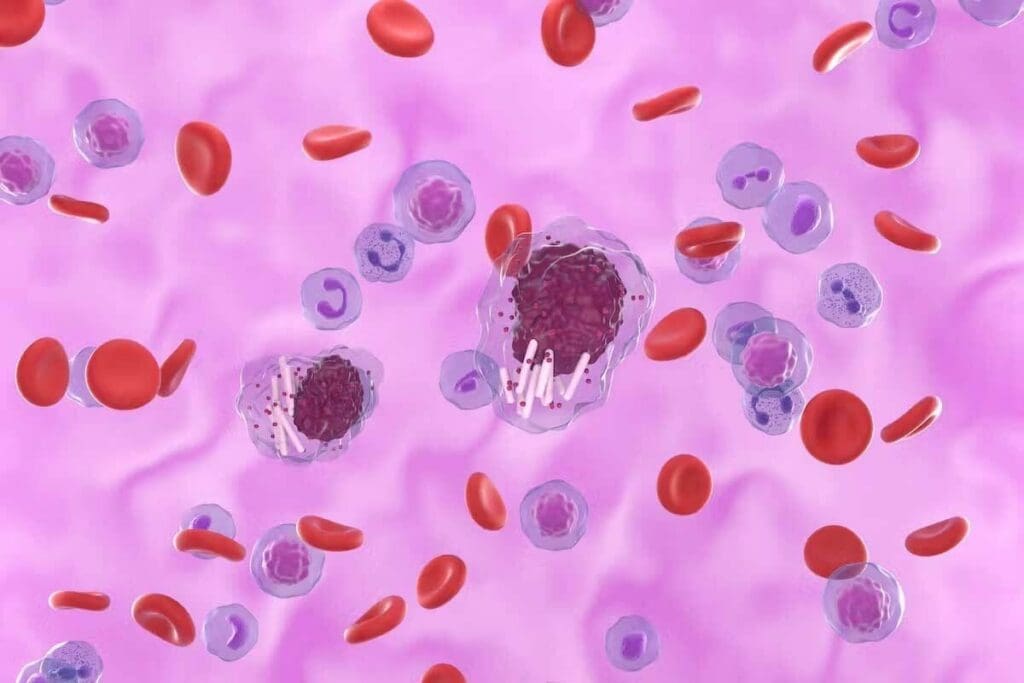
ALL, or Acute Lymphoblastic Leukemia, is a serious challenge in cancer treatment. It quickly spreads and harms the body’s ability to make healthy blood cells. This blood cancer affects the bone marrow, where it makes too many immature white blood cells.
ALL makes too many immature cells in the bone marrow. This makes it hard for the body to fight off infections. It can happen to both kids and adults, but kids are more likely to get it. The exact cause is not known, but some genetic and environmental factors can raise the risk.
Chemotherapy is the main treatment for ALL. It uses drugs to kill the cancer cells. The goal is to get the disease into remission, where it’s no longer found.
According to the Canadian Cancer Society, chemotherapy is often used with other treatments. It’s effective because it targets the fast-growing cancer cells in the body.
Every patient’s response to ALL is different. That’s why treatment plans need to be tailored to each person. We consider age, health, and the leukemia cells’ genetic makeup when planning treatment.
By personalizing treatment, we can improve results and lower the chance of side effects. Understanding ALL and its treatment is key for both patients and doctors. Keeping up with the latest in ALL chemotherapy helps us work together to better patient outcomes and quality of life.
ALL chemotherapy is given in three phases. Each phase has a specific goal to help achieve and keep remission. This structured approach makes sure the treatment plan fits the patient’s needs well.
The induction phase is the first step in ALL chemotherapy. It aims to quickly reduce the number of leukemia cells. A mix of chemotherapy drugs is used to kill leukemia cells in the bone marrow and blood.
The main goal is to achieve complete remission. This means no leukemia cells are found in the bone marrow or blood.
Key objectives of the induction phase include:
After the induction phase, the consolidation phase aims to get rid of any leftover leukemia cells. This phase is key to lowering the chance of relapse and improving survival chances. The chemotherapy used in consolidation might be different or stronger than in induction.
The consolidation phase is characterized by:
The maintenance phase is the last stage of ALL chemotherapy. It aims to keep remission going and prevent relapse for a long time. This phase uses less intense chemotherapy for months to years. It helps control any remaining leukemia cells and supports the body’s recovery.
Here’s an overview of the typical duration and key aspects of the maintenance phase:
| Phase | Duration | Key Aspects |
| Maintenance | Several months to a few years | Less intensive chemotherapy, monitoring for relapse, supporting recovery |
Understanding the three phases of ALL chemotherapy helps patients and healthcare providers better manage treatment. This approach improves outcomes and enhances quality of life.
In treating Acute Lymphoblastic Leukemia (ALL), vinca alkaloids and anthracyclines are key. These drugs have been mainstays for decades, helping manage the disease well.
Vincristine is a vinca alkaloid that stops microtubule formation. This action causes cell cycle arrest at metaphase. It’s very effective against fast-growing cancer cells.
Vincristine is given with other drugs to boost its effect. It’s given through an IV, with doses adjusted for each patient.
Daunorubicin is an anthracycline that works by intercalating DNA strands. It stops topoisomerase II and causes cancer cell death. It’s key in the induction phase of ALL treatment.
Daunorubicin’s dose is very important. It’s adjusted for each patient to avoid heart damage while keeping its cancer-fighting power. Continuous infusion and liposomal formulations help improve its safety and effectiveness.
| Drug | Dosing Strategy | Key Benefit |
| Daunorubicin | Continuous Infusion | Reduced Cardiotoxicity |
| Daunorubicin | Liposomal Formulation | Enhanced Therapeutic Index |
Doxorubicin is used in treating different ALL subtypes. It works like Daunorubicin, by intercalating DNA and stopping topoisomerase II.
In high-risk ALL subtypes, Doxorubicin is part of intense chemotherapy. But it’s used carefully to avoid heart damage. Close monitoring is needed.
Adding vinca alkaloids and anthracyclines to ALL treatment has greatly helped patients. Knowing how they work, their uses, and side effects is key to using them best.
Alkylating agents and enzyme therapies are key parts of chemotherapy for Acute Lymphoblastic Leukemia (ALL). They target leukemia cells in different ways. This makes treatment more effective.
Cyclophosphamide is a common alkylating agent in ALL treatment. It damages leukemia cells’ DNA, stopping them from growing. It’s used for:
Using cyclophosphamide in ALL treatment plans needs careful thought. This is to get the most benefit while keeping side effects low.
Pegaspargase is an enzyme therapy for ALL. It works by reducing asparagine levels. This stops leukemia cells from making proteins. It helps patients with certain types of ALL.
The benefits of pegaspargase include:
As we keep improving ALL treatment, alkylating agents and enzyme therapies are key. They help make treatment plans better. This has greatly improved patient results.
Antimetabolites are key in treating Acute Lymphoblastic Leukemia (ALL). They work by blocking the growth of cancer cells. This makes them very effective against fast-growing cancer cells.
We will look at three important antimetabolites: Methotrexate, Cytarabine, and Mercaptopurine. Each drug has its own way of helping in ALL treatment.
Methotrexate is a common drug in ALL treatment. It comes in standard and high-dose forms. The choice depends on the patient’s risk and how they respond to treatment.
High-dose Methotrexate is great for reaching cancer cells in the brain. This is important for treating the brain in ALL patients.
| Protocol | Dose | Application |
| Standard | 50-100 mg/m² | Initial treatment phases |
| High-Dose | 3-5 g/m² | CNS prophylaxis, intensification phases |
Cytarabine is vital in treating ALL, mainly in high-risk cases. It works well in different treatment plans. This makes it very useful.
In high-risk ALL, Cytarabine is often combined with other drugs. This makes the treatment stronger.
Mercaptopurine is an oral drug used in ALL treatment. It’s important to take it correctly to control the disease and reduce side effects.
How well Mercaptopurine works depends on the dose, how well the patient takes it, and their body’s metabolism.
In treating ALL, corticosteroids like prednisone and dexamethasone are key. They work with agents like nelarabine and thioguanine. These drugs are vital in all stages of chemotherapy.
Corticosteroids are essential in ALL treatment. Prednisone and dexamethasone are the most ucommonly sed. They differ in how well they work and their side effects.
Dexamethasone might be better for the brain because it lasts longer and gets in deeper. But it can cause more side effects, like bone damage.
| Corticosteroid | Half-life | CNS Penetration | Risk of Osteonecrosis |
| Prednisone | 12-36 hours | Moderate | Lower |
| Dexamethasone | 36-54 hours | Higher | Higher |
Nelarabine is a new drug for T-cell ALL. It stops DNA from working, killing cancer cells. This is a big win for a tough-to-treat type of ALL.
“Nelarabine has emerged as a critical component in the treatment of relapsed or refractory T-cell ALL, providing new hope for patients with limited previous options.”
Studies show nelarabine works well for both kids and adults with T-cell ALL. It’s now approved for this use.
Thioguanine is used in some ALL treatments. It messes with DNA and stops cancer cells from growing. It’s part of certain treatment plans.
Thioguanine is used in specific cases. Its role is being looked at in new treatments, too.
We’re always learning how to use these drugs to help ALL patients more.
Getting chemotherapy to the right place is key in fighting Acute Lymphoblastic Leukemia (ALL). The way we give the treatment affects how well it works and how safe it is.
Intravenous chemotherapy is a common way to treat ALL. It lets us give high doses straight into the blood. We watch patients closely for side effects and adjust the doses as needed.
We plan the timing of intravenous chemotherapy carefully. This helps it work best while keeping side effects low. Regular blood tests and checks help us catch any problems early.
Oral chemotherapy is easy to take at home. But, sticking to the schedule is very important. We teach patients why it’s key to follow their treatment plan closely.
Oral chemotherapy can be tricky because of side effects and drug interactions. Regular visits to the doctor help manage these risks.
Intrathecal therapy puts chemotherapy right into the spinal fluid. This helps stop and treat leukemia in the brain and spinal cord. Methotrexate and cytarabine are often used for this.
Targeting the brain and spinal cord is vital in ALL treatment. It helps prevent the disease from coming back in these areas. By putting chemotherapy directly into the spinal fluid, we can hit leukemia cells harder.
| Chemotherapy Administration Route | Key Characteristics | Clinical Considerations |
| Intravenous | Direct delivery into the bloodstream | High-dose capability, close monitoring required |
| Oral | Convenient for home administration | Adherence is key; drug interactions are possible |
| Intrathecal | Direct delivery into the spinal fluid | Great for brain and spinal cord treatment |
Knowing the pros and cons of each way to give chemotherapy helps us make treatment plans that fit each patient. This approach can lead to better results in fighting ALL.
ALL treatment has evolved, with chemotherapy plans made for different patients and disease types. We’ll look at the main chemotherapy plans for Acute Lymphoblastic Leukemia (ALL). This includes both treatments for kids and adults.
Pediatric ALL treatments aim to be effective yet gentle on kids. The Berlin-Frankfurt-Münster (BFM), Children’s Oncology Group (COG), and St. Jude Children’s Research Hospital methods are top choices.
The BFM protocol uses a strong chemotherapy plan that has been updated to achieve better results. COG protocols, by contrast, adjust treatment based on how high the risk is for each patient.
| Protocol | Key Features | Target Population |
| BFM | Intensive induction and consolidation phases | Pediatric patients with ALL |
| COG | Risk-stratified treatment approach | Pediatric patients with ALL |
| St. Jude | Total Therapy approach, incorporating multiple chemotherapy agents | Pediatric patients with ALL |
Adult ALL treatments are more intense than those for kids. This is because adults often face tougher challenges. The Hyper-CVAD regimen is a key example, mixing hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone.
Other plans, like CALGB 8811 and MRC UKALLXII/ECOG2993, have shown mixed results. These treatments often use a mix of drugs and might include targeted therapy for certain ALL types.
ALL with the Philadelphia chromosome is a special case. It’s caused by a swap between chromosomes 9 and 22. Thanks to tyrosine kinase inhibitors (TKIs) like imatinib and dasatinib, treatment has greatly improved.
Today, treatments for this type of ALL combine TKIs with chemotherapy. This combo has led to better results. Researchers are working to find the best way to use these treatments together.
Chemotherapy has made big strides in treating Acute Lymphoblastic Leukemia (ALL). New drugs and treatments are being developed to fight this blood cancer. This has grown the list of medicines for blood cancer, giving patients new hope.
Chemotherapy is key in managing leukemia. Research is ongoing to make current treatments better and find new ones. This work aims to improve how we treat leukemia.
Thanks to these advances, patients with ALL are doing better. Doctors are now tailoring treatments for different patients. The addition of drugs like nelarabine for T-Cell ALL has broadened treatment options.
Looking ahead, we can expect even more progress in leukemia treatment. New therapies and ways to improve chemotherapy are on the way. This will lead to better care for patients with ALL.
As research keeps moving forward, we’ll see more targeted and effective treatments. This will help patients with ALL get even better results. Our understanding of leukemia and how to treat it is growing, helping us fight this disease more effectively.
Acute Lymphoblastic Leukemia (ALL) is a blood cancer. It affects the bone marrow, where white blood cells are made. It’s common in kids but can also happen in adults.
Chemotherapy is the main treatment for ALL. It kills cancer cells all over the body. It’s often used with other treatments like targeted therapy or radiation.
ALL treatment has three phases: induction, consolidation, and maintenance. The first phase aims for initial remission. The second phase gets rid of any remaining cancer cells. The third phase helps keep the disease under control long-term.
Vinca alkaloids and anthracyclines are chemotherapy drugs. They stop cancer cells from growing. These drugs are key in ALL treatment.
Alkylating agents, like cyclophosphamide, damage cancer cells’ DNA. This stops them from making copies. They’re used with other drugs in ALL treatment.
Antimetabolites, like methotrexate and mercaptopurine, stop cancer cells from growing. They work by messing with DNA and RNA production. They’re a big part of ALL treatment.
Chemotherapy can be given in different ways. It can be injected, taken by mouth, or put directly into the brain. The method depends on the drug and the patient’s needs.
CNS-directed therapy targets the brain and spinal cord. It’s vital in ALL treatment. The brain is a common place for leukemia to come back.
There are many chemotherapy protocols for ALL. Pediatric ones, like BFM and COG, and adult ones, like Hyper-CVAD, are common. The right one depends on the patient’s needs and risk factors.
Philadelphia chromosome-positive ALL gets a special treatment. It combines chemotherapy with targeted therapy, like tyrosine kinase inhibitors. This is because of the unique genetic makeup of this type of ALL.
New treatments for ALL include immunotherapy and CAR-T cell therapy. There’s also a focus on making treatments more effective and less harsh. These are the future directions in ALL treatment.
Common leukemia treatments include vincristine, daunorubicin, doxorubicin, cyclophosphamide, methotrexate, and mercaptopurine. These drugs are key in fighting leukemia.
Oral chemotherapy is taken as pills or capsules. Patients must follow a strict schedule. The main challenges are making sure patients stick to it and managing side effects.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!