Last Updated on November 25, 2025 by
What cancers have high leukocytes? Learn the dangerous, crucial facts about leukocytosis and the powerful role of white blood cell count in hematologic malignancies.
High levels of leukocytes are a key sign in many cancers. They tell us about the disease’s severity and how it might affect survival. We’re discovering how high white blood cell counts link to different cancers, mainly blood cancers.
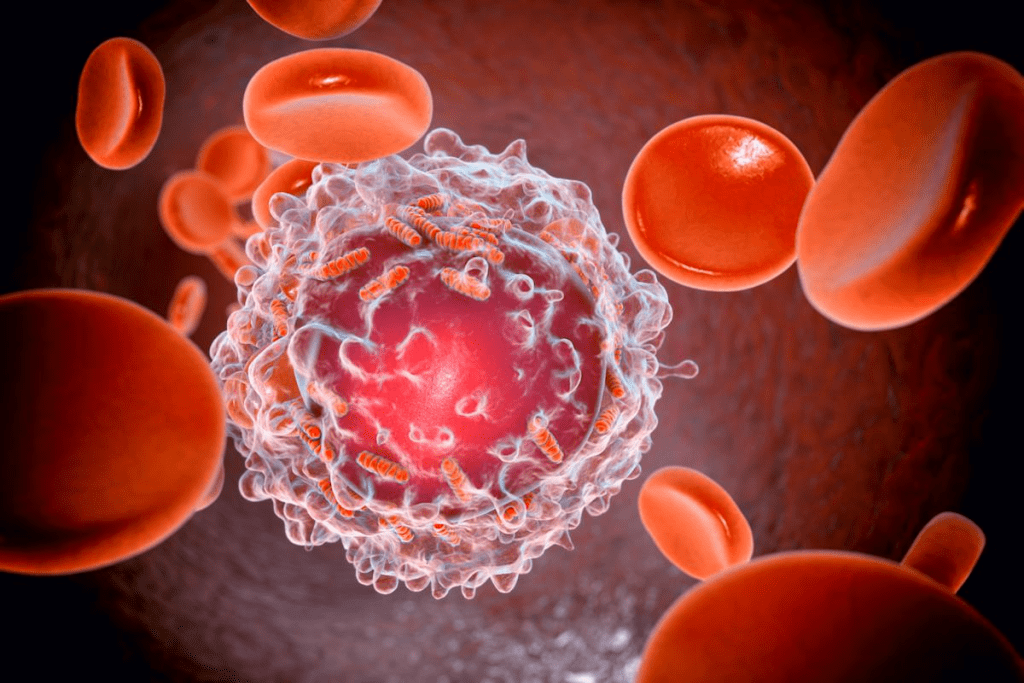
Leukocytosis, or a high white blood cell count, can mean many things. It can show infections, inflammation, or cancer. When it comes to cancer, knowing about a high white blood cell count helps us understand how the body reacts to the disease.
Studies show some cancers are more likely to have high white blood cells. This info is key to taking care of patients and planning their treatment. By grasping the link between leukocytosis and cancer, we can handle diagnosis and treatment better.
Leukocytosis is when you have too many white blood cells. It’s common in people with cancer. We’ll look at what’s normal for white blood cells and how cancer can cause too many.
For adults, a normal white blood cell count is usually under 11,000 per microliter. Knowing what’s normal is key to spotting leukocytosis.
The normal range for WBC count is between 4,500 to 11,000 cells per microliter for adults. But, this can change slightly based on the lab.
Key factors that influence WBC count include:
Cancer can cause too many white blood cells in a few ways. Tumors might make substances that boost white blood cell production. Or, they can cause inflammation, raising WBC counts.
Some cancers are more likely to cause this issue. For example, certain blood cancers directly affect the blood and bone marrow, leading to abnormal counts.
Understanding these causes is important for managing cancer-related leukocytosis. It helps in the overall care of cancer patients.
Leukocytosis, or high white blood cell count, is common in many blood cancers. These cancers affect the blood, bone marrow, and lymphatic system. They can cause an overproduction of white blood cells, seen in blood tests.
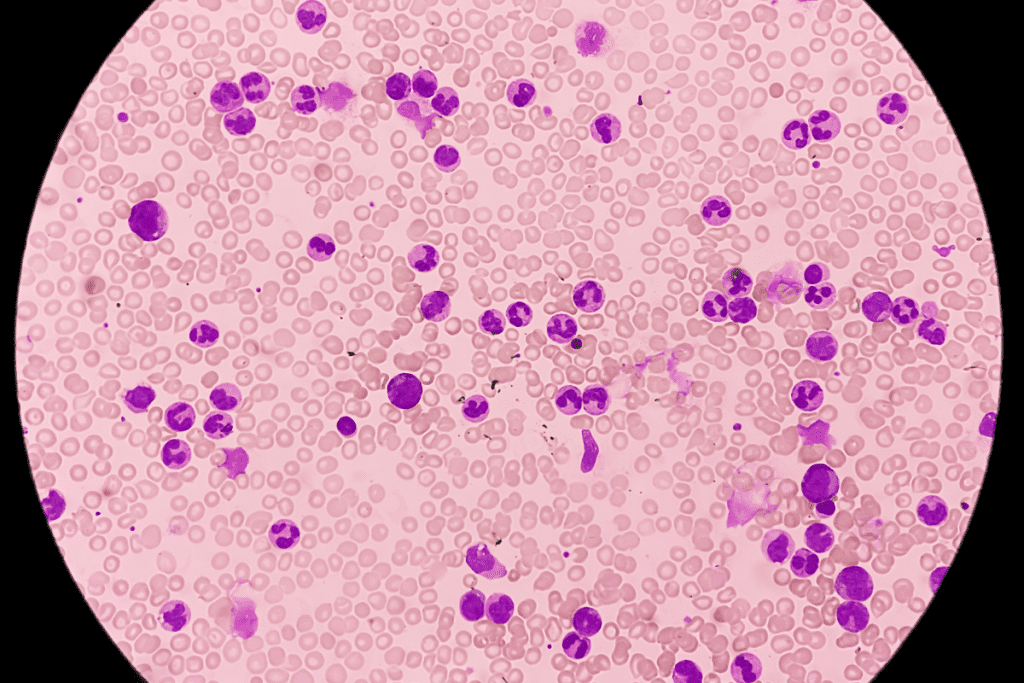
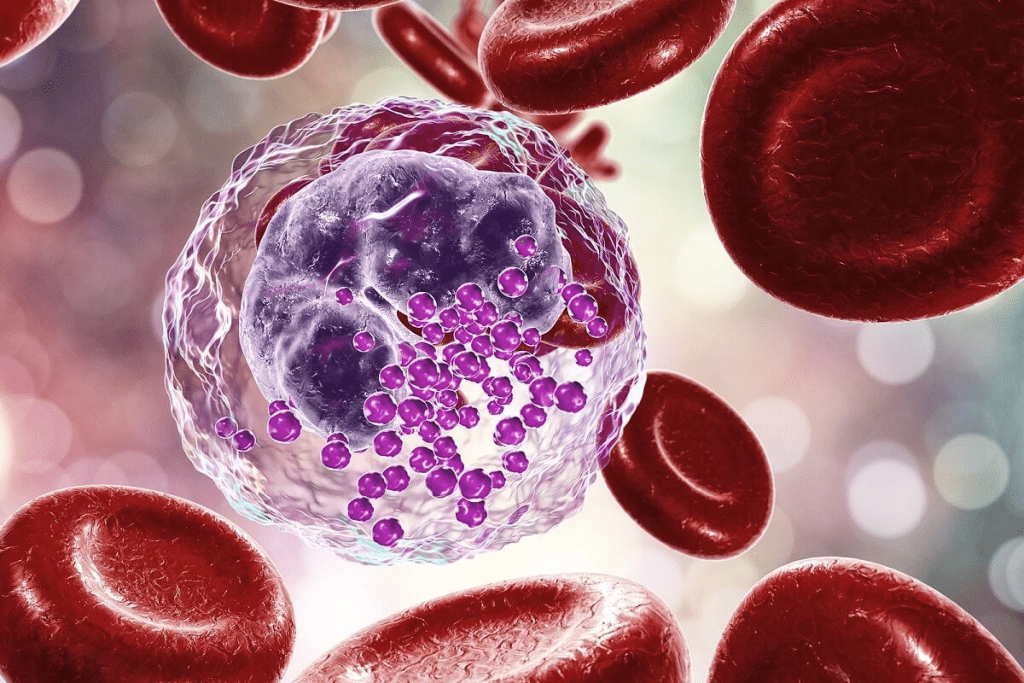
Chronic Lymphocytic Leukemia (CLL) is a blood and bone marrow cancer. It produces too many immature white blood cells. CLL leads to elevated white blood cell counts, causing problems. Studies show it’s key to understand CLL and leukocytosis for better management.
Small Lymphocytic Lymphoma (SLL) is similar to CLL. It mainly affects lymph nodes but can also cause high white blood cell counts. Monitoring WBC counts is part of SLL management.
Other blood cancers like acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) also cause leukocytosis. They need quick diagnosis and treatment to control high white blood cell counts.
In summary, many blood cancers can lead to high white blood cell counts. This affects patient health and treatment plans. It’s vital to understand these conditions for proper care.
Studies have found a strong link between high white blood cell (WBC) counts and lung cancer risk. The UK Biobank study played a big role in this discovery.
The UK Biobank study showed that high WBC counts raise lung cancer risk. This makes WBC counts a possible biomarker for lung cancer risk. The study’s large data and detailed analysis support this finding.
Key findings from the UK Biobank study include:
Lung adenocarcinoma, a type of non-small cell lung cancer, is linked to high WBC counts. Studies show that lung adenocarcinoma patients often have high WBC counts. This suggests an inflammatory role in the disease.
“The inflammatory microenvironment plays a key role in lung adenocarcinoma development and growth.”
Monocyte counts, part of WBC, are markers for lung adenocarcinoma. Research shows that high monocyte counts are linked to worse lung cancer outcomes. This shows why monitoring monocyte levels is key in lung cancer management.
Our analysis of the relationship between lung cancer and elevated WBC counts highlights the complexity of cancer biology. It shows the need for detailed diagnostic methods.
Gastrointestinal cancers, like colorectal and stomach cancer, are linked to leukocytosis. This is when white blood cell counts go up. It’s important because it can mean a worse outcome and a tumor that suppresses the immune system.
Research shows that high white blood cell counts are linked to a worse prognosis in colorectal cancer. This is because it can show an inflammatory response that helps tumors grow and spread. For example, a study by Kim et al. (2020) found that higher WBC counts were linked to more advanced disease and lower survival rates in colorectal cancer patients.
The reasons for this link are complex. Inflammation is key in colorectal cancer development, and high WBC counts show how much inflammation is in the tumor. Also, some cytokines and growth factors from inflammation can help tumors grow.
In stomach cancer, leukocytosis shows the body’s inflammatory response to the tumor. Helicobacter pylori infection, a risk factor for stomach cancer, causes chronic gastritis. This can lead to higher WBC counts. Leukocytosis in stomach cancer patients might mean a more aggressive disease or a bigger tumor burden.
Key findings related to gastrointestinal cancers and leukocytosis include:
Understanding the link between gastrointestinal cancers and leukocytosis helps in finding better treatments. By knowing the meaning of high WBC counts, doctors can better care for patients. This could lead to better survival rates.
Breast and gynecological cancers are linked to high white blood cell counts. This shows a possible connection between inflammation and cancer growth. It’s key to understand how white blood cells react in these cancers.
Research links high white blood cell counts to a higher breast cancer risk. The leukocyte response is vital in the tumor environment. It affects how cancer grows and spreads.
“The presence of leukocytes in the tumor microenvironment can significantly impact the behavior of breast cancer, affecting both treatment response and overall survival.” This highlights the need to study this connection further.
Endometrial cancer, a common gynecological cancer, is also linked to high white blood cell counts. The inflammatory response is thought to play a big role in its development and growth. Studies show that higher WBC counts are linked to more aggressive disease and worse outcomes.
Ovarian and cervical cancers are also linked to changes in white blood cell counts. The role of leukocytes in these cancers is complex. They can fight cancer or help it grow. It’s important to understand how white blood cells react in these cancers to find better treatments.
“The complex interplay between the immune system and gynecological cancers highlights the need for a detailed understanding of leukocyte response in these malignancies.”
By studying the link between high WBC counts and breast and gynecological cancers, we can learn more about these diseases. This knowledge can help improve treatment and outcomes for patients.
Exploring treatment-related causes of leukocytosis shows that many cancer therapies are involved. Leukocytosis, or an elevated white blood cell count, can be a side effect of some treatments.
Cancer treatments aim to kill cancer cells but can harm healthy cells too. This can change white blood cell counts. It’s important to understand these changes to care for patients well.
Chemotherapy is a common cancer treatment. It kills cancer cells but can also affect the bone marrow. This can lead to changes in white blood cell counts, including leukocytosis, according to the clinical observations.
“Chemotherapy-induced leukocytosis is a complex phenomenon that can result from the body’s response to the treatment,” notes a study on chemotherapy’s effects on blood cell counts.
“The inflammation caused by chemotherapy can lead to an increase in white blood cell production.”
Steroid medications are used in cancer treatment to reduce inflammation and manage symptoms. But, they can also increase white blood cell counts. Medical professionals know that steroid-induced leukocytosis is a side effect to watch for in cancer patients.
Using steroid medications can cause white blood cells to move from one pool to another. This can lead to higher WBC counts. This effect usually goes away when the steroid treatment is changed or stopped.
Cancer patients on treatment are more likely to get infections because their immune systems are weak. These infections can cause inflammation and lead to leukocytosis. It’s important to treat infections quickly to avoid more problems.
Other inflammatory complications can come from the cancer or the treatment itself. Keeping an eye on white blood cell counts and fixing any issues is key to caring for cancer patients.
To reduce the risks of leukocytosis, doctors might change treatment plans or give medicines to help white blood cells. Knowing how to increase white blood cells during cancer treatment is important for supporting patients.
Keeping an eye on white blood cell counts is key to understanding cancer risk and how well a patient might do. We’ve looked at different cancers that can cause high leukocyte. These include blood cancers, lung, stomach, breast, and gynecological cancers.
High white blood cell counts can signal cancer’s presence and how it’s growing. For those with cancer, knowing about leukocytosis is essential. It helps in planning their treatment and care.
Healthcare teams can learn a lot by watching white blood cell counts. This is very important for patients with cancers that affect these counts. It also helps when red corpuscles are involved.
As we keep improving in cancer research and treatment, watching white blood cell counts is more important than ever. It’s a big part of caring for cancer patients. It helps doctors give treatments that are just right for each patient.
A high white blood cell count, or leukocytosis, is over 11,000 cells per microliter of blood. Normal counts can vary slightly. But, a count above 11,000 is usually seen as high.
Cancer can raise white blood cell counts in several ways. It can produce cytokines and growth factors. These stimulate the bone marrow to make more white blood cells. Different cancers can affect counts differently.
Many cancers can raise white blood cell counts. This includes CLL and SLL, lung cancer, and cancers of the gut and breast. It also includes endometrial cancer.
Yes, chemotherapy can change white blood cell counts. It can lower counts by suppressing the bone marrow. But, it can also raise counts in recovery or as a reaction to infection.
Steroid medications can increase white blood cell counts. They do this by releasing white blood cells from storage sites. This effect is usually short-lived and goes away when the steroids stop.
Monitoring white blood cell counts is key for cancer patients. It helps check for infection risk, treatment response, and early signs of complications.
A high white blood cell count may mean a worse prognosis in some cancers. The link between WBC counts and prognosis varies. It depends on the cancer type and other factors like inflammation or infection.
Yes, a low white blood cell count, or leukopenia, is a concern for cancer patients. It raises the risk of infections. These can be serious and need quick medical care.
Managing white blood cell counts in cancer patients involves monitoring and preventive measures. It also includes adjusting treatments as needed. This might include medications to boost white blood cell production or treat infections
Tavakkoli, M. (2018). The significance of leukocytosis in malignancies: A review. Blood (Supplement). https://ashpublications.org/blood/article/132/Supplement%201/4944/262048/The-Significance-of-Leukocytosis-in-Malignancies-A ASH Publications
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!