Last Updated on December 3, 2025 by Bilal Hasdemir

Did you know thousands of men have prostate removal surgery each year? The idea of living without a prostate can be scary. It makes people wonder about its impact on health and life quality. Explore the realities of life after a prostatectomy and understand what to expect when living without a prostate gland.
We will look into the role of the prostate gland and what happens when it’s removed. This is important for those thinking about prostatectomy. We’ll share medical facts and personal stories about life without a prostate. This guide aims to help and support those facing this big health choice.
Key Takeaways
- Understanding the role of the prostate gland and its removal’s impact.
- Insights into the medical aspects of living without a prostate.
- Personal experiences and challenges associated with prostate removal.
- Overview of the prostate surgery recovery process.
- Managing side effects after prostatectomy.
- Support and resources for individuals undergoing prostate removal.
Understanding the Prostate Gland and Its Function
The prostate gland is small but very important for men’s health. It affects both urinary and sexual health. We will look at its anatomy, functions, and how it impacts health.
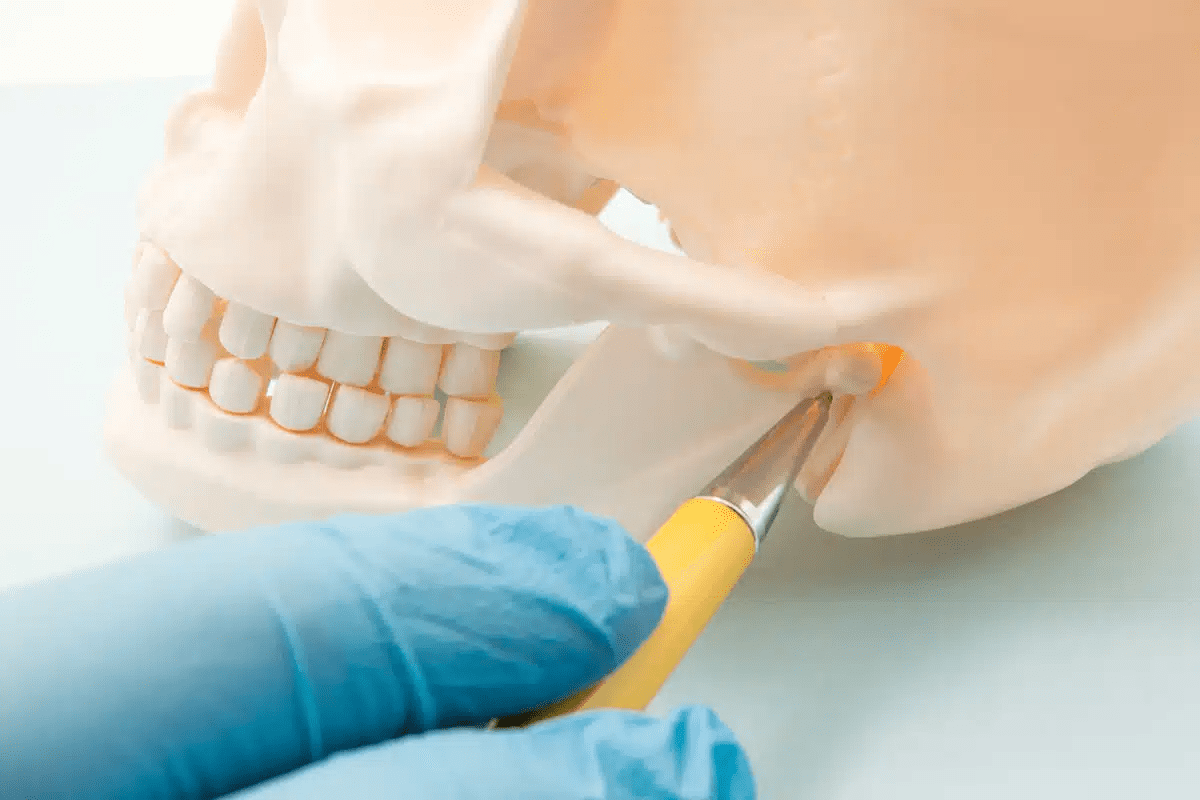
Anatomy and Location of the Prostate
It’s about the size of a walnut and is key to the male reproductive system. Knowing where it is helps us understand its role in health.
Normal Prostate Functions in the Male Body
The prostate gland makes seminal fluid, which helps sperm. This fluid is essential for sperm health and movement. It also helps control urine flow by surrounding the urethra.
How the Prostate Affects Urinary and Sexual Health
The prostate gland greatly affects urinary and sexual health. Its location around the urethra means issues can cause urine problems. It also plays a big role in fertility by producing seminal fluid. Any problems with the prostate can greatly impact a man’s life quality.
What is a Prostatectomy? Definition and Purpose

The term prostatectomy means removing the prostate gland through surgery. This is a big deal in medicine. It’s mainly done to treat prostate cancer and other issues with the prostate.
Medical Definition of Prostatectomy
A prostatectomy is when doctors take out part or all of the prostate gland. This medical definition includes different methods. For example, radical prostatectomy means taking out the whole gland and some nearby tissues.
The goal of this surgery is to get rid of the bad part of the prostate. This helps with problems like prostate cancer, BPH, or other prostate issues.
History of Prostate Removal Surgery
Prostate removal surgery has come a long way. At first, doctors used big cuts to do the surgery.
Now, we have better ways like laparoscopic and robotic-assisted prostatectomy. These methods help patients heal faster and have fewer problems.
When Surgical Intervention Becomes Necessary
Surgery, like radical prostatectomy, is needed when other treatments don’t work. For prostate cancer, surgery is often the first choice.
Severe BPH might also need surgery if medicines and other treatments don’t help.
Deciding to have prostate surgery is a big choice. Doctors carefully consider the patient’s health and how bad the prostate problem is.
Common Reasons for Prostate Removal

Deciding to remove the prostate is often based on health factors. Prostatectomy is considered when certain conditions affect a patient’s life quality or pose serious health risks.
Prostate Cancer as the Primary Indication
Prostate cancer is a common reason for prostate removal. When prostate cancer is found, doctors look at the cancer’s stage, grade, and the patient’s health. Prostatectomy is a definitive treatment that aims to remove the cancerous gland entirely.
In cases where the cancer is localized within the prostate, surgery can be highly effective. We consider various factors, including the patient’s age, health status, and personal preferences, when deciding on prostate removal for cancer treatment.
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia, or BPH, is another significant indication for prostate removal. BPH is a non-cancerous enlargement of the prostate gland that can cause urinary symptoms such as difficulty starting urination, weak urine flow, and frequent urination.
When BPH symptoms are severe and not adequately managed with medications or other treatments, surgical intervention may be necessary. Prostatectomy can provide significant relief from BPH symptoms by removing the enlarged prostate tissue that obstructs urine flow.
Other Medical Conditions Requiring Prostate Surgery
Apart from prostate cancer and BPH, other medical conditions can necessitate prostate removal. These include:
- Prostatitis: Chronic inflammation of the prostate that doesn’t respond to other treatments.
- Prostate stones or calcifications: Hardened deposits within the prostate that can cause pain and other complications.
- Prostatic abscess: A rare but serious condition involving a collection of pus within the prostate.
In some cases, the decision to remove the prostate is made when these conditions cause significant symptoms or complications that cannot be managed through other means.
Understanding the reasons for prostate removal helps patients and healthcare providers make informed decisions about treatment options. We consider the individual patient’s condition, overall health, and personal preferences when evaluating the need for prostate surgery.
Long-Term Recovery After Prostate Removal
After prostate surgery, knowing how to recover is key. The healing journey includes getting back to normal, physical therapy, diet changes, and follow-up visits. These steps help you heal fully.
Timeline for Returning to Normal Activities
How long it takes to get back to normal varies. It depends on your health, age, and if you had any problems. Usually, you can start with light activities a few weeks after surgery.
It’s important to listen to your body and not rush. Healthcare experts say this is vital.
Start with short walks and slowly increase how long and often you walk. Avoid heavy lifting and bending for a while. Also, wait until you feel comfortable before driving and doing other daily tasks.
Physical Therapy and Recommended Exercises
Physical therapy is important for getting better, helping with bladder control and physical function. A physical therapist will give you exercises that fit your needs.
Some good exercises are:
- Kegels to strengthen muscles for bladder control
- Walking or swimming to keep your heart healthy
- Stretching to stay flexible and reduce muscle tightness
Dietary Considerations Post-Surgery
Changing your diet is key after prostate surgery. Eating well helps your body heal and manage side effects.
Focus on:
- Eating fruits, veggies, and whole grains for vitamins and fiber
- Choosing lean proteins like chicken, fish, and beans for healing
- Drinking lots of water, at least eight glasses a day
“A healthy diet is fundamental to recovery. It’s not just about eating to survive, but to thrive during the healing process.” – Nutrition Expert
Follow-up Medical Care Schedule
Regular check-ups are important to track your healing, handle any issues, and adjust treatment if needed. Stick to your doctor’s schedule, which may include:
| Time Post-Surgery | Follow-up Activities |
| 1-2 weeks | Post-operative check-up, removal of catheter |
| 6-12 weeks | Assessment of urinary function, discussion of further treatment options |
| 3-6 months | Evaluation of overall recovery, adjustment of rehabilitation plans as needed |
By following these guidelines, you can recover better, avoid problems, and improve your life quality.
Urinary Function Changes After Prostatectomy
Understanding how prostate removal surgery affects urination is key for recovery. This surgery can change how the body handles urine. Many men face this issue after surgery.
Incontinence: Types, Causes and Prevalence
Urinary incontinence is a common issue after prostate surgery. There are two main types: stress incontinence and urge incontinence. Stress incontinence happens when physical activity causes leakage. Urge incontinence is when you feel a sudden need to urinate.
The reasons for incontinence after prostate surgery are complex. They include damage to the urinary sphincter and nerves. Knowing these reasons helps in managing the condition.
Pelvic Floor Exercises for Urinary Control
Pelvic floor exercises, or Kegels, are key to regaining control over urination. These exercises strengthen muscles that support the bladder and urethra. Starting them early after surgery is recommended.
To do Kegels right, find the right muscles and contract them for a few seconds. Then, slowly release them. Doing this several times a day can improve urinary control.
Products and Techniques for Managing Urinary Issues
There are many products and techniques to manage incontinence. These include absorbent pads, adult diapers, and devices to support continence. Techniques like timed voiding and bladder training also help.
It’s important for patients to try different options to find what works best. Talking to healthcare professionals can help find the right products and techniques.
When to Expect Improvement in Urinary Function
Improvement in urinary function after prostate surgery varies. Some men recover quickly, while others take longer. Generally, noticeable improvements happen within the first year.
Patients should be patient and keep up with pelvic floor exercises. Regular check-ups with healthcare providers are also important to track progress and address concerns.
Sexual Health Following Prostate Removal
Prostate removal surgery can change a man’s sexual health a lot. It can affect how well he can get an erection and his overall sexual well-being. It’s important for men to know about these changes and the treatments available after prostatectomy.
Impact on Erectile Function and Mechanisms
The prostate gland’s removal can harm the nerves and blood vessels around it. This can lead to erectile dysfunction (ED). How much it affects a man depends on the surgery type, his age, and his sexual health before surgery. Doctors use nerve-sparing techniques to reduce damage, but ED is a common issue.
There are many reasons for ED after prostate surgery. Damage to the cavernous nerves, less blood flow, and psychological factors play a part. Penile rehabilitation programs are recommended. They include medicines, devices, and lifestyle changes to help regain erectile function.
Changes in Ejaculation, Fertility, and Orgasm
Prostate removal surgery also changes how men ejaculate. Some men experience dry orgasm, where they ejaculate but no semen comes out. This happens because the prostate and seminal vesicles, which make semen, are removed.
Fertility is also affected, as prostate surgery usually makes a man sterile. The removal of seminal vesicles and possible damage to the ejaculatory ducts are the reasons. Orgasmic function can also change, but many men can have an orgasm, even if it’s not as intense.
Treatment Options for Post-Prostatectomy Sexual Dysfunction
There are many treatment options for sexual problems after prostate surgery. These include:
- Phosphodiesterase type 5 inhibitors (PDE5 inhibitors) to help with erections
- Penile rehabilitation programs with medicines and devices
- Counseling and sex therapy for the mind
- Penile implants for severe ED
Men should talk to their doctor about these options. This helps find the best treatment plan for their specific situation and health.
Hormonal and Metabolic Changes After Prostatectomy
Removing the prostate gland can change hormone and metabolic levels in the body. It’s important to know how these changes affect our health and happiness.
Effect on Testosterone and Other Hormone Levels
Prostatectomy can affect hormone production, including testosterone levels. Studies show the surgery itself might not lower testosterone. But treatments or age at surgery can impact hormone levels. It’s key to watch these changes to catch any problems early.
Other hormones, like estrogen, can also change. This can cause symptoms like hot flashes and changes in body shape.
Potential Symptoms of Hormonal Imbalance
After prostatectomy, hormonal imbalances can cause several symptoms. These include:
- Fatigue and decreased energy levels
- Mood swings and irritability
- Changes in body composition, such as increased fat around the abdomen
- Decreased libido
These symptoms can really affect a patient’s life. It’s important to talk to doctors to find ways to manage them.
Hormone Replacement Therapy Considerations
Hormone replacement therapy (HRT) might be an option for those with big hormonal imbalances. HRT tries to balance hormone levels, easing symptoms and improving life quality. But, choosing HRT needs careful thought, weighing risks and benefits.
Patients should talk to their doctors to see if HRT is right for them.
Metabolic Health Monitoring
Metabolic health is also key after prostatectomy. Hormonal changes can mess with metabolism, causing weight gain or insulin resistance. It’s important to keep an eye on metabolic health, checking blood sugar, cholesterol, and blood pressure.
Living a healthy lifestyle, eating well, and exercising can help with metabolic changes. It’s best to work with doctors to create a plan for good metabolic health.
Psychological Impact of Living Without a Prostate
Men often face emotional and psychological challenges after a prostatectomy. The removal of the prostate gland can deeply affect a man’s mental health. It impacts many areas of his life.
Emotional Challenges Post-Surgery
Men may feel a range of emotions after surgery, like anxiety, depression, and relief. These feelings can be intense. It’s important to acknowledge them to move through recovery well.
Common emotional challenges include:
- Fear of cancer coming back
- Anxiety about losing control of urine
- Concerns about sexual problems
Body Image and Masculinity Concerns
The prostate gland is tied to masculinity. Its removal can make men worry about their body image and masculine identity. This can hurt their self-esteem.
It’s key to talk openly and get support for these feelings.
Relationship and Intimacy Adjustments
Prostatectomy can change relationships, including intimate ones. Men and their partners may face new challenges in sex and closeness. Talking openly and seeking counseling can help.
| Adjustment Areas | Potential Challenges | Support Strategies |
| Sexual Intimacy | Erectile dysfunction, changes in ejaculation | Counseling, sexual therapy, medication |
| Emotional Intimacy | Feelings of inadequacy, anxiety | Open communication, couples therapy |
Support Resources and Counseling Options
Men going through prostatectomy can find many support options. These include therapy, support groups, and online forums.
Available support resources:
- Professional counseling
- Support groups for men post-prostatectomy
- Online forums and communities
We understand the need to tackle the psychological effects of prostatectomy fully. By giving men access to the right support, they can handle the challenges of living without a prostate better.
Daily Life Adjustments After Prostate Removal
Life without a prostate means making big changes. Men must adjust their daily life to deal with urinary and sexual health changes after a prostatectomy.
Practical Tips for Managing Incontinence in Social Settings
Dealing with incontinence after prostate removal is tough. Pelvic floor exercises, like Kegel exercises, can help control urination. Using incontinence products like absorbent pads or adult diapers is also helpful when you’re out.
It’s important to plan ahead. Knowing where restrooms are and having a backup plan can ease anxiety. Drinking less before going out and avoiding caffeinated drinks can also help manage incontinence.
Exercise and Physical Activity Modifications
Exercise is key for health, but some activities might need to change after surgery. High-impact exercises like running or heavy lifting can make incontinence worse. Instead, choose low-impact activities like walking, swimming, or cycling.
Keep doing pelvic floor exercises to help regain bladder control. Listen to your body and don’t push too hard. Start slowly and gradually increase the intensity and duration of your workouts.
Travel Considerations Without a Prostate
Traveling after prostate removal needs some planning. Research your destination to find medical facilities and restrooms. Bringing a portable urination device is useful, even on long trips.
Tell your travel buddies about your situation. They can offer the support you need. Don’t forget to pack extra incontinence supplies and any medications.
Communicating Needs with Partners and Family
Talking openly with partners and family is key after surgery. Share your feelings, needs, and concerns. This helps them understand and support you better.
Counseling or support groups can also help. They offer a place to share experiences and learn from others facing similar challenges.
Long-Term Health Considerations Without a Prostate
Living without a prostate means watching your health closely. After a prostatectomy, it’s important to stay alert to avoid problems. This helps keep you healthy in the long run.
Cancer Surveillance After Prostatectomy
One big worry after removing the prostate is cancer coming back. It’s key to watch for this closely. This means:
- Getting regular PSA tests to check for cancer signs.
- Seeing your doctor often to check your health.
- Maybe getting MRI or CT scans if your doctor thinks it’s needed.
A top urologist says, “Watching your health closely is vital. It helps manage cancer risk and ensures the best care after prostate removal.”
“The goal of cancer surveillance is to detect any recurrence at the earliest stage possible, when it is most treatable.”
- A Urologist
Bone Health and Osteoporosis Risk
Removing the prostate can affect your bones, increasing osteoporosis risk. Hormonal changes can weaken bones. So, it’s important to:
- Eat foods rich in calcium and vitamin D.
- Do exercises that make your bones stronger.
- Get bone density tests to check your bone health.
| Nutritional Element | Recommended Daily Intake | Food Sources |
| Calcium | 1,000-1,200 mg | Dairy products, leafy greens, fortified foods |
| Vitamin D | 600-800 IU | Fatty fish, fortified dairy products, sunlight exposure |
Cardiovascular and Metabolic Implications
Prostate removal might affect your heart and metabolism. It’s important to:
- Check your heart health regularly.
- Live a healthy lifestyle with a good diet and exercise.
- Keep an eye on your blood sugar and cholesterol levels.
Regular Screening Recommendations
After prostate removal, regular health checks are a must. This includes:
- Annual physical exams to check your overall health.
- Tests for heart disease risk.
- Monitoring for metabolic syndrome signs.
By being proactive about your health, you can avoid risks and enjoy a good life after prostate removal.
Alternatives to Complete Prostate Removal
Prostatectomy is a common treatment, but there are other choices. These alternatives can manage prostate issues well and keep quality of life high.
Partial Prostatectomy Options
Partial prostatectomy, or focal therapy, removes only the diseased part of the prostate. This method aims to reduce side effects from removing the whole gland.
- Focal Laser Ablation: A minimally invasive procedure using laser energy to target and destroy cancerous or diseased tissue.
- High-Intensity Focused Ultrasound (HIFU): A non-invasive technique that uses ultrasound waves to heat and destroy targeted tissue.
Radiation Therapy Approaches
Radiation therapy is another option, using high-energy rays to kill cancer cells. There are several types, including:
- External Beam Radiation Therapy (EBRT): Delivers radiation from outside the body, targeting the prostate.
- Brachytherapy: Involves placing radioactive seeds directly into or near the prostate.
Radiation therapy is effective for early-stage prostate cancer.
Active Surveillance for Prostate Conditions
Active surveillance is an option for men with low-risk prostate cancer or other conditions. It involves regular monitoring with PSA tests, biopsies, and imaging studies, without immediate treatment.
It’s best for older patients or those with serious health issues. This approach avoids the side effects of aggressive treatments.
Emerging Focal Therapies
Focal therapies target diseased areas of the prostate while sparing healthy tissue. Some new focal therapies include:
- Cryotherapy: Freezing cancer cells to destroy them.
- Irreversible Electroporation: Using electrical pulses to create permanent pores in cancer cells, leading to their death.
These therapies are being studied in clinical trials to check their safety and effectiveness.
In conclusion, while prostate removal is a common treatment, there are many alternatives. Each has its own benefits and considerations. Patients should talk to their healthcare provider to find the best treatment for their condition.
Conclusion: Quality of Life After Prostate Removal
Men often wonder about their life after prostate removal surgery. Living without a prostate means making changes, but many men stay happy and healthy. We’ve looked at how to recover, manage side effects, and adjust to lifestyle changes.
The life quality after surgery depends on many things. These include how well you recover, your health, and how you feel mentally. Knowing these can help men get ready for life after surgery. Thanks to better medical care, many men see big improvements in their health and happiness.
Living without a prostate requires careful thought and action. Being well-informed and proactive helps men enjoy life. Our aim is to offer full support and care to help men live well after prostate removal.
FAQ
What is a prostatectomy?
A prostatectomy is a surgery to remove part or all of the prostate gland. It’s often done to treat prostate cancer or other prostate issues.
Can you live without a prostate?
Yes, living without a prostate is possible. But, you might face side effects like trouble controlling urine and sexual problems. You’ll also need to make some lifestyle changes.
What are the common reasons for prostate removal?
Prostate removal is usually needed for prostate cancer, BPH, or other issues that affect your quality of life or health.
How long does it take to recover from prostate surgery?
Recovery time varies, but it usually takes weeks to months to get back to normal. Physical therapy and follow-up care are key to a smooth recovery.
What are the possible side effects of prostate removal?
Side effects can include trouble controlling urine, erectile dysfunction, changes in ejaculation, and hormonal imbalances. Managing these often requires medical treatment, lifestyle changes, and support.
How can urinary incontinence be managed after prostatectomy?
Managing urinary incontinence involves pelvic floor exercises, using incontinence products, and timed voiding. Improvement in urine control can happen over time, but it varies for everyone.
Are there treatment options for sexual dysfunction after prostate removal?
Yes, there are treatments for sexual dysfunction. These include medications, counseling, and other therapies to help with erectile dysfunction and other sexual health issues.
What are the alternatives to complete prostate removal?
Alternatives include partial prostatectomy, radiation therapy, active surveillance, and focal therapies. The best option depends on your condition, its severity, and your health.
How does prostate removal affect hormonal and metabolic health?
Prostate removal can change hormone levels, including testosterone. This might affect metabolic health. It’s important to monitor and manage these changes for your overall health.
What lifestyle adjustments are necessary after prostate removal?
Adjustments may include managing incontinence, changing exercise routines, and planning travel. It’s also important to communicate with your partner and family to maintain relationships and intimacy.
What are the long-term health considerations after prostate removal?
Long-term, you’ll need to watch for ongoing cancer, bone health, and cardiovascular and metabolic issues. Regular health screenings are key to maintaining your well-being.
References
- InformedHealth.org. (2022, September 14). In brief: How does the prostate work? German Institute for Quality and Efficiency in Health Care. https://www.ncbi.nlm.nih.gov/books/NBK279291