Last Updated on November 13, 2025 by
Knowing life expectancy after a stem cell transplant is key for those thinking about it. The outcome depends on several things. These include the disease, the patient’s health, and the transplant type.
Recent studies show good stem cell transplant survival statistics. For some blood cancers, the success rate is 60-70%. In children, over 90% survive the first year. Better medical tech and care have greatly helped patients.

We’ll dive into these factors, giving insights into survival rates. The life expectancy after a bone marrow transplant can vary. But, with the right care, many patients see big improvements.
Key Takeaways
- Life expectancy after stem cell transplant depends on multiple factors.
- Recent studies show a 60-70% success rate for certain blood cancers.
- Children have shown over 90% one-year survival rates.
- Advances in medical technology have improved patient outcomes.
- Comprehensive care is key for stem cell transplant patients.
- Survival rates vary based on the disease and the patient’s health.
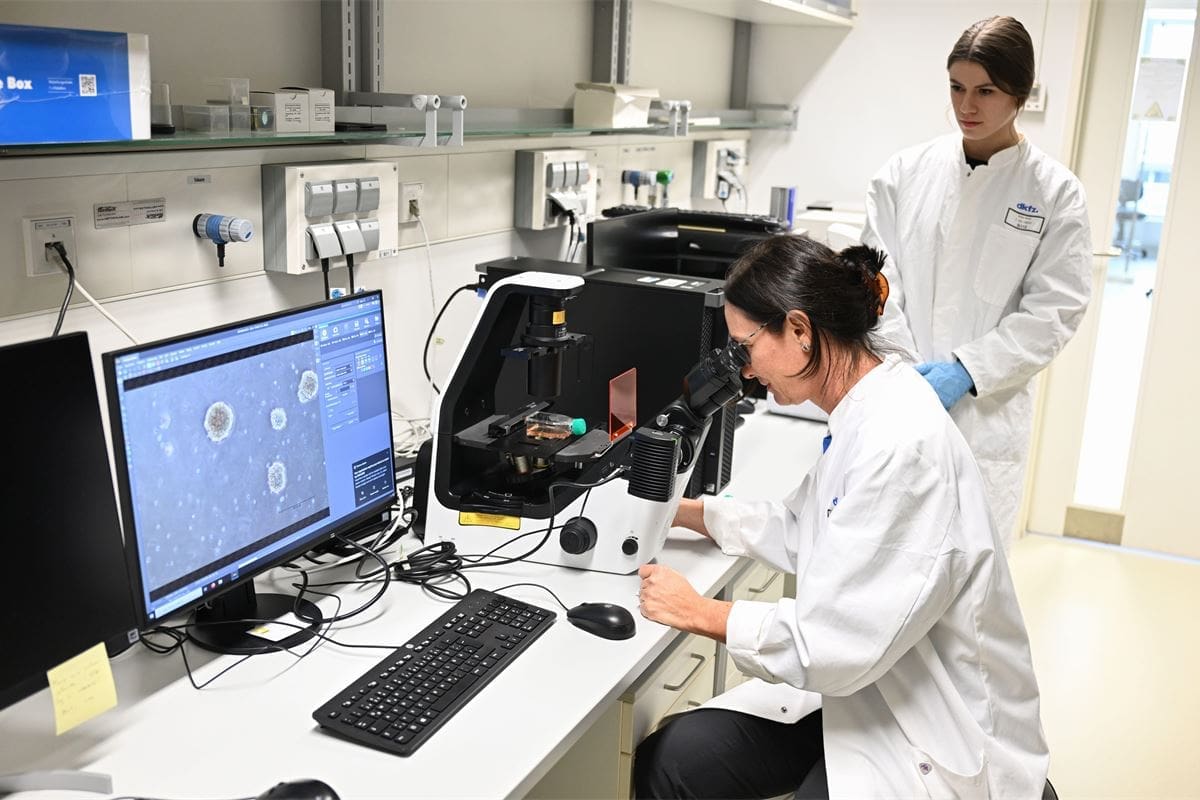
Understanding Stem Cell Transplants
Stem cell transplants, also known as bone marrow transplants, are key to treating many diseases. They replace damaged stem cells with healthy ones. This can come from the patient themselves or a donor.
Types of Stem Cell Transplants
There are two main types: autologous and allogeneic. Autologous transplants use the patient’s own stem cells. These are collected, stored, and then given back after treatment.
Allogeneic transplants use stem cells from a donor. This can be a family member or someone else. These cells are usually taken from bone marrow or blood. Allogeneic transplants are used for leukemia and other blood disorders.
- Autologous transplants: Using the patient’s own stem cells.
- Allogeneic transplants: Using stem cells from a donor.
The Transplantation Process
The process starts with conditioning therapy. This is usually chemotherapy and/or radiation. It gets rid of the patient’s sick cells and weakens their immune system.
Then, the patient gets the stem cell infusion. It’s like a blood transfusion. The new stem cells go to the bone marrow and start making new blood cells.
- Conditioning therapy to prepare the patient’s body.
- Stem cell infusion.
- Recovery and monitoring post-transplant.
Every patient’s journey with stem cell transplants is different. The details of the process depend on the patient’s health and the disease being treated.
Factors Affecting Life Expectancy After Stem Cell Transplant
It’s important to know what affects life expectancy after a stem cell transplant. Many factors play a big role in how well a transplant works and how long a person lives.
Underlying Disease and Condition
The disease a person has before the transplant matters a lot. Those with diseases in remission or well-controlled usually do better. The type of disease, its stage, and how it responds to the transplant are critical factors that influence overall survival.
Patient Age and Overall Health
Age and health also play a big part in life expectancy after a transplant. Older patients or those with significant comorbidities might face higher risks and lower life expectancy. We carefully assess these factors to give personalized care.

Donor Compatibility
In allogeneic transplants, finding a compatible donor is key. A well-matched donor lowers the risk of graft-versus-host disease (GVHD) and other problems. We use advanced matching techniques to find the best donors for our patients.
Post-Transplant Care
The care a person gets after the transplant is very important. Good follow-up care, including watching for complications and managing side effects, is essential. Our multidisciplinary teams work closely with patients to provide the support and care they need, improving their quality of life and survival.
Overall Survival Statistics
Stem cell transplant survival rates have greatly improved over time. This gives hope to those with blood cancers. For blood cancers, stem cell transplants now have a 60-70% success rate. This boost comes from better technology, care, and treatment plans.
Short-Term Survival Rates
Adults and children are living longer after stem cell transplants. Adults now have over 80% one-year survival rates. Children do even better, with rates over 90%. These numbers show how far stem cell transplant techniques and care have come.
- Adult one-year survival rates: over 80%
- Children’s one-year survival rates: over 90%
- Significant improvement in short-term survival due to better treatment protocols
Long-Term Survival Rates
Long-term survival after stem cell transplant is also getting better. Many factors affect long-term survival, like the disease, age, and health. Research shows that survival rates are improving as treatments get better.
A study by the American Association for Cancer Research shows better outcomes for elderly patients with acute myeloid leukemia.
Trends in Survival Improvement
Survival rates are improving for many reasons. Better conditioning regimens, care, and new treatments are key. As research keeps advancing, we expect even better survival rates for stem cell transplant patients.
- Advancements in conditioning regimens
- Improved supportive care
- Novel therapeutic approaches
In summary, survival rates for stem cell transplant patients are looking up. We see big improvements in both short-term and long-term survival. As we keep working on treatments and care, the future looks brighter for these patients.
Life Expectancy After Stem Cell Transplant for Blood Cancers
Stem cell transplants have changed how we treat blood cancers like leukemia, multiple myeloma, and lymphoma. They can help patients live longer. Blood cancers often need stem cell transplants, and these treatments have made a big difference.
Leukemia Survival Rates
Leukemia patients who get stem cell transplants have better chances of survival. Advances in transplant techniques and post-transplant care have helped a lot. The five-year survival rate for these patients can be between 40% to 60%.
This depends on the disease stage and how well the donor’s cells match the patient’s.
Multiple Myeloma Outcomes
Stem cell transplants are now a key treatment for multiple myeloma. These patients are living longer, with some studies showing a median overall survival of 6 to 10 years after the transplant. Several factors affect these outcomes, including the patient’s age and how well they respond to initial treatments.
Hodgkin Lymphoma Success Rates
Hodgkin lymphoma patients who get stem cell transplants, often those with relapsed or refractory disease, have success rates. The long-term survival for these patients can be from 50% to 70%. This depends on the disease stage at diagnosis and how well they responded to previous treatments.
Non-Hodgkin Lymphoma Outcomes
Non-Hodgkin lymphoma is a group of lymphoid malignancies with different outcomes based on the subtype. Generally, patients with certain subtypes have good response rates to stem cell transplants. Some studies show five-year overall survival rates ranging from 40% to 70%.
Overall, patients with blood cancers are living longer after stem cell transplants. This shows how far medical care and transplant technology have come.
Autologous vs. Allogeneic Transplant Outcomes
When we compare autologous and allogeneic stem cell transplants, we see big differences. These include success rates, risks, and how each transplant works for different diseases. Patients and doctors must think about these points when choosing a transplant.
Comparing Success Rates
Success rates for these transplants depend on many things. This includes the disease, the patient’s health, and if the donor is a good match. Autologous transplants use the patient’s own stem cells. They have fewer risks of problems like GVHD.
Allogeneic transplants use donor stem cells. They can fight cancer better, which is good for some cancers.
- Autologous transplants are often chosen for multiple myeloma and some lymphomas.
- Allogeneic transplants are usually for acute leukemias and diseases where fighting cancer is key.
- Both types of transplants have gotten better over time thanks to new care and techniques.
Risk Profiles and Complications
The risks for autologous and allogeneic transplants are different. Autologous transplants have less GVHD risk but might see cancer come back more often. Allogeneic transplants have a GVHD risk but can fight cancer, which might lower the chance of cancer coming back.
- Graft-versus-host disease is a big worry for allogeneic transplants. It needs careful donor matching and care after the transplant.
- Both types face infection risks, but how fast the immune system recovers can vary.
- There’s also a risk of getting another cancer later for both types of transplant patients.
Disease-Specific Considerations
When picking between autologous and allogeneic transplants, the disease matters a lot. For example, some lymphomas or multiple myelomas might do better with autologous transplants. But, acute leukemia patients might do better with allogeneic transplants.
It’s key for patients to talk with their healthcare team about their situation. This helps decide the best transplant type for their disease, health, and other factors.

Pediatric Stem Cell Transplant Survival Rates
The field of stem cell transplants for kids has grown a lot. Now, more kids survive and live better lives after these treatments. Thanks to new medical tech and better care, kids are doing much better than before.
Children’s Outcomes vs. Adults
Research shows kids usually do better than adults after stem cell transplants. This is because kids’ immune systems are stronger and they’re generally healthier.
Several things help kids do well:
- Fewer comorbidities: Kids usually don’t have as many health problems as adults, which lowers the risk of bad side effects.
- Better donor matches: When kids get transplants, they often get them from siblings. This means a better match and less chance of problems.
- Improved supportive care: New ways to care for kids after transplants have made a big difference in managing problems.
One-Year Survival Statistics
Recent numbers from top transplant centers show that over 90% of kids survive a year after a transplant. This is a big jump from before and shows how far we’ve come in transplant tech and care.
A study in a top medical journal found:
- The one-year survival rate for kids was 92%.
- Kids with certain diseases, like leukemia, did even better, with a 95% survival rate.
Long-Term Quality of Life
It’s important to think about how well kids do long-term after a transplant. Studies show many kids live active, healthy lives. Some key points are:
- More than 80% of kids who survive long-term don’t have big health problems.
- Many kids can go back to school and sports within a year or two after their transplant.
As we keep improving in stem cell transplants, we expect even better results for kids. This brings hope to families and kids facing these tough conditions.
Racial and Ethnic Disparities in Transplant Outcomes
Stem cell transplants have made great strides, yet racial and ethnic disparities in outcomes remain. These disparities stem from many factors. These include genetic differences, socio-economic status, access to healthcare, and the quality of care.
Current Disparities
Research shows that racial and ethnic minorities face lower survival rates and higher complication rates after stem cell transplants. For example, African Americans and Hispanics/Latinos are at a higher risk of graft-versus-host disease (GVHD), a serious complication.
“The disparity in transplant outcomes among different racial and ethnic groups is a significant concern that warrants further investigation and action,” as noted by experts in the field.
Factors Contributing to Differences
Several factors lead to the disparities in transplant outcomes. These include:
- Genetic differences that may affect the compatibility between donors and recipients.
- Socio-economic factors, such as access to healthcare and the ability to afford post-transplant care.
- Differences in the quality of care received, with minorities potentially having less access to high-quality transplant centers.
- Cultural and linguistic barriers that may impact patient understanding and adherence to treatment plans.
Efforts to Improve Equity
To tackle these disparities, the medical community is making strides. Efforts include:
- Increasing diversity among stem cell donors to improve the chances of finding compatible matches for minority patients.
- Implementing culturally sensitive care practices to better meet the needs of diverse patient populations.
- Enhancing patient education and support to improve understanding and adherence to treatment plans.
- Conducting research into the genetic and biological factors that contribute to disparities in transplant outcomes.
By acknowledging and addressing these disparities, we can strive for more equitable outcomes for all patients undergoing stem cell transplants.
Post-Transplant Complications and Their Impact on Survival
Surviving a stem cell transplant is just the beginning. Managing complications after the transplant is key for long-term survival. Patients often face many challenges that can affect their quality of life and life expectancy. We will look at common complications and their impact on patient outcomes.
Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big problem after an allogeneic stem cell transplant. The donated stem cells see the recipient’s body as foreign and attack it. GVHD can be acute or chronic, happening months or years after the transplant. GVHD management uses immunosuppressive drugs to control the graft’s immune response.
Acute GVHD happens within the first 100 days and can affect the skin, liver, and gut. Symptoms range from mild to severe, including rash, nausea, and abdominal pain. Chronic GVHD can cause skin changes, dry eyes and mouth, and liver problems.
Infections and Immune System Recovery
Infections are a big risk after stem cell transplantation because of the immunosuppressive treatments. It takes months to a year or more for the immune system to recover. During this time, patients are at high risk of viral, bacterial, and fungal infections. Prophylactic measures, like antimicrobial drugs, are used to prevent infections.
Viral infections, like CMV reactivation, are a big concern. Regular monitoring and preemptive treatment can help manage these risks. Bacterial infections can happen due to low white blood cell count, and fungal infections, though rare, can be severe.
Secondary Malignancies
Secondary malignancies are a long-term risk of stem cell transplantation. The risk depends on the conditioning regimen, radiation or chemotherapy exposure, and GVHD presence. Long-term follow-up is key to catch secondary cancers early.
Managing Long-Term Side Effects
Managing long-term side effects is vital for improving the quality of life and survival of stem cell transplant recipients. Side effects can include organ dysfunction, hormonal imbalances, and psychological issues. A detailed follow-up care plan is needed, involving a team of healthcare providers.
Patients and their caregivers need to know about long-term complications and the importance of follow-up care. This includes regular check-ups, monitoring for late effects, and interventions to reduce these effects when possible.
Quality of Life After Stem Cell Transplant
Life after a stem cell transplant is different for everyone. It depends on the transplant type and the patient’s health. Recovery is not just about getting better physically. It also involves the mind and emotions.
Physical Recovery Timeline
Recovery time after a stem cell transplant varies. Patients might start feeling better in weeks or months. But, it can take up to a year or more to fully recover. This depends on the patient’s health and the transplant type.
Key milestones in physical recovery include:
- Regaining strength and energy
- Recovery of blood counts
- Healing of any transplant-related complications
Patients need to follow their doctor’s advice. They should also go to follow-up appointments to check their progress.
Psychological and Emotional Aspects
The mental and emotional journey after a transplant is as important as physical recovery. Patients may feel many emotions, like relief, gratitude, anxiety, or depression. Support from loved ones and mental health experts is key in dealing with these feelings.
Some patients might need counselling or therapy to handle their emotions. Doing things that bring joy and practicing stress reduction can help too.
Returning to Normal Activities
Getting back to normal activities is a big part of recovery. The time it takes varies, but many can start their daily routines again in a few months. It’s important to listen to your body and not push too hard, as this can cause setbacks.
Long-Term Survivors’ Experiences
People who survive for a long time after a transplant often feel grateful and resilient. They might face long-term side effects, but many live active and meaningful lives. Thanks to medical progress and supportive care, their outlook is improving.
Understanding the different aspects of life after a transplant helps patients and their families prepare. It also helps them make informed decisions about their care.
Advances Improving Transplant Outcomes
The field of stem cell transplantation is always changing. This is thanks to new medical research and technology. New ways to prepare patients, better care, and new treatments are making transplants safer and more successful.
New Conditioning Regimens
Conditioning regimens are key in stem cell transplants. They clear out the old bone marrow for new cells. Now, we have new ways to do this that are less harsh but just as effective.
Reduced-intensity conditioning (RIC) is one such method. It’s gentler, making it better for older patients or those with health issues.
RIC uses less chemotherapy and radiation. This means fewer side effects and quicker recovery times. Research shows it works as well as older methods in some cases, with fewer risks.
Improved Supportive Care
Supportive care is essential for transplant success. It helps prevent and treat problems like infections and organ damage. Thanks to new advances, transplants are now safer and more effective.
For instance, antimicrobial prophylaxis is now common to fight off infections. Also, better treatments for graft-versus-host disease (GVHD) have made it less common and severe.
Novel Therapeutic Approaches
New treatments are also pushing the field forward. CAR-T cell therapy is one example. It’s showing great promise in fighting certain blood cancers.
Research into regenerative medicine is also exciting. It involves using stem cells to repair tissues and boost the immune system. This could lead to new transplant treatments in the future.
Research Directions
There are many areas of research in stem cell transplantation. We’re working on making conditioning regimens safer and more precise. We’re also exploring new ways to use stem cells and other therapies.
Personalized medicine is another big area. It aims to tailor treatments to each patient’s needs. This could lead to even better results and fewer side effects.
Choosing a High-Quality Transplant Center
Finding the right transplant center is key for those getting stem cell transplants. The care you get before, during, and after the transplant greatly affects your outcome and life quality.
Key Factors to Consider
When looking at transplant centers, several important factors come into play. Experience and expertise in stem cell transplants are essential. Centers that do many transplants tend to have better results.
- The qualifications and experience of the medical team
- The availability of advanced technology and treatment options
- The quality of supportive care services, including nursing and counselling
- Accreditation and certification from reputable organizations
It’s also important for the center to offer comprehensive care. This means they take care of your medical, psychological, and emotional needs.
Questions to Ask Your Healthcare Team
Patients should ask their healthcare team about the transplant center. Key questions include:
- What is the center’s success rate for stem cell transplants?
- How does the center handle complications or emergencies?
- What kind of follow-up care is provided after the transplant?
- Are there any support services available for patients and their families?
The Role of Comprehensive Care
Comprehensive care is more than just medical treatment. It includes support services for recovery and rehabilitation. A top-notch transplant center should offer nutritional counselling, psychological support, and physical therapy. These help patients regain strength and adjust to life after transplant.
Center-Specific Survival Rates
Survival rates are a key measure of a transplant center’s quality. Look for centers that openly share their outcomes and survival rates. Center-specific survival rates give insight into how well the center handles different cases and complications.
By carefully looking at these factors and asking the right questions, patients can make smart choices. They can pick a transplant center that fits their needs.
Conclusion
Life expectancy after a stem cell transplant has greatly improved. This is thanks to new medical technologies and better care. We’ve looked at what affects life expectancy, like the disease, the patient’s age, and the match with the donor.
Knowing these factors is key for patients, their families, and doctors. It helps everyone make better choices.
Survival rates for stem cell transplants are getting better, thanks to progress in treating blood cancers. The type of transplant also matters a lot. As research keeps moving forward, we’ll see even better survival rates.
Patients can improve their chances of a good outcome by staying up-to-date with the latest in stem cell transplants. It’s vital to pick a top-notch transplant center. This way, patients can live longer and better lives.
FAQ’s:
What is the life expectancy after a stem cell transplant?
How do different types of stem cell transplants affect life expectancy?
What factors influence life expectancy after a stem cell transplant?
What are the current survival statistics for stem cell transplant patients?
How does the underlying disease affect life expectancy after a stem cell transplant?
What is the difference in survival rates between autologous and allogeneic stem cell transplants?
How do stem cell transplants in children compare to those in adults in terms of survival rates?
What are the common post-transplant complications that can impact survival?
How does the quality of life change after a stem cell transplant?
What advances are improving transplant outcomes?
How can patients choose a high-quality transplant center?
Does donating bone marrow shorten your life?
What is the life expectancy after a bone marrow transplant for leukemia?
What are the stem cell transplant survival statistics?
How long does a bone marrow transplant last?
References
- Cancer Research UK. (2025). Phases of treatment for acute lymphoblastic leukaemia (ALL). https://www.cancerresearchuk.org/about-cancer/acute-lymphoblastic-leukaemia-all/treatment/phases
- National Cancer Institute. (2025). Acute lymphoblastic leukemia treatment (PDQ ®). https://www.cancer.gov/types/leukemia/patient/adult-all-treatment-pdq
- StatPearls. (2024). Acute myeloid leukemia. https://www.ncbi.nlm.nih.gov/books/NBK507875/