Last Updated on December 1, 2025 by Bilal Hasdemir
Nearly 30% of cancer patients get brain metastases. This greatly affects their life expectancy and life quality. For many, whole brain radiation therapy (WBRT) is a common treatment.
Knowing the life expectancy after whole brain radiation is key. It helps patients and their families make better care choices.
We will look at what affects whole brain radiation therapy outcomes and brain metastases life expectancy with treatment. Our goal is to give a detailed guide to help patients through this tough time.
Key Takeaways
- WBRT is a common treatment for brain metastases, affecting life expectancy.
- Several factors influence life expectancy after WBRT.
- Understanding treatment outcomes is key for patient care.
- Personalized support is vital for patients undergoing WBRT.
- Life expectancy varies a lot among patients with brain metastases.
Understanding Whole Brain Radiation Therapy
Whole Brain Radiation Therapy (WBRT) is a key treatment for brain metastases. It offers a full approach to manage the disease. WBRT controls tumor growth and relieves symptoms.
Definition and Purpose
WBRT is a radiation therapy that targets the whole brain. Its main goal is to control cancer cells in the brain. This is important because treating the whole brain helps manage multiple metastases.
When WBRT is Recommended
WBRT is suggested for patients with many brain metastases or large tumors. It’s also recommended for those with symptoms from brain metastases. The choice to have WBRT depends on several factors.
These include the cancer type and stage, the number and location of brain metastases, and the patient’s health.
WBRT is often advised in these situations:
- Multiple brain metastases
- Large brain tumors causing significant symptoms
- Presence of extracranial disease
- Poor performance status, making surgical intervention challenging
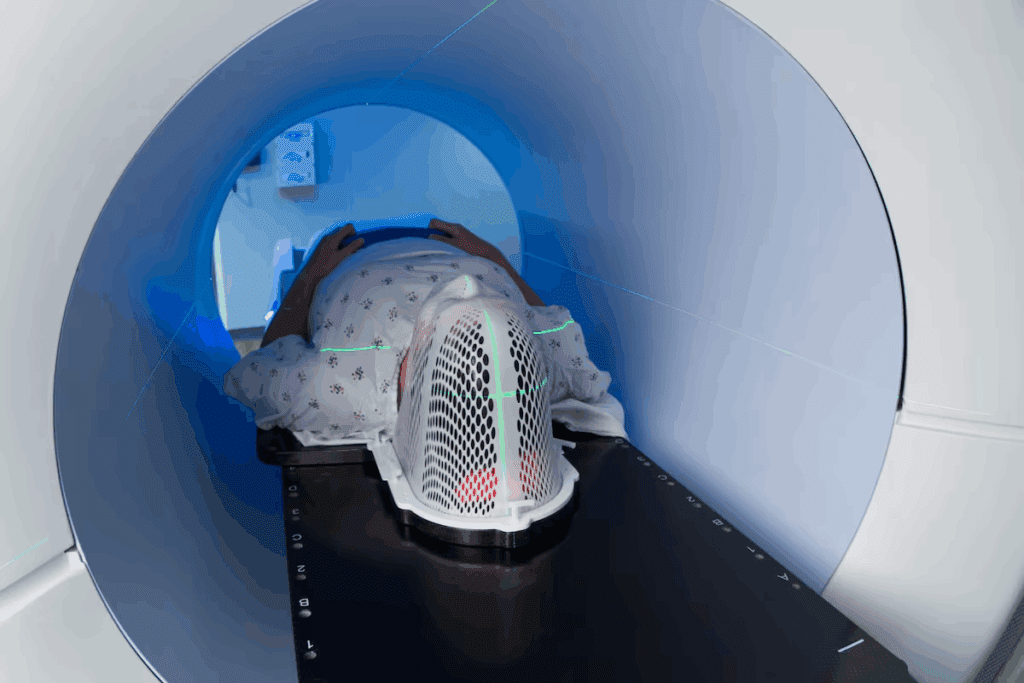
How the Treatment is Administered
WBRT uses a linear accelerator to deliver precise radiation to the brain. The treatment involves several steps:
- Simulation: The patient undergoes a simulation session to determine the exact area to be treated.
- Planning: A radiation oncologist creates a personalized treatment plan.
- Treatment Delivery: The patient receives WBRT, usually in fractions over several sessions.
Understanding WBRT helps patients and families deal with brain metastases treatment. It’s important to talk about the benefits and side effects with a healthcare provider. This way, they can make informed decisions.
Brain Metastases: The Primary Reason for WBRT
Brain metastases are a big challenge in cancer treatment. They often need Whole Brain Radiation Therapy (WBRT) to help patients. This makes treatment more complex and often involves many doctors.
Common Primary Cancers That Spread to the Brain
Some cancers are more likely to spread to the brain. These include:
- Breast cancer, specially HER2-positive and triple-negative types
- Non-small cell lung cancer (NSCLC), a big cause of brain metastases
- Melanoma, known for its aggressive nature and high rate of brain metastasis
- Renal cell carcinoma, which can also spread to the brain, though less often
Knowing the type of cancer is key to understanding the patient’s outlook and treatment.
How Brain Metastases Affect Prognosis
Brain metastases usually mean a worse outlook for cancer patients. The outlook depends on several things. These include the number and location of metastases, the type of cancer, and the patient’s health.
| Primary Cancer Type | Median Survival After Brain Metastasis Diagnosis |
| Breast Cancer | 12-18 months |
| Non-Small Cell Lung Cancer | 6-12 months |
| Melanoma | 4-6 months |
Types of Brain Metastases
Brain metastases can be single or multiple. Their location in the brain affects treatment choices and outlook.
Symptomatic vs. Asymptomatic Metastases: Some metastases cause symptoms like headaches or seizures. Others are found by chance during imaging.
Knowing the details of brain metastases is vital for planning treatment. This might include WBRT, surgery, or other treatments.
Life Expectancy After Whole Brain Radiation: Statistical Overview
Whole brain radiation therapy is a common treatment for brain metastases. It’s important for patients and healthcare providers to understand its impact on life expectancy. Statistical overviews offer valuable insights into patient prognosis.
Median Survival Rates
Median survival rates after whole brain radiation therapy vary. Factors like the type and stage of the primary cancer, the number and location of brain metastases, and the patient’s overall health status play a role. Generally, the median survival rate ranges from 3 to 6 months, but it can be longer for some patients.
For instance, patients with a single brain metastasis and controlled extracranial disease may have a median survival of up to 7 months. Those with multiple brain metastases and uncontrolled extracranial disease may have a median survival of around 2-3 months.
One-Year and Two-Year Survival Statistics
One-year and two-year survival statistics offer further insight into patient prognosis. Studies show that the one-year survival rate for patients with brain metastases treated with WBRT ranges from 10% to 20%. The two-year survival rate is generally less than 10%.
But, certain subgroups of patients may have more favorable outcomes. For example, patients with breast cancer or non-small cell lung cancer (NSCLC) brain metastases may have one-year survival rates of up to 30-40% following WBRT.
Interpreting Survival Data Appropriately
Interpreting survival data requires careful consideration of various factors. These include the patient population, treatment specifics, and study methodologies. It’s essential to understand that survival statistics are based on averages and may not accurately predict individual patient outcomes.
Survival data should be interpreted in the context of the patient’s overall health status, the type and stage of the primary cancer, and the presence of other comorbidities. This approach helps healthcare providers and patients make informed decisions about treatment options.
Differences Between Primary and Metastatic Brain Tumors
Primary brain tumors originate in the brain, whereas metastatic brain tumors arise from cancers that have spread to the brain from other parts of the body. The prognosis and treatment outcomes for these two types of brain tumors differ significantly.
| Characteristics | Primary Brain Tumors | Metastatic Brain Tumors |
| Origin | Arise from brain tissue | Spread from other cancers |
| Prognosis | Varies based on tumor type and grade | Generally poorer due to systemic disease |
| Treatment Approach | Surgery, radiation, chemotherapy | Whole brain radiation, SRS, systemic therapy |
Understanding these differences is key to developing effective treatment plans and improving patient outcomes.
Key Factors Affecting Survival After WBRT
WBRT’s success depends on several key factors that greatly affect survival rates. Knowing these factors is key to predicting outcomes and creating a treatment plan that fits each patient.
Primary Cancer Type and Stage
The type and stage of the primary cancer are very important for survival after WBRT. Different cancers spread to the brain and react to radiation therapy in different ways. For example, breast cancer or lung cancer patients might have different outcomes than those with melanoma or other cancers.
Primary cancer type and its biological traits greatly influence how well it responds to WBRT. The cancer’s stage at diagnosis also matters, as more advanced cancers often have a worse prognosis.
Number and Location of Brain Metastases
The number and location of brain metastases are key to survival after WBRT. Patients with fewer metastases usually do better than those with many. Also, where these metastases are in the brain can affect treatment success and quality of life.
Patient’s Overall Health Status (KPS Score)
A patient’s overall health, measured by the Karnofsky Performance Status (KPS) score, is a big predictor of survival after WBRT. The KPS score looks at a patient’s daily activities and overall function. Patients with higher KPS scores tend to live longer.
The KPS score is a valuable tool for doctors to assess a patient’s prognosis and make informed care decisions.
Age and Comorbidities
Age and comorbidities also play a big role in survival after WBRT. Older patients or those with many health issues may face a tougher time due to less physical strength and more side effects from treatment.
Understanding these factors helps doctors create treatment plans that are best for each patient. This aims to improve survival chances and quality of life.
Prognostic Scoring Systems for Brain Metastases
Several scoring systems help predict outcomes for patients with brain metastases. These tools help doctors and patients understand the disease’s likely path. They aid in making informed treatment choices.
RPA Classification
The Recursive Partitioning Analysis (RPA) classification is a well-known system. It sorts patients into three groups based on age, Karnofsky Performance Status (KPS), and extracranial disease presence.
This system offers a simple way to gauge prognosis. Class 1 has the best outlook, while Class 3 faces the worst.
GPA Scoring System
The Graded Prognostic Assessment (GPA) scoring system is also widely used. It considers age, KPS, brain metastasis number, and extracranial metastases. This gives a more detailed prognosis.
The GPA score ranges from 0 to 4. Higher scores mean a better prognosis. It’s effective in predicting survival for brain metastasis patients.
Disease-Specific GPA Scores
Disease-specific GPA scores are tailored for different cancers. For instance, the breast-GPA and lung-GPA scores focus on specific factors for breast and lung cancer.
These scores offer a more personalized prognosis. They help in planning treatments that fit individual needs.
How Doctors Use These Systems for Treatment Planning
Prognostic scoring systems are vital in managing brain metastases. They help doctors tailor treatments based on a patient’s prognosis. This ensures treatments meet individual needs and preferences.
| Scoring System | Key Factors | Prognostic Value |
| RPA Classification | Age, KPS, Extracranial disease | Simple, effective prognosis |
| GPA Scoring System | Age, KPS, Number of brain metastases, Extracranial metastases | Nuanced estimate of prognosis |
| Disease-Specific GPA | Primary cancer-specific factors | Tailored prognosis for specific cancers |
Doctors use these systems to give patients accurate, personalized prognosis information. This helps patients make informed decisions about their care.
Specific Cancer Types and Their Brain Metastases Outcomes
Brain metastases outcomes vary by cancer type, like breast, lung, melanoma, and prostate. The prognosis and survival rates are greatly influenced by the primary cancer. Knowing these differences helps patients and healthcare providers make better treatment choices.
Breast Cancer Metastasis to Brain Survival
Breast cancer spreading to the brain is a serious issue for many patients. Thanks to new treatments, survival rates have improved. Median survival rates range from 2 to 16 months after brain metastases diagnosis, depending on the breast cancer type and brain involvement.
HER2-positive breast cancer patients often have better outcomes than those with triple-negative breast cancer. Targeted therapies have shown promise in improving survival for certain patients.
Lung Cancer Brain Metastases Prognosis
Lung cancer is a common cause of brain metastases, affecting prognosis significantly. Brain metastases in lung cancer patients usually mean a poor prognosis. Median survival times typically range from 3 to 7 months after diagnosis. Yet, new treatments and radiation techniques have improved some outcomes.
Genetic mutations, like EGFR, can influence treatment choices and potentially improve survival.
Melanoma Brain Metastases
Melanoma often spreads to the brain, historically leading to a poor prognosis. But, thanks to immunotherapies and targeted therapies, survival has improved. Some patients can achieve long-term survival, though the prognosis remains challenging.
BRAF inhibitors and immunotherapies have changed the treatment landscape for melanoma patients with brain metastases.
Prostate Cancer and Brain Metastases
Brain metastases from prostate cancer are rare but challenging. The prognosis is generally poor, with limited treatment options available. Advances in prostate cancer treatments have not significantly changed outcomes for brain metastases patients.
Research aims to find better treatments for prostate cancer brain metastases, focusing on improving survival and quality of life.
Understanding the specific outcomes for different cancer types is key to tailoring treatments. While overall trends are helpful, each patient’s cancer is unique. This must be considered when deciding on treatment.
Side Effects of Whole Brain Radiation
WBRT is a treatment for brain metastases, but knowing its side effects is key. It can cause short-term and long-term effects. These can affect a patient’s quality of life.
Short-Term Side Effects
WBRT can lead to fatigue, hair loss, and skin irritation. These issues usually go away after treatment ends. Fatigue makes patients very tired and unable to do daily tasks. Hair loss and skin irritation, like redness and itchiness, are also common.
Long-Term Cognitive Effects
WBRT can also have long-term effects on the brain. These include memory loss, trouble concentrating, and changes in personality. Some patients may see a decline in their ability to do daily tasks.
It’s important to think about these effects when choosing treatments. The impact on brain function can differ from person to person.
Impact on Quality of Life
WBRT’s side effects can greatly affect a patient’s life. While it aims to control brain metastases and improve survival, it’s important to weigh the benefits against the risks. Patients and caregivers should be aware of how it can change daily life, including cognitive function and emotional health.
Managing Side Effects
It’s vital to manage WBRT’s side effects to keep a patient’s quality of life high. This can involve medications for symptoms like fatigue and skin issues. Cognitive rehabilitation programs can also help with brain function decline. Patients should talk to their healthcare team to create a plan for managing side effects.
| Side Effect Type | Examples | Management Strategies |
| Short-Term | Fatigue, Hair Loss, Skin Irritation | Rest, Scalp Care, Topical Creams |
| Long-Term | Cognitive Decline, Memory Loss | Cognitive Rehabilitation, Medications |
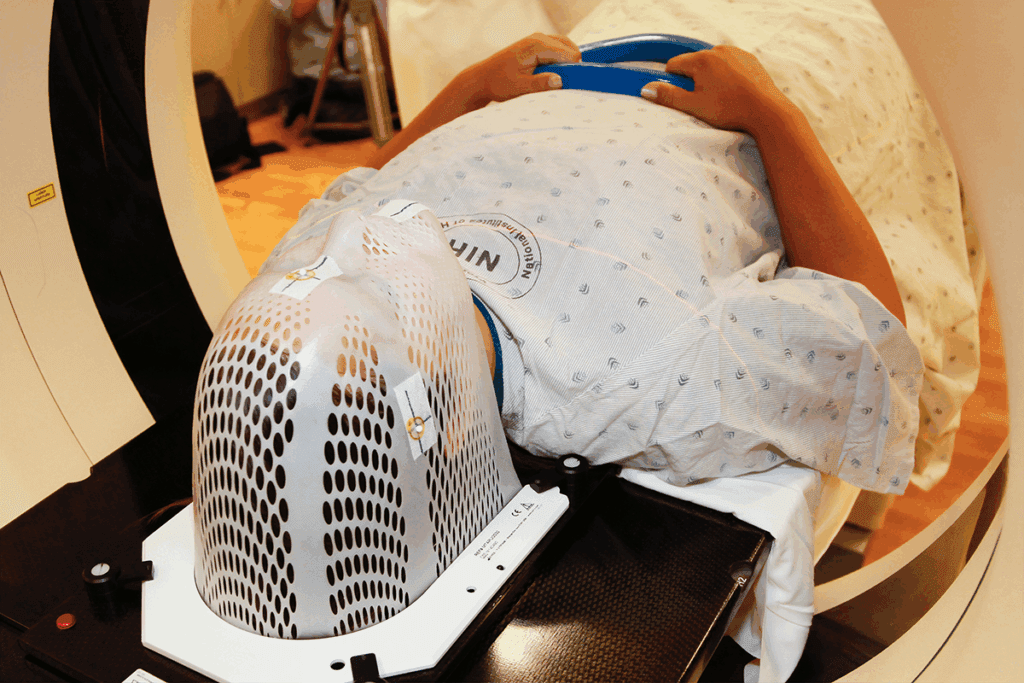
Hippocampal-Sparing Whole Brain Radiation: A Modern Approach
Hippocampal-sparing whole brain radiation is a new method to protect brain function during treatment. It’s a key advancement in radiation therapy. It aims to keep the hippocampus, key for memory and learning, safe from radiation.
How It Differs From Traditional WBRT
Traditional WBRT covers the whole brain, which can harm cognitive skills. Hippocampal-sparing WBRT uses intensity-modulated radiation therapy (IMRT) to target the hippocampus less. This method is more precise, aiming to reduce brain damage.
Cognitive Outcomes and Benefits
Research shows hippocampal-sparing WBRT can lower cognitive decline risks. It helps keep memory and learning skills sharp. This improves patients’ quality of life.
Availability and Eligibility
This treatment is growing in availability at cancer centers. But, who can get it depends on several factors. These include the number and location of brain tumors and the patient’s health. Patients should talk to their oncologist to see if it’s right for them.
Future Directions in Neuroprotective Approaches
Hippocampal-sparing WBRT is a big step in protecting the brain during treatment. Future studies will aim to make these methods even better. They’ll look for new ways to shield the brain and enhance patient results.
| Feature | Traditional WBRT | Hippocampal-Sparing WBRT |
| Radiation Technique | Whole brain irradiation | Intensity-modulated radiation therapy (IMRT) |
| Cognitive Impact | Higher risk of cognitive decline | Reduced risk of cognitive decline |
| Hippocampus Dose | High dose exposure | Sparing of the hippocampus |
Alternative and Complementary Treatments
There are many treatments beyond whole brain radiation therapy for brain metastases. These options let patients choose what works best for them.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery (SRS) is a precise radiation therapy. It targets a specific brain area with a high dose of radiation. SRS works well for treating up to three or four brain metastases. It’s non-invasive and can be done in one session, making it appealing for quick results.
- High precision in targeting tumors
- Non-invasive, reducing recovery time
- Effective for limited number of metastases
Surgery for Brain Metastases
Surgery is an option for brain metastases, mainly for a single, accessible tumor causing symptoms. The decision to have surgery depends on the tumor’s location, size, and the patient’s health. Surgery can quickly relieve symptoms and is often used with other treatments.
- Immediate relief from tumor-related symptoms
- Can be used for diagnostic purposes
- Effective for single, accessible tumors
Systemic Therapies and Targeted Approaches
Systemic therapies, like chemotherapy and targeted therapy, reach cancer cells throughout the body. These treatments are good for managing brain metastases, even when cancer has spread a lot. The right systemic therapy depends on the cancer type and its molecular details.
Proton Therapy for Brain Cancer
Proton therapy uses protons to kill cancer cells, unlike X-rays. It’s great for tumors near important brain areas. Proton therapy can protect healthy tissue, making it a good choice for some patients.
- Precise delivery of radiation
- Reduced risk of damage to surrounding tissue
- Effective for tumors near critical brain structures
These treatments give patients with brain metastases many options. Understanding each treatment’s benefits and limits helps patients make informed choices about their care.
Patient Experiences: Whole Brain Radiation Success Stories
Whole brain radiation success stories are more than just survival. They show living with dignity and purpose after a tough diagnosis. These stories give hope and share insights into the journey of those who have had whole brain radiation therapy.
Long-Term Survivors
Many patients live long after whole brain radiation therapy. Their stories show the possibility of a long life and better quality of life. For example, a patient might say,
“I was diagnosed with brain metastases five years ago, and after whole brain radiation, I’m not only alive but also living a fulfilling life.”
These survivors often thank effective treatment and strong support for their success. Important factors include:
- Early detection and treatment: Quick action can greatly improve results.
- Comprehensive care: A team approach ensures all health aspects are covered.
- Resilience and positivity: A positive outlook helps emotionally and psychologically.
Quality of Life After Treatment
After whole brain radiation therapy, quality of life is a big concern. Many patients see a big improvement in their condition and overall well-being.
Improving quality of life includes:
- Rehabilitation programs: Programs help regain cognitive and physical functions.
- Support groups: Connecting with others who have gone through similar challenges offers emotional support.
- Advanced care planning: Talking about future care needs and preferences reduces stress and uncertainty.
Coping Strategies from Patients
Patients who have had whole brain radiation therapy often find effective ways to cope. These strategies include:
- Mindfulness and meditation: These practices reduce stress and improve mental health.
- Staying connected: Keeping in touch with family and friends is key for emotional support.
- Pursuing hobbies: Doing things they enjoy helps patients feel a sense of purpose.
Caregiver Perspectives
Caregivers are essential in the journey of patients with whole brain radiation therapy. Their views offer valuable insights into the challenges and rewards of caregiving.
Caregivers often stress the importance of:
- Self-care: Taking care of their own health to avoid burnout.
- Seeking support: Connecting with other caregivers and getting professional help when needed.
- Staying informed: Understanding the patient’s condition and treatment options to provide the best support.
By sharing these experiences and strategies, we hope to inspire and support others facing whole brain radiation therapy challenges.
Is Whole Brain Radiation Worth It? Decision-Making Considerations
Deciding on Whole Brain Radiation Therapy (WBRT) is complex. It involves looking at quality of life and survival chances. Patients and their families must think about the benefits and side effects of WBRT on daily life.
Quality vs. Quantity of Life
Choosing WBRT means weighing life’s quality and length. WBRT might add years to life but could also affect daily life, thinking, and happiness.
- Quality of Life: Think about how WBRT might change daily activities, mood, and social life.
- Quantity of Life: Consider if WBRT could extend life and what that means.
When WBRT May Be Most Beneficial
WBRT is often helpful when there are many brain tumors or cancer has spread a lot. It can help manage symptoms and possibly increase survival chances.
When Alternative Approaches Might Be Preferred
For some, treatments like Stereotactic Radiosurgery (SRS) or surgery might be better. This is true for those with fewer brain tumors or a better outlook. The choice between WBRT and other treatments depends on health and cancer details.
Shared Decision-Making with Healthcare Providers
It’s important to make decisions about WBRT together with healthcare providers. Patients should talk openly about treatment options, including WBRT’s benefits and risks. This way, they can choose what fits their values and goals.
“The key to making an informed decision about WBRT lies in understanding the treatment’s implications on both the quality and quantity of life, and discussing these aspects thoroughly with healthcare providers.”
By thinking about these points and talking with healthcare providers, patients can decide if WBRT is right for them.
Follow-Up Care After Whole Brain Radiation
Whole brain radiation therapy (WBRT) is just the start. Ongoing care is key to manage side effects and watch for cancer coming back. After WBRT, patients need careful watching to get the best results.
Monitoring for Recurrence
Regular check-ups are vital to catch cancer coming back early. We use MRI or CT scans and check-ups to keep an eye on patients. Finding cancer early helps us act fast, which can greatly improve results.
Managing Late Effects
WBRT can cause late effects like memory problems, tiredness, and other brain issues. We help patients manage these with medicine, brain training, and lifestyle changes.
Neurological Assessments
Checking the brain is a big part of follow-up care. These checks help us see how the brain is doing, spot new problems, and adjust treatment plans. Regular brain checks let us give better support and help.
Supportive Care Resources
Supportive care is a big part of follow-up care. We offer counseling, support groups, and educational materials to help patients and families deal with treatment challenges. Our goal is to improve life quality for our patients.
In summary, follow-up care after whole brain radiation therapy is essential for the best patient outcomes. By watching for recurrence, managing late effects, doing regular brain checks, and providing support, we can greatly help those with cancer.
Conclusion: Navigating Life After Brain Metastases Treatment
Life after brain metastases treatment can be tough, both emotionally and practically. We’ve talked about how whole brain radiation therapy (WBRT) is often used. It’s key for patients and their caregivers to understand its effects.
Patients need to take care of their health after WBRT. This means watching for signs of the cancer coming back, dealing with late effects, and keeping up with neurological checks. Supportive care resources are very important. They help patients handle the emotional and psychological challenges of treatment.
It’s important to focus on quality of life after treatment. By making smart choices about treatment and using support systems, patients can improve their well-being. We suggest patients and caregivers work with their doctors to create a care plan. This plan should meet their specific needs and help them live a fulfilling life after treatment.
FAQ
What is whole brain radiation therapy (WBRT) and when is it recommended?
Whole brain radiation therapy (WBRT) is a treatment that targets the whole brain. It’s often used for patients with brain metastases or when cancer spreads to the brain.
What are the common primary cancers that spread to the brain?
Lung cancer, breast cancer, melanoma, and prostate cancer are the most common cancers to spread to the brain.
How does whole brain radiation therapy affect life expectancy?
Life expectancy after WBRT varies. It depends on the cancer type, number and location of brain metastases, and the patient’s health.
What is the median survival rate after whole brain radiation therapy?
Survival rates after WBRT can range from a few months to several years. This depends on the cancer type and other factors.
What are the side effects of whole brain radiation therapy?
WBRT can cause fatigue, hair loss, and cognitive changes. Some may experience long-term memory loss and difficulty concentrating.
What is hippocampal-sparing whole brain radiation therapy?
Hippocampal-sparing WBRT aims to reduce cognitive side effects. It spares the hippocampus, a key area for memory and learning.
Are there alternative treatments to whole brain radiation therapy?
Yes, alternatives include stereotactic radiosurgery (SRS), surgery, systemic therapies, and proton therapy. Treatment choice depends on the patient’s condition and history.
How does the primary cancer type affect survival after whole brain radiation therapy?
Survival after WBRT varies by cancer type. For example, breast cancer or lung cancer patients tend to have better survival rates than those with melanoma or aggressive cancers.
What is the role of prognostic scoring systems in brain metastases treatment?
Prognostic scoring systems, like RPA and GPA, help predict outcomes. They guide doctors in making treatment decisions.
How can patients manage side effects after whole brain radiation therapy?
Patients can manage side effects by living a healthy lifestyle, resting regularly, and participating in cognitive rehabilitation. Supportive care resources are also available.
What is the importance of follow-up care after whole brain radiation therapy?
Follow-up care is key to monitor for recurrence and manage late effects. Regular neurological assessments and supportive care are essential.
Can patients with brain metastases from prostate cancer benefit from whole brain radiation therapy?
While rare, WBRT can be effective for prostate cancer brain metastases. It depends on the individual case.
How does whole brain radiation therapy impact quality of life?
WBRT can both improve and worsen quality of life. It can control symptoms and improve survival but also cause side effects that affect daily life.
References
National Center for Biotechnology Information. Survival Following Whole Brain Radiation for Brain Metastases. Retrieved from
https://pmc.ncbi.nlm.nih.gov/articles/PMC6088331/