Last Updated on October 21, 2025 by mcelik

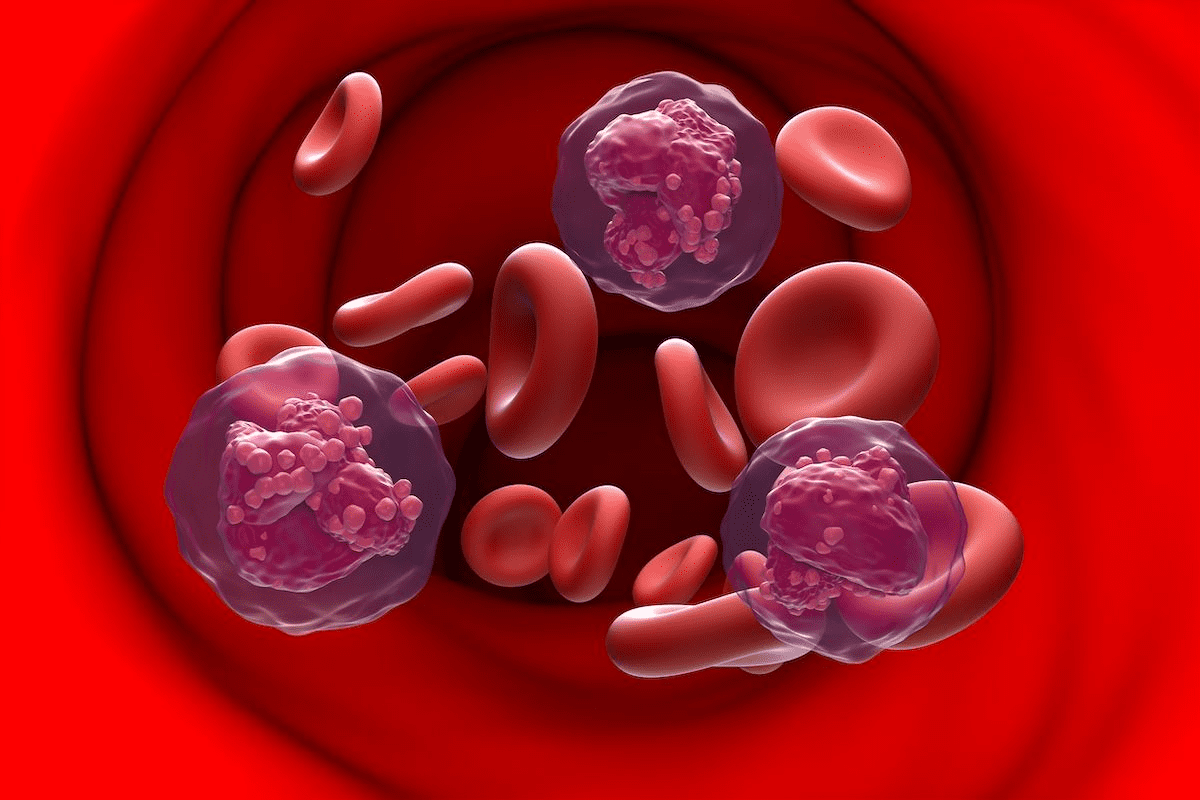
Sickle cell disease is a genetic disorder that affects how red blood cells make hemoglobin. This leads to the cells becoming sickle-shaped. These cells can get stuck in small blood vessels, causing pain and serious problems. Approximately 100,000 Americans are affected by sickle cell disease, with many facing recurring pain and symptoms.Learn lifestyle changes with sickle cell, what can worsen anemia, and how adjusting habits can help manage symptoms and improve overall health.
Managing sickle cell disease needs a full approach. Some things can make a sickle cell crisis worse. Knowing what these triggers are helps people with sickle cell disease manage their symptoms better. This improves their quality of life.
Key Takeaways
- Understanding the genetic nature of sickle cell disease
- Recognizing the role of hemoglobin in the condition
- Identifying factors that can trigger a sickle cell crisis
- The importance of a complete management plan
- Improving quality of life for individuals with sickle cell disease
Understanding Sickle Cell Disease: A Brief Overview
Learning about sickle cell disease is key to helping patients manage it. It’s a genetic disorder that changes the shape of red blood cells. This change makes it hard for the cells to carry oxygen, leading to health problems.
What Causes Sickle Cell Anemia
Sickle cell anemia comes from a gene mutation in the HBB gene. This mutation creates abnormal hemoglobin, or sickle hemoglobin. People with two copies of this mutated gene, one from each parent, usually get sickle cell anemia.
The disease follows an autosomal recessive pattern. This means carriers, with one normal and one mutated gene, often don’t show symptoms. But they can pass the mutated gene to their kids.
How Sickle Cell Affects the Body
Sickle cell disease impacts the body in many ways. The sickled cells can block blood flow in small vessels. This causes pain episodes and can harm organs like the spleen, kidneys, and liver.
Also, these abnormal cells are more likely to break down. This leads to anemia, causing fatigue, weakness, and shortness of breath.
Common Symptoms and Complications
Symptoms of sickle cell disease vary but often include pain episodes, infections, and anemia. Complications can be severe, like acute chest syndrome, stroke, and splenic sequestration.
| Symptom/Complication | Description |
| Acute Chest Syndrome | A condition characterized by a new pulmonary infiltrate on chest radiograph, often accompanied by fever, respiratory symptoms, or chest pain. |
| Stroke | A serious complication that occurs when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. |
| Splenic Sequestration | A life-threatening condition where sickled red blood cells accumulate in the spleen, leading to a sudden drop in hemoglobin levels. |
Knowing about sickle cell disease helps in managing it better. It improves the lives of those affected.
The Impact of Environmental Factors on Sickle Cell Disease

The environment around us can greatly affect those with sickle cell disease. It can cause crises and make symptoms worse. It’s key for patients to know and manage these factors well.
High Altitude and Low Oxygen Environments
High altitudes can harm those with sickle cell disease because of less oxygen. At high elevations, the air has less oxygen. This can cause more red blood cells to sickle, raising the risk of crises.
Precautions at High Altitudes:
- Stay hydrated to help your body adapt.
- Avoid strenuous activities.
- Monitor your body’s response and seek medical help if you experience any severe symptoms.
Air Quality and Pollution Concerns
Air quality is also a big factor in managing sickle cell disease. Pollutants can cause respiratory problems, leading to crises.
| Pollutant | Effect on Sickle Cell Disease | Precautionary Measures |
| Particulate Matter (PM) | Increases respiratory issues, potentially triggering crises. | Avoid outdoor activities when PM levels are high. |
| Ozone (O3) | Can exacerbate respiratory problems. | Stay indoors on days with high ozone levels. |
| Nitrogen Dioxide (NO2) | May worsen lung function. | Use air purifiers indoors. |
Seasonal Changes and Weather Effects
Seasonal changes and weather also impact sickle cell disease. Extreme temperatures can trigger crises.
Knowing how weather affects your body is important. Cold weather can cause blood vessels to constrict, leading to crises. Hot weather can cause dehydration if not managed right.
Weather-Related Precautions:
- Dress appropriately for the weather.
- Stay hydrated, especially in hot weather.
- Avoid exposure to extreme temperatures.
Temperature Extremes: A Significant Trigger
Temperature extremes can really affect people with sickle cell disease. They can trigger crises and make their condition worse. It’s important for patients and caregivers to know how temperature affects the body. They should also take steps to lessen these effects.
How Cold Weather Affects Sickle Cell Patients
Cold weather can cause sickle cell crises in some patients. The cold makes blood vessels narrow. This can cut down on blood flow and oxygen to tissues. This can cause pain and other problems related to sickle cell disease.
To avoid cold weather risks, patients can take precautions. Wearing warm clothes, in layers, helps keep the body warm. Staying inside when it’s very cold and using heaters safely is also good.
Heat Exposure Risks and Prevention
High temperatures also pose big risks for sickle cell patients. Heat can cause dehydration, which is a major crisis trigger. When the body loses too much water, the blood gets thicker. This increases the chance of sickling.
To avoid heat-related problems, staying hydrated is key. Drink lots of water. Also, avoid hard work when it’s very hot. Stay in cool, shaded places to manage heat.
Maintaining Optimal Body Temperature
Keeping the body temperature stable is important for sickle cell disease management. Patients can do this by dressing right for the weather, drinking plenty of water, and avoiding extreme temperatures.
Knowing the weather forecast and planning ahead is also helpful. For example, staying indoors during extreme cold or heat can lower the risk of temperature-related issues.
By understanding the dangers of temperature extremes and taking steps to manage them, sickle cell patients can lower their crisis risk. This can improve their quality of life.
Dehydration: A Major Trigger for Sickle Cell Crisis

It’s key to understand how dehydration affects sickle cell disease. Dehydration can make red blood cells more concentrated. This increases the chance of sickling and can trigger a crisis.
How Dehydration Affects Blood Cells
Dehydration makes blood thicker by reducing plasma volume. This thickness makes red blood cells more likely to sickle. Staying hydrated is vital to avoid these issues.
Recommended Daily Fluid Intake for Patients
People with sickle cell disease should drink lots of water to stay hydrated. The right amount depends on age, activity, and where you live. Drinking eight to ten glasses a day is a good start, but talk to your doctor for specific advice.
Signs of Dehydration to Monitor
It’s important to know the signs of dehydration early. Look out for:
- Dark yellow or amber-colored urine
- Dry mouth and throat
- Fatigue or feeling weak
- Dizziness or lightheadedness
- Headaches
Watching for these signs and drinking enough water can prevent dehydration problems in sickle cell disease.
Physical Exertion and Its Effects on Sickle Cell Patients
For those with sickle cell disease, knowing how physical activity affects them is key. Staying active is good, but it’s important not to overdo it. This balance helps manage their condition well.
Understanding Your Physical Limits
It’s vital for sickle cell patients to know their limits to avoid crises. Listening to your body and noticing signs of tiredness or pain is important. Start with gentle activities and slowly increase them as your body allows.
Safe Exercise Options for People with Sickle Cell
Not all exercises are right for everyone with sickle cell disease. But, there are many safe and beneficial exercise options. These include:
- Low-impact aerobics, such as walking or swimming
- Yoga or Pilates for flexibility and strength
- Cycling or using a stationary bike
Always talk to a healthcare provider before starting a new exercise routine. This ensures it fits your specific needs and health status.
Recovery Strategies After Physical Activity
After exercising, recovery is just as important as the exercise itself. Rest, hydration, and nutrition are essential for recovery. We suggest:
- Drink plenty of water to stay hydrated
- Eat a balanced meal or snack with proteins and carbohydrates
- Rest and avoid hard activities for a few hours after exercising
By knowing your limits, choosing safe exercises, and focusing on recovery, you can enjoy physical activity while managing your sickle cell disease.
Stress and Emotional Factors That Worsen Symptoms
Stress has a big impact on sickle cell disease, affecting both body and mind. It can make symptoms worse, leading to more and more severe crises. Knowing how stress affects sickle cell is key to managing the disease well.
The Physiological Impact of Stress on Sickle Cell
Stress changes the body in many ways for those with sickle cell disease. It releases hormones like cortisol and adrenaline. These hormones can make blood vessels narrow, reducing blood and oxygen to tissues and possibly causing a crisis.
Key physiological effects include:
- Increased heart rate and blood pressure
- Reduced immune function
- Inflammation and oxidative stress
Stress Management Techniques for Patients
It’s vital for sickle cell disease patients to manage stress. There are many ways to do this. These include:
- Meditation and mindfulness: These practices help lower stress and relax.
- Physical activity: Gentle exercises like yoga or walking can reduce stress without too much effort.
- Cognitive-behavioral therapy (CBT): This therapy helps change how one responds to stress.
Mental Health Support Resources
Getting mental health support is important for sickle cell disease. Patients can benefit from:
- Professional counseling: Trained therapists offer ways to deal with stress and emotional challenges.
- Support groups: Meeting others with sickle cell disease can offer emotional support and understanding.
- Online resources: Many online platforms have information, forums, and support for managing stress and mental health.
By understanding stress’s impact and using effective stress management, people with sickle cell disease can live better lives. They can also reduce how often crises happen.
Infections and Illness: Heightened Risks for Sickle Cell Sufferers
People with sickle cell disease are at a higher risk of getting infections. These infections can make their condition worse, leading to more severe crises. It’s important to know the risks and take steps to prevent them.
Common Infections That Trigger Crises
Those with sickle cell disease are more likely to get certain infections. Pneumonia and sepsis are among the most dangerous. These can be caused by bacteria, viruses, or fungi and can be very serious because of their weakened immune system.
Other infections, like urinary tract infections and osteomyelitis (bone infection), are also risky. It’s key for patients to know about these risks and get help quickly if they think they have an infection.
Preventive Measures and Vaccination Recommendations
Stopping infections is key to managing sickle cell disease. Vaccinations are a big part of this. Patients should get all recommended vaccines, like pneumococcal, meningococcal, and flu vaccines. These can help a lot in preventing infections that could lead to a crisis.
Good hygiene is also important. This includes washing hands often, staying away from sick people, and not sharing personal items. Patients should also watch out for places where infections might be more common.
When to Seek Medical Attention
It’s important for sickle cell patients to know when to go to the doctor. Signs like fever, chills, increased pain, or shortness of breath mean they might have an infection. If they have these symptoms, they should see a doctor right away.
Getting infections treated early can really help sickle cell patients. Doctors might give antibiotics or other treatments. Patients should work with their healthcare team to manage infections and avoid serious problems.
Lifestyle Changes with Sickle Cell: Nutrition and Diet
Nutrition plays a big role in managing sickle cell disease. It affects overall health and well-being. Eating a balanced diet can help lessen symptoms and reduce complications.
Foods That May Trigger Symptoms
Some foods can make symptoms worse for people with sickle cell disease. What triggers symptoms can differ for each person. But, there are common foods to watch out for:
- Foods high in sugar and salt
- Processed meats
- Foods with advanced glycation end (AGE) products, like fried foods and charred meats
People with sickle cell disease should pay attention to their diet. They should find out which foods make them feel bad.
Nutritional Recommendations for Sickle Cell Patients
A balanced diet is key for managing sickle cell disease. Here are some important nutritional tips:
| Nutrient | Benefit | Food Sources |
| Protein | Supports overall health and repair | Lean meats, fish, eggs, legumes |
| Omega-3 fatty acids | Reduces inflammation | Fatty fish, nuts, seeds |
| Antioxidants | Protects against oxidative stress | Fruits, vegetables, nuts |
The Role of Folic Acid and Other Supplements
Folic acid is very important for people with sickle cell disease. It helps make red blood cells. Other supplements that can be helpful include:
- Vitamin D
- Zinc
- Antioxidant supplements
But, always talk to a healthcare provider before taking supplements. They can affect medications or cause problems in some people.
Sleep Patterns and Their Impact on Disease Management
For those with sickle cell disease, sleep is key to managing the condition. It affects how often and how severe sickle cell crises are.
Effects of Poor Sleep on Sickle Cell Symptoms
Poor sleep can make sickle cell disease symptoms worse. Studies show that not enough sleep can cause more inflammation and stress. This can lead to sickle cell crises. Some common effects of poor sleep on sickle cell symptoms include:
- Increased pain sensitivity
- Fatigue and decreased energy levels
- Heightened stress levels
- Worsening of depressive symptoms
Developing Healthy Sleep Habits
It’s important to have good sleep habits for sickle cell disease management. Here are some strategies to improve sleep quality:
- Maintain a consistent sleep schedule
- Create a sleep-conducive environment (cool, dark, quiet)
- Avoid caffeine and heavy meals before bedtime
- Engage in relaxing activities before sleep (e.g., reading, meditation)
Managing Pain for Better Sleep Quality
Pain is a big problem for sleep in sickle cell disease. Managing pain well is key to better sleep. Some approaches to managing pain for better sleep include:
- Using prescribed pain medications as directed
- Applying heat or cold packs to affected areas
- Engaging in gentle stretches or relaxation techniques before bed
- Keeping a pain journal to identify patterns and triggers
By focusing on sleep and its role in sickle cell disease, people can manage their condition better. This can improve their life quality a lot.
Medications and Substances to Avoid with Sickle Cell Disease
Certain medications and substances can harm people with sickle cell disease. It’s important to avoid triggers and watch for interactions with treatments.
Over-the-Counter Medications That May Cause Complications
Many think over-the-counter (OTC) meds are safe. But for those with sickle cell disease, some can be very harmful. For example, some pain relievers can hurt the kidneys, which are already at risk.
Be careful with these OTC meds:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, which can damage the kidneys if used too much.
- Aspirin, which can make bleeding more likely.
- Decongestants with pseudoephedrine, which can narrow blood vessels and trigger a crisis.
| OTC Medication | Potential Risk |
| NSAIDs (e.g., ibuprofen) | Kidney damage |
| Aspirin | Increased risk of bleeding |
| Decongestants (e.g., pseudoephedrine) | Vasoconstriction, potentially triggering a crisis |
Drug Interactions with Sickle Cell Treatments
Drug interactions are a big worry for sickle cell disease patients. Some meds can make treatments less effective or increase side effects.
For example, hydroxyurea is a common treatment. But its effectiveness can be affected by other meds, like antibiotics or antifungals.
We suggest:
- Tell your doctor about all meds and supplements you’re taking.
- Talk to your pharmacist about possible drug interactions.
- Check your meds regularly to make sure they’re safe and working well.
Knowing which meds and substances to avoid can help manage sickle cell disease better. This can lower the risk of serious problems.
Pain Management Strategies for Sickle Cell Crises
Pain management is key for those with sickle cell crises. It helps them live better every day. Managing pain well is important for their quality of life.
Medical Interventions for Pain Relief
Medical treatments are vital for pain during sickle cell crises. Opioid analgesics are used for severe pain but need careful watch for addiction risk. Non-opioid analgesics, like NSAIDs, work well with other treatments.
It’s important for patients to work with their doctors on a pain plan. This plan should cover the right medicines, how often to take them, and ways to avoid side effects.
Home Remedies and Non-Pharmaceutical Approaches
Home remedies and non-medical methods can also help with pain. Heat therapy and cold packs can ease muscle tension and pain. Relaxation techniques like deep breathing, meditation, and yoga can also help reduce pain and stress.
Staying healthy is also important. Eating well, drinking enough water, and getting enough sleep can help manage pain episodes.
Creating an Effective Pain Management Plan
Creating a good pain plan takes teamwork. Patient education is essential. It helps people understand their condition and make smart choices about their care.
The plan should fit the person’s needs. It might include medicines, lifestyle changes, and other therapies. It’s important to regularly check and update the plan to keep it working well.
Modern Treatments and Medical Interventions
Modern treatments offer new hope for managing sickle cell disease. Advances in medical research have led to the development of various treatments. These treatments improve the quality of life for patients.
Current FDA-Approved Medications
The U.S. Food and Drug Administration (FDA) has approved several medications for sickle cell disease. These include:
- Hydroxyurea: This is a well-established medication that reduces the frequency of painful crises. It may also reduce the need for blood transfusions.
- L-Glutamine: An amino acid that has been shown to reduce the frequency of sickle cell crises.
- Crizanlizumab: A monoclonal antibody that has been approved to reduce the frequency of sickle cell crises.
- Voxelotor: A medication that increases hemoglobin levels. It reduces the risk of complications.
These medications have undergone rigorous clinical trials. They have shown to be safe and effective.
Emerging Therapies and Clinical Trials
Beyond current treatments, researchers are actively exploring new therapies through clinical trials. Some promising areas include:
- Gene therapy: Scientists are working on correcting the genetic mutation that causes sickle cell disease.
- Stem cell transplantation: This involves replacing the patient’s bone marrow with healthy stem cells.
- Novel pharmacological agents: Researchers are developing new drugs that target specific pathways involved in the disease.
Participation in clinical trials can provide patients with access to cutting-edge treatments. It also contributes to the advancement of medical knowledge.
Gene Therapy and Future Treatment Directions
Gene therapy represents a potentially curative approach for sickle cell disease. It aims to eliminate the root cause of the disease by correcting the underlying genetic defect. While in the experimental stages, gene therapy has shown promising results in early clinical trials.
Future treatment directions may also involve personalized medicine approaches. Treatments will be tailored to the individual patient’s genetic and clinical profile.
Conclusion: Empowering Yourself to Live Well with Sickle Cell Disease
Living with sickle cell disease means you need a full plan to handle its effects every day. Knowing what makes it worse helps you make better choices. This way, you can live a better life.
Self-care is key in managing sickle cell disease. Eating right, drinking plenty of water, and avoiding very hot or cold places are important. Also, exercising regularly, managing stress, and getting enough sleep help a lot.
Managing sickle cell disease well means using medicine and making lifestyle changes. Working with your doctor and making smart choices can help. This can make crises less common and improve your health overall.
We urge those with sickle cell disease to be proactive in their care. Use the newest treatments and strategies to improve your life.
FAQ
What is sickle cell disease and how does it affect the body?
Sickle cell disease is a genetic disorder that affects hemoglobin production. This causes red blood cells to become misshapen and break down. It can lead to anemia, pain crises, and an increased risk of infections.
How can environmental factors impact sickle cell disease?
Environmental factors like high altitude, poor air quality, and extreme temperatures can trigger sickle cell crises. Understanding and mitigating these factors can help manage the condition.
What are the risks associated with temperature extremes for individuals with sickle cell disease?
Both cold and hot weather can trigger sickle cell crises. Cold weather can cause blood vessels to constrict. Hot weather can lead to dehydration. Maintaining optimal body temperature is key.
Why is hydration important for individuals with sickle cell disease?
Dehydration can cause red blood cells to become more concentrated, increasing the risk of sickling. Drinking enough fluids is essential to prevent dehydration and reduce the risk of crises.
How does physical exertion affect individuals with sickle cell disease?
Physical exertion can trigger sickle cell crises if not managed properly. Understanding personal physical limits, engaging in safe exercise options, and using recovery strategies can help mitigate risks.
Can stress and emotional factors worsen sickle cell symptoms?
Yes, stress and emotional factors can exacerbate sickle cell symptoms. Practicing stress management techniques and seeking mental health support can help alleviate these effects.
What are the heightened risks of infections for individuals with sickle cell disease?
Individuals with sickle cell disease are more susceptible to infections, which can trigger crises. Preventive measures, vaccination recommendations, and knowing when to seek medical attention are critical.
How does nutrition and diet impact sickle cell disease management?
A balanced diet rich in essential nutrients can help manage sickle cell disease. Certain foods may trigger symptoms. Nutritional recommendations, including folic acid supplements, can support overall health.
How do sleep patterns affect sickle cell disease management?
Poor sleep can exacerbate sickle cell symptoms. Developing healthy sleep habits and managing pain effectively can improve sleep quality and overall disease management.
What medications and substances should individuals with sickle cell disease avoid?
Certain over-the-counter medications, alcohol, tobacco, and recreational drugs can complicate sickle cell disease management. Understanding drug interactions with treatments is also important.
What are effective pain management strategies for sickle cell crises?
Medical interventions, home remedies, and non-pharmaceutical approaches can help manage pain during sickle cell crises. Creating an effective pain management plan is essential for individuals with the condition.
What are the current and emerging treatments for sickle cell disease?
Current FDA-approved medications, emerging therapies, and gene therapy represent the evolving landscape of sickle cell disease treatment. Staying informed about these developments can help individuals manage their condition effectively.
How can individuals with sickle cell disease empower themselves to live well with the condition?
By understanding their condition, making informed lifestyle changes, and staying up-to-date with the latest treatments and management strategies, individuals with sickle cell disease can improve their quality of life.
References
- Schechter, A. N. (2024). Sickle cell anaemia therapy in 2025. British Journal of Haematology, 206(3), 842“845. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11886933/