Last Updated on November 27, 2025 by Bilal Hasdemir
The efficiency of surgeries is very important. But, robotic surgery takes longer to set up. This can slow down how well surgeries go. Healthcare workers need to know about these issues.
Robotic surgical systems come with a big price tag. They’ve changed the medical world with their accuracy and small incisions. But, the cost is really high.
The money side of robotic surgery is complex. It includes the upfront cost and the ongoing bills. Hospitals need to know these costs before they decide to use robotic surgery.
The first cost for robotic systems is huge. There’s also the cost of changing the operating room to fit the robot.
There are also ongoing costs. These include maintenance, which can be a lot, and the cost of tools used in surgeries.
The total cost can be tough on a hospital’s budget. Hospitals must think carefully about the benefits of robotic surgery against the high costs.
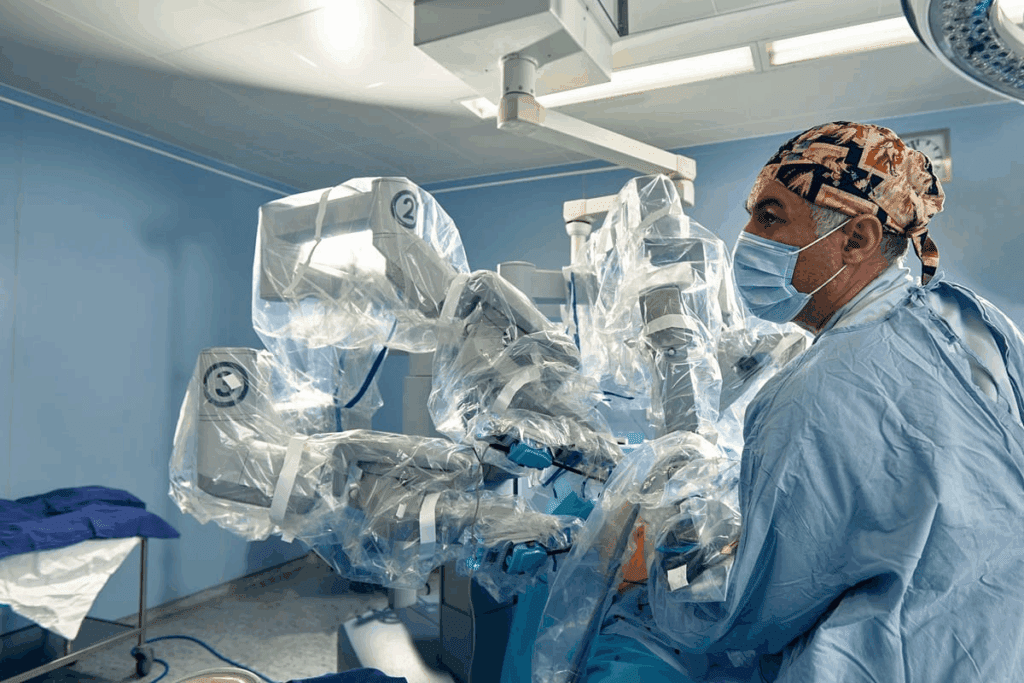
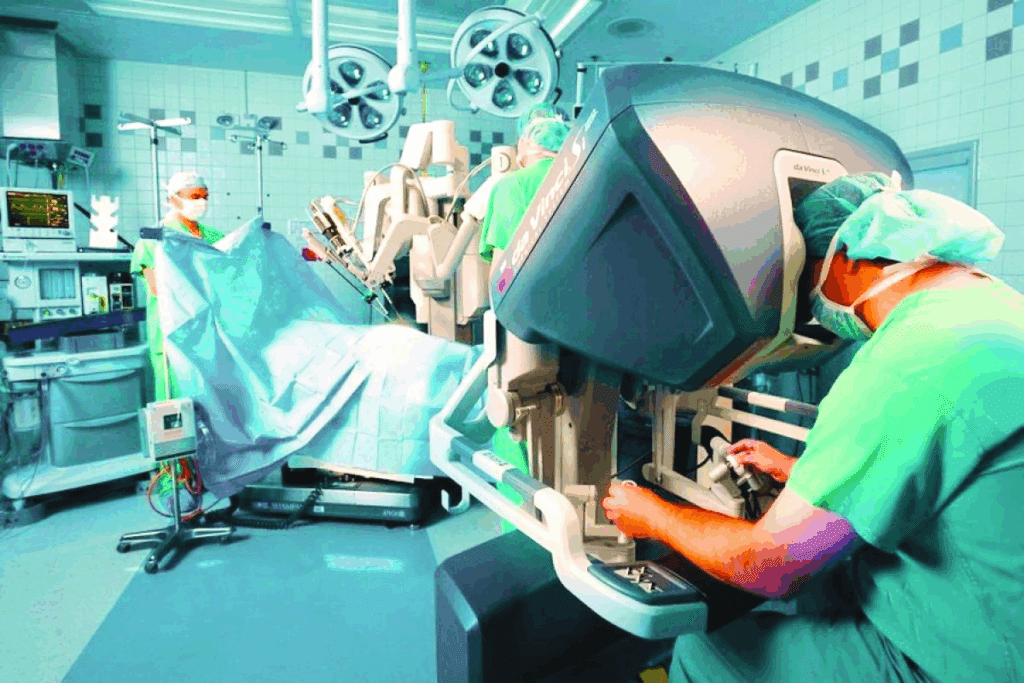
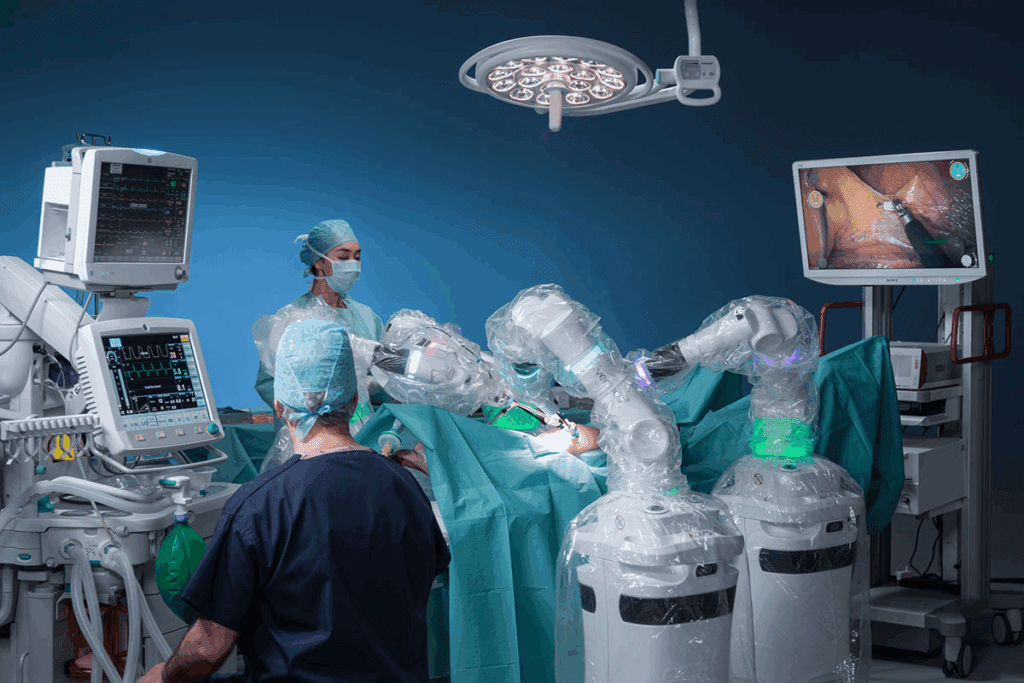
While surgical procedures demand efficiency, robotic surgery encounters significant challenges. The setup for robotic surgery is complex. It involves preparing the robotic equipment, positioning the patient, and getting the surgical team ready.
Preparing for robotic surgery is a big job. It takes a lot of time to set up the robotic system and check all the equipment. The surgical team also needs to be well-prepared. This complex setup can cause delays, affecting the surgery’s efficiency.
Getting the patient in the right position and docking the robotic arms takes extra time. These steps are key for a successful surgery. But, they can make the operating room busy, limiting restricted access for other patients.
Long setup times for robotic surgery affect the operating room’s schedule a lot. Delays in one surgery can spread, impacting the day’s schedule. This means fewer patients can be treated, putting more pressure on the team.
The longer setup time also means higher costs. Longer operating times lead to more expenses. So, making the setup process more efficient is key to keeping robotic surgery affordable and effective.
Disparities in robotic surgery access are a big worry in healthcare. Not everyone can get to this advanced tech.
Robotic surgery is great but has big challenges. It’s hard to get because of limited availability and restricted access. Some areas and groups can’t get to these surgeries.
The geographic distribution of robotic surgery is a big issue. Big cities and top hospitals have these systems. But, rural and remote places often don’t.
This means some patients face a geographic barrier. They might wait longer for treatments that robotic surgery could help with.
Socioeconomic barriers also block access to robotic surgery. The cost is too high for many. This is true for those without good insurance or money.
High insurance coverage limitations and out-of-pocket expenses make it hard. This financial wall stops some from getting these surgeries.
We need to find ways to make robotic surgery more available. This could mean spreading out the systems more. Or making the surgeries cheaper for more people.
Learning robotic surgery takes a lot of time and effort. It’s complex, so surgeons and staff need special skills. They must learn how to use these systems well.
How long it takes to train surgeons is key. They learn both theory and practice. This can take months to a year or more, based on their experience and how often they do surgeries.
The training includes:
“The learning curve for robotic surgery is steep, but with structured training, surgeons can achieve proficiency and improve patient outcomes.”
Nurses and surgical technicians are key to robotic surgery success. They need good training to help surgeons and manage the systems.
| Training Component | Description | Duration |
| Theoretical Training | Understanding the principles and operation of robotic systems | 2-4 weeks |
| Practical Training | Hands-on experience with robotic systems during surgeries | 3-6 months |
| Continuous Education | Regular updates on new technologies and techniques | Ongoing |
As robotic surgery grows, so does the need for ongoing learning. Hospitals must invest in good training programs. This ensures staff stays up-to-date with new methods and tools.
Robotic surgery doesn’t have the tactile feedback surgeons are used to. This makes procedures less precise and less safe.
Without tactile feedback, surgeons struggle with tissue handling and force application. They must rely heavily on visual cues, which can be misleading or not enough.
This can lead to increased risks of tissue damage or improper force application. It can make the surgery more complicated and affect patient outcomes.
To make up for the lack of tactile feedback, surgeons use advanced visual techniques. They use high-definition 3D visualization and enhanced imaging to understand the surgical site better.
But, these visual techniques have their limits. Reliance on visual information alone can lead to misinterpretation of tissue properties or anatomical structures, making complex or delicate procedures harder.
Research is ongoing to improve tactile feedback in robotic surgery. Advances in sensor technology and haptic feedback systems are being explored to overcome current limitations.
We understand that the lack of tactile feedback is a big challenge in robotic surgery. It’s essential to address this issue to improve surgical outcomes and expand the capabilities of robotic surgical systems.
Robotic surgery is getting better, but we must watch out for technical problems. These can happen with any complex tech, like robotic surgery systems. They might not work right, which could affect how well surgery goes.
The da Vinci Surgical System and others like it are very advanced. But, they can have technical problems. These can be software bugs, hardware issues, or problems with the robotic arms or tools.
Some common issues include:
These problems can cause delays or make surgery harder. This might affect how well the patient does.
Power failures during surgery are a big worry. They can happen for many reasons, like the power grid failing or equipment problems.
Hospitals and surgery centers have backup power to avoid these issues. They use things like UPS or emergency generators. These keep the robotic equipment working even when the main power goes out.
| Backup Power System | Description | Response Time |
| Uninterruptible Power Supply (UPS) | Provides immediate backup power using batteries | Instantaneous |
| Emergency Generator | Activates to provide power in case of extended outage | Typically 10-60 seconds |
Knowing about these problems and having good backup systems helps. It makes sure robotic surgery stays safe and effective.
Extended operation times in robotic surgery raise important patient safety concerns. Robotic surgery offers benefits like precision and less invasiveness. But, it can sometimes take longer than traditional surgery.
Longer operation times can lead to serious risks for patients. These include higher risks of anesthesia problems and infection. It’s vital to understand what causes these long times and how they affect patient outcomes.
One major concern is the longer time under anesthesia. Longer anesthesia times can lead to complications like respiratory and cardiac issues. Patients in robotic surgery may face a higher risk of anesthesia-related complications due to the extended operation times.
Anesthesiologists and surgical teams must closely monitor patient vital signs. They need to adjust anesthesia levels as needed. Good communication and teamwork are key to managing these risks.
Prolonged surgeries, like those in robotic surgery, can raise the risk of surgical site infections. The longer a patient is in the surgical environment, the higher the risk of contamination and infection.
To reduce this risk, surgical teams use several strategies. They include using prophylactic antibiotics, keeping the surgical area sterile, and ensuring all equipment is sterilized.
| Risk Factor | Implications | Mitigation Strategies |
| Prolonged Anesthesia | Increased risk of respiratory and cardiac complications | Close monitoring of patient vital signs, adjusted anesthesia levels |
| Surgical Site Infection | Increased risk of infection with prolonged exposure | Prophylactic antibiotics, sterile surgical environment, proper equipment sterilization |
Surgeon expertise is key in robotic surgery success. A surgeon’s experience and skill greatly affect the operation’s outcome.
Robotic surgery, though advanced, faces surgeon skill variability. The need for skilled surgeons is critical. It’s important to focus on maintaining and assessing surgeon skills.
Research links surgeon experience to robotic surgery results. More experienced surgeons often have better outcomes. They have fewer complications and quicker recovery times.
| Surgeon Experience Level | Average Complication Rate | Average Recovery Time |
| Low | 15% | 6 weeks |
| Medium | 8% | 4 weeks |
| High | 3% | 2 weeks |
The table shows how experience affects outcomes. Clearly, more experience leads to better results.
Keeping surgeon skills sharp in robotic surgery is tough. It needs ongoing training and feedback. Sometimes, surgeons must re-certify.
Hospitals and medical groups are tackling these issues. They use:
These steps help surgeons stay proficient. They keep up with new robotic surgery techniques.
Recognizing surgeon dependency and skill variability is vital. It helps reduce outcome gaps. This improves care in robotic surgery.
Effective hospital resource allocation is key for robotic surgery success. Hospitals face big challenges when adding robotic surgery to their services. They need to manage resources well.
Robotic surgery needs big changes in hospital setup. Hospitals must update their operating rooms for the new systems. This includes new electrical and data connections and enough space for everyone.
Also, thinking about long-term costs is important. Robotic equipment is high-tech and needs regular, expensive maintenance. Hospitals must make sure their setup can handle these systems without problems.
Starting robotic surgery programs means big changes for staff. Hospitals must train everyone to use the new systems. This includes surgeons, nurses, and technicians.
Hospitals might also need to change how many staff they have. They might need more people with special skills or keep training current staff. This helps everyone stay good at using the robotic tech.
Knowing these challenges helps hospitals plan better. They can then improve patient care and results with robotic surgery.
Converting from robotic to open or laparoscopic surgery is a big deal in planning surgeries. Robotic surgery has made big strides, but sometimes it needs to switch to another method. This can happen for many reasons.
There are a few reasons why a surgeon might switch from robotic to another method. These include:
Knowing these reasons helps surgeons get ready for possible problems. It helps them make smart choices about how to proceed.
Switching to open or laparoscopic surgery can really change how a patient does after surgery. Potential complications include:
We know robotic surgery is great, but sometimes needing to switch can hurt patient results. So, it’s key to think carefully about the risks and benefits. And to have backup plans ready.
Understanding the risks of switching to open or laparoscopic surgery helps us manage what patients expect. It also helps us improve how we care for them during surgery.
Robotic surgery relies heavily on complex technology. This has made the supply chain vulnerable, affecting equipment availability. Robotic systems need specific parts, and any supply chain issue can cause downtime. This impacts scheduling and patient care.
Robotic systems need specific parts to work well. But, supply chain problems can happen. These include delays, logistics issues, and global events like pandemics.
When these parts are not available, we see:
Maintenance downtime is a part of robotic system management. But, how often and for how long it happens affects surgery schedules.
Here’s a table showing how downtime affects scheduling:
| Downtime Duration | Impact on Surgical Scheduling | Potential Mitigation Strategies |
| Less than 24 hours | Minimal disruption; rescheduling of non-urgent procedures. | Advance scheduling of maintenance during low surgical volume periods. |
| 1-3 days | Moderate disruption; possible delay of elective surgeries. | Coordination with surgical teams to adjust schedules. |
| More than 3 days | Significant disruption; possible cancellation of surgeries. | Expedited repair services; use of backup equipment if available. |
Understanding supply chain issues and downtime helps healthcare institutions. They can plan better to keep robotic surgery services running smoothly.
The cost of robotic surgery is a big worry because it’s expensive and insurance coverage varies. It’s key to grasp the financial side of robotic surgery for patients.
Insurance for robotic surgery changes a lot depending on the provider and policy. Some plans cover it, but others don’t, or only under certain conditions. Patients often have to deal with complex insurance to see what’s covered. This can cause worry and stress for those thinking about robotic surgery.
Even with insurance, the costs for robotic surgery can be high. These costs include deductibles, copays, and care before and after surgery. For those with little money or no good insurance, it’s a big problem.
To help with these costs, some hospitals offer financial help or advice. Knowing about these resources is important for anyone thinking about robotic surgery.
Exploring the negatives of robotic surgery is key. We must balance these against its benefits. High costs and longer setup times are drawbacks. Yet, the precision and quicker recovery times are big pluses for patient safety.
The benefits of robotic surgery are clear. It offers better accuracy and less invasive procedures. This can lead to better health outcomes for patients. But, we must carefully weigh these against the risks.
In summary, robotic surgery is complex. It needs careful thought about its benefits and drawbacks. By understanding these, we can give our patients the best care and keep them safe during surgery.
Robotic surgery’s downsides include high costs and long setup times. It’s not available everywhere, and it’s hard to learn. You also miss out on feeling the tissues, face technical problems, and risk machine failures.
High costs put a big strain on healthcare places, mainly those with tight budgets. They need a lot of money upfront and then ongoing costs for upkeep and use.
Setting up for robotic surgery is complex. This can cause delays in the operating room. It affects the surgery’s efficiency.
Yes, not everyone can get robotic surgery. It’s hard to reach some areas and people because of money and location issues.
You need a lot of training to use robotic surgery. It’s hard, mainly for those new to it.
Surgeons can’t feel tissues or apply force precisely. They have to rely on what they see instead.
Technical problems and machine failures are risks. They can harm patient safety and the surgery’s success.
Longer surgeries mean more time under anesthesia. This raises the risk of complications. Longer times also increase infection risks.
The surgeon’s experience greatly affects the surgery’s success. More experienced surgeons tend to have better results.
Starting robotic surgery programs is hard. It needs a lot of money and staff. You also have to change your setup and staff levels.
Sometimes, you have to switch to open or laparoscopic surgery. This can harm the patient and increase surgery risks.
The parts for robotic systems can be hard to get. This can cause equipment problems and delays in surgery plans.
Patients often have to pay a lot for robotic surgery. This is hard for those with little money, because insurance doesn’t always cover it.
Yes, there are extra costs. These include ongoing maintenance, setup needs, and training for staff. All these add up to the total cost of robotic surgery.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!