Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that over 300,000 spine surgeries are done every year in the United States? Microdiscectomy is a top choice for fixing herniated discs Lumbar microdiscectomy outcome.
Microdiscectomy is key in treating lumbar disc herniation. It greatly reduces pain and boosts life quality. The success rate is high, with over 80% of patients being happy with the results.
The Macnab classification helps measure how well the surgery goes. It shows how satisfied patients are and if the surgery was a success. With such a high microdiscectomy success rate, it’s a go-to for many with lumbar disc herniation.
Key Takeaways
- Microdiscectomy is a common surgical procedure for treating herniated discs.
- The success rate of microdiscectomy is over 80% in terms of patient satisfaction.
- The Macnab classification is used to evaluate the outcome of microdiscectomy surgeries.
- Patient satisfaction is a key indicator of the success of spine surgery.
- Microdiscectomy offers a significant reduction in pain and improved quality of life.
Understanding Lumbar Microdiscectomy
Learning about lumbar microdiscectomy is key for those thinking about surgery for a herniated disc. This surgery is a small cut to fix a big problem. It helps by taking pressure off nerves from a herniated disc.
Definition and Procedure Overview
Lumbar microdiscectomy removes the part of the disc that’s pressing on nerves. It’s done with a tiny incision, thanks to modern tools. The steps include:
- Making a small incision in the lower back.
- Using a microscope or endoscope to see the disc.
- Removing the bad part of the disc.
- Freeing the nerve from pressure.
When Microdiscectomy Is Recommended
Doctors suggest microdiscectomy when other treatments don’t work. This includes trying physical therapy and pain meds first. The choice to have surgery depends on several things, like:
Diagnostic Criteria | Description |
Symptoms | Persistent pain, numbness, tingling, or weakness in the lower back and legs. |
Imaging Studies | MRI or CT scans showing disc herniation compressing spinal nerves. |
Conservative Treatment | Failure to improve with non-surgical treatments. |
Evolution of the Procedure
The microdiscectomy has changed a lot over time. New tools and ways of doing surgery have made it better. Today’s microdiscectomy is:
- Less invasive.
- Uses better ways to see inside the body.
- Causes less damage.
- Means a quicker recovery.
Knowing more about lumbar microdiscectomy helps patients make better choices. It lets them understand what to expect from the surgery.
Defining Success in Spine Surgery Outcomes
Measuring the success of spine surgery is complex. It looks at both how well the surgery works and what the patient says. Success isn’t just about the surgery’s technical success. It’s also about how it improves the patient’s life.
Clinical Measures of Success
There are key clinical measures for spine surgery success:
- Improvement in neurological function
- Less pain
- More mobility
- Spine stability
Doctors use physical checks, X-rays, and MRI scans to measure these.
Patient-Reported Outcome Measures
Patient feedback is vital for judging surgery success. It includes:
- The Roland-Morris Disability Questionnaire for back pain
- Pain scales like the Visual Analog Scale (VAS)
- Quality of life surveys, such as SF-36 or EQ-5D
The Macnab Classification System
The Macnab system is key for spine surgery results, like microdiscectomy. It has four levels:
“Excellent: complete recovery, no pain; Good: some pain, but able to work; Fair: improved, but with significant pain or limitations; Poor: little or no improvement.”
This system makes it easy to judge surgery success based on patient feedback and doctor checks.
By using clinical checks, patient feedback, and systems like Macnab, we can fully understand spine surgery success. This helps us better care for patients.
Short-Term Success Rates of Microdiscectomy
Research shows that microdiscectomy is very successful right after surgery and in the first year. This is because it’s a minimally invasive procedure. It causes less damage and leads to faster recovery times than traditional surgery.
Immediate Post-Operative Outcomes
Right after surgery, patients often feel much less pain and can move around better. Effective pain management is key in the early recovery. Many patients can go home the same day or the next day after surgery.
- Reduced pain levels
- Improved mobility
- Effective pain management strategies
1-Year Follow-Up Results
One year after surgery, most patients are happy with the results. They can usually go back to their usual activities, like work and hobbies. This shows that the relief from symptoms lasts a long time.
- High patient satisfaction rates
- Significant reduction in leg pain and sciatica
- Improved quality of life
Factors Affecting Short-Term Success
Several things can affect how well microdiscectomy works in the short term. These include the patient’s health, how bad the disc herniation is, and the surgeon’s skill. Proper patient selection is very important for the best results.
Factor | Impact on Success |
Patient Health Status | Pre-existing health conditions can affect recovery and outcome |
Severity of Disc Herniation | More severe herniations may have different outcomes |
Surgeon Experience | More experienced surgeons tend to have better outcomes |
Lumbar Microdiscectomy Outcome: Long-Term Data
It’s important to know how well lumbar microdiscectomy works over time. This knowledge helps both patients and doctors. The good news is that many patients see lasting benefits from the surgery.
5-Year Success Rates
Research shows that lumbar microdiscectomy works well even five years later. Many patients feel better and live better lives. For example, a study found that over 80% of patients were happy with their results five years after surgery.
What makes these results last? It’s mainly because of:
- Choosing the right patients
- Using a skilled surgical method
- Good care after surgery
10-Year Follow-Up Studies
Studies that follow patients for ten years or more are very helpful. They show that many patients keep feeling better over time. A longitudinal study found that most patients kept improving for over a decade.
Durability of Surgical Benefits
How long the benefits of lumbar microdiscectomy last is key. The good news is that it can give long-lasting relief to many. But, how long it lasts depends on the patient’s health and how well they follow up care.
Looking at the long-term data, lumbar microdiscectomy is a great option for many with lumbar disc herniation. The secret to success is a careful approach. This includes choosing the right patients, doing the surgery well, and taking good care after.
“The long-term outcomes of lumbar microdiscectomy are generally favorable, with a significant proportion of patients experiencing sustained benefits.”
— Journal of Neurosurgery: Spine
Recurrence Rates After Microdiscectomy
Microdiscectomy is a common surgery for back pain. But, it can sometimes fail and the pain comes back. Knowing why this happens helps doctors and patients make better choices.
Risk of Reherniation
The chance of reherniation, or the disc bulging again, depends on several things. These include the patient’s health, how much of the disc was removed, and any spinal problems they might have. Studies show reherniation can happen in 5% to 15% of cases.
Factors Influencing Reherniation:
- Patient Age and Health Status: Older patients or those with certain health conditions may have a higher risk of reherniation.
- Extent of Disc Removal: The amount of disc material removed during surgery can impact the risk of recurrence.
- Surgical Technique: The skill and technique of the surgeon play a significant role in minimizing the risk of reherniation.
Timeframe for Recurrence
Reherniation can happen at any time after surgery. But, it’s most common in the first few years. Knowing when it might happen helps plan follow-up care.
Timeframe | Risk of Recurrence |
0-1 Year | Higher risk due to incomplete healing or residual disc material |
1-5 Years | Moderate risk as the spine continues to degenerate |
5+ Years | Lower risk, but possible due to ongoing degenerative changes |
Managing Recurrent Disc Herniation
Dealing with a herniation that comes back needs a mix of treatments. Sometimes, surgery is needed again. The choice depends on how bad the symptoms are and the patient’s health.
Strategies for Managing Recurrence:
- Conservative Management: First, try physical therapy, pain management, and lifestyle changes.
- Reoperation: If these don’t work and symptoms are severe, surgery might be needed.
- Lifestyle Changes: Keeping a healthy weight, exercising regularly, and good posture can help prevent it from coming back.
Factors Influencing Microdiscectomy Success Rates
Knowing what affects microdiscectomy success is key for both patients and surgeons. The success of this surgery depends on many things. These include the patient’s health and the surgical method used.
Patient Age and Health Status
Age and health are big factors in microdiscectomy success. Younger patients with fewer health problems usually do better. We look at things like diabetes, smoking, and overall health to decide if a patient is a good candidate.
Table: Factors Affecting Microdiscectomy Success
Factor | Description | Impact on Success |
Patient Age | Younger patients tend to have better recovery rates. | Higher success rate in younger patients |
Health Status | Presence of comorbidities can affect recovery. | Fewer comorbidities = higher success rate |
Herniation Type | Type of disc herniation (e.g., extruded, sequestered). | Certain types may have better outcomes |
Herniation Type and Location
The type and where the disc herniation is located are very important. Some herniations, like extruded or sequestered ones, might do better than others. Where the herniation is in relation to the nerve root also matters a lot.
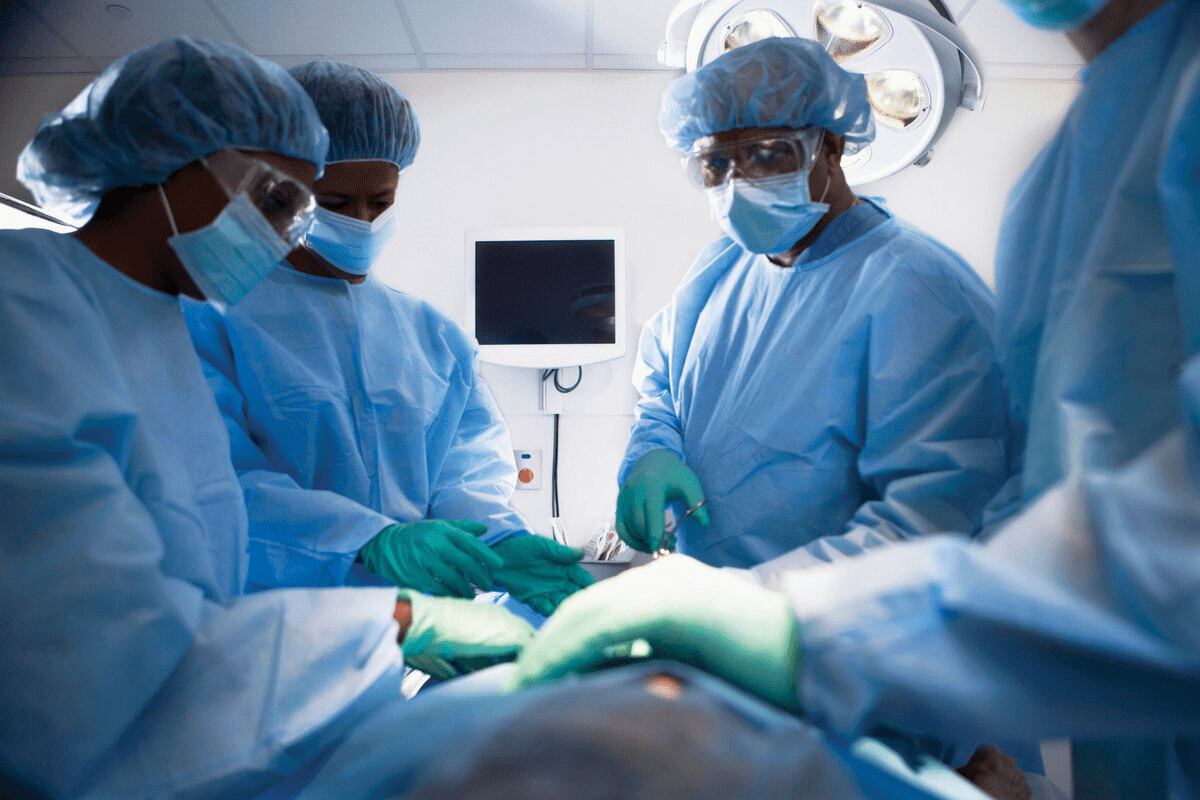
Surgeon Experience and Technique
The surgeon’s experience and the method used can greatly affect the success of microdiscectomy. More experienced surgeons tend to get better results. The specific technique, like the size of the incision and how much tissue is removed, also plays a role.
Pre-existing Spinal Conditions
Spinal conditions like stenosis or spondylolisthesis can impact microdiscectomy success. Patients with these conditions might need more surgery or have a harder recovery. We carefully check for these conditions before surgery to improve outcomes.
By understanding these factors, we can better choose who should have microdiscectomy. We can also improve surgical techniques to get the best results.
Lumbar Microdiscectomy Recovery Timeline
Knowing how long it takes to recover from lumbar microdiscectomy is key. It helps patients set realistic goals and plan their care. Everyone recovers differently, but there are common steps most follow.
Hospital Stay and Immediate Recovery
Most people have this surgery as an outpatient. This means they go home the same day. But, some might need to stay in the hospital for a bit if there are issues.
Right after surgery, patients are watched in the recovery room. This is to make sure everything goes smoothly.
Key aspects of immediate recovery include:
- Resting in a comfortable position to minimize discomfort
- Managing pain through medication prescribed by the surgeon
- Gradually increasing mobility with the help of healthcare professionals
Return to Daily Activities
When patients can go back to their usual activities varies. But, most can do so in 2-6 weeks. It’s important to listen to the surgeon about how active to be.
Typical milestones include:
- Light walking and stretching within the first week
- Gradually increasing activity levels over the next 2-3 weeks
- Returning to more strenuous activities, such as heavy lifting or bending, after 4-6 weeks
Complete Recovery Expectations
Full recovery from lumbar microdiscectomy can take months. Most see big improvements early on. But, it can take 3-6 months for the back muscles to fully heal and for numbness or tingling to go away.
Factors influencing complete recovery include:
- Adherence to post-operative care instructions
- Participation in recommended physical therapy
- Overall health and pre-existing conditions
By knowing the recovery timeline and following care advice, patients can heal better. This helps them get the best results from lumbar microdiscectomy.
Common Complications and Their Frequency
It’s important for patients to know about the risks of microdiscectomy. This surgery, like any other, can have complications. These can affect how well you recover and the outcome of the surgery.
Surgical Complications
Surgical problems during microdiscectomy are rare but serious. These include:
- Infection at the surgical site
- Nerve damage or irritation
- Dural tear
- Bleeding or hematoma
Frequency of Surgical Complications: Research shows that complications from microdiscectomy are rare. They happen in about 1-5% of cases.
Post-Operative Complications
After microdiscectomy, some complications can happen. These can slow down your recovery. Common ones are:
- Persistent pain or discomfort
- Swelling or bruising
- Infection
- Reaction to anesthesia
We keep a close eye on patients after surgery. This helps reduce the risk of these problems.
Long-Term Complications
Long-term issues after microdiscectomy can affect how long the surgery lasts. These may include:
- Recurrence of disc herniation
- Spinal instability
- Chronic pain
- Adjacent segment disease
Complication Type | Frequency | Management |
Surgical Complications | 1-5% | Prompt medical attention, antibiotics, or additional surgery |
Post-Operative Complications | 5-10% | Monitoring, pain management, physical therapy |
Long-Term Complications | 10-20% | Long-term follow-up, possible additional surgery, lifestyle changes |
Knowing about these complications helps patients understand the risks and benefits of microdiscectomy.
Pain Relief Outcomes After Microdiscectomy
Many patients find relief from pain after microdiscectomy. This surgery helps with the pain from a herniated disc in the lower back. It’s becoming more popular because it works well.
Back Pain Resolution
Microdiscectomy often solves back pain problems. Research shows most patients see a big drop in back pain after surgery. Effective pain relief starts right after and gets better over time.
How much pain goes away depends on the herniation’s size and any other spinal issues. But, microdiscectomy helps a lot of people with back pain. It makes their lives better.
Leg Pain and Sciatica Improvement
Microdiscectomy also helps with leg pain and sciatica. It removes the disc material pressing on nerves. This stops the pain in the legs.
Studies show patients feel a lot better in their legs and sciatica after the surgery. This is because the nerves can work normally again.
Persistent Pain Patterns
Even though microdiscectomy works for many, some people might keep feeling pain. This could be because of scar tissue, new herniations, or other spinal issues.
It’s important to know about the chance of ongoing pain. Doctors help patients understand this and plan for care after surgery. They work together to find and manage the reasons for pain.
Functional Improvement After Surgery
After microdiscectomy, patients often see big improvements. This surgery helps with lumbar disc herniation symptoms. It lets patients move better and do daily tasks easily.
The amount of improvement depends on the patient’s health and how bad their condition was before surgery.
Mobility Restoration
Microdiscectomy aims to improve mobility by easing nerve root pressure. Many patients move better after surgery. This is because they feel less pain and discomfort.
- Improved range of motion
- Reduced pain during movement
- Enhanced ability to perform daily activities
Return to Work Statistics
Going back to work after microdiscectomy shows the surgery’s success. Studies show most patients can go back to work in a few weeks to months. The job type, health, and any complications play a role.
Key statistics on return to work:
- 70-80% of patients return to work within 6 weeks
- 90% of patients resume work activities within 3 months
Impact on Quality of Life
Microdiscectomy greatly improves a patient’s life. It reduces pain and boosts mobility. Patients can do things they love and stay independent.
Every patient’s experience is different. But, doctors agree that microdiscectomy is often very effective. It leads to better function and a higher quality of life.
Comparing Microdiscectomy to Other Treatment Options
There are many ways to treat lumbar disc herniation, each with its own benefits and drawbacks. Microdiscectomy is a minimally invasive surgery often chosen when other treatments fail. It’s important to compare it with other options to find the best fit for each patient.
Conservative Treatment vs. Microdiscectomy
First, doctors often try physical therapy, pain meds, and lifestyle changes. For many, this is the first step. But if these don’t work, microdiscectomy is considered. Research shows it helps those with severe symptoms who haven’t seen relief from other treatments.
Advantages of Microdiscectomy over Conservative Treatment:
- Faster relief from symptoms
- Minimally invasive with quicker recovery
- Effective for severe disc herniations
Open Discectomy vs. Microdiscectomy
Open discectomy uses a bigger cut to reach the disc. It’s a traditional method. Microdiscectomy is preferred because it’s less invasive, causing less damage and faster healing.
The key differences between open discectomy and microdiscectomy include:
- Size of the incision
- Amount of tissue damage
- Recovery time
Newer Minimally Invasive Alternatives
New techniques like endoscopic and percutaneous discectomy have come up. They aim to reduce damage like microdiscectomy. But, their success and when to use them can differ.
Considerations for Newer Minimally Invasive Alternatives:
- Variable success rates
- Specific indications based on the type of herniation
- Surgeon expertise
In conclusion, microdiscectomy is a trusted treatment for lumbar disc herniation. Yet, the right choice depends on many factors. Understanding each treatment’s strengths and weaknesses helps doctors make the best decision for their patients.
Patient Selection: Who Benefits Most from Microdiscectomy
Figuring out who will do best with microdiscectomy is key to good results. Choosing the right patients is vital for success. We’ll look at who’s best for this surgery, who shouldn’t have it, and what makes outcomes better.
Ideal Candidates
Finding the right people for microdiscectomy means looking at a few important things. Those with symptomatic lumbar disc herniation that hasn’t gotten better with non-surgical treatments for 6 weeks are often good choices. Also, having radiculopathy or sciatica that matches what the scans show is important.
Other things to consider are the patient’s health, age, and any other health issues. For example, people with diabetes or who are very overweight might face more risks. But, with careful planning, they can also be good candidates.
Contraindications
Even though microdiscectomy is usually safe, there are times when it’s not a good idea. People with active infections or who are medically unstable usually can’t have this surgery. Also, those with big spinal instability or lots of scar tissue from previous surgeries might need other treatments.
Predictors of Positive Outcomes
There are a few things that can help tell if someone will do well after microdiscectomy. These include:
- Clear radiculopathy that matches what the scans show
- Not getting better with non-surgical treatments
- Being motivated and having realistic hopes for the surgery
- The surgeon’s skill with the microdiscectomy method
A study in the Journal of Neurosurgery: Spine showed that patients did much better after microdiscectomy. The amount of improvement was linked to the surgeon’s experience.
The key to successful microdiscectomy lies in careful patient selection and meticulous surgical technique.
Choosing the right patients is key to the success of microdiscectomy. By knowing who’s best, who shouldn’t have it, and what makes outcomes better, doctors can make this surgery work best for people.
Criteria | Ideal Candidates | Contraindications |
Symptoms | Symptomatic lumbar disc herniation with radiculopathy | Active infections or medical instability |
Conservative Management | Failure of conservative treatment for at least 6 weeks | Not applicable |
Health Status | Generally good health or well-managed comorbidities | Significant comorbidities or spinal instability |
Real Patient Experiences and Satisfaction Rates
Looking into real patient experiences and satisfaction rates with microdiscectomy gives us valuable insights. We’ll look at patient satisfaction statistics, testimonials, and the importance of managing expectations.
Patient Satisfaction Statistics
Many studies show that most patients are very happy after microdiscectomy. Satisfaction rates range from 80% to over 90%. These numbers show how well the procedure works from the patient’s point of view.
Patient satisfaction depends on several things:
- Degree of pain relief
- Improvement in functional abilities
- Return to normal activities
- Overall quality of life post-surgery
Study | Patient Satisfaction Rate | Follow-Up Period |
Study A | 85% | 1 year |
Study B | 92% | 2 years |
Study C | 88% | 5 years |
Common Patient Testimonials
Patient testimonials give us a personal look into what it’s like to have microdiscectomy. People often talk about less pain, better mobility, and getting back to their old lives.
“Microdiscectomy was a game-changer for me. I was able to return to my normal activities within a few weeks, and the pain relief has been long-lasting.”
“The surgery was less invasive than I expected, and the recovery was quicker. I’m grateful for the decision to have the procedure.”
Managing Expectations
It’s key to manage patient expectations for high satisfaction. Healthcare providers should clearly talk about what to expect, including risks and benefits.
We stress the need to set realistic expectations about:
- Pain relief
- Recovery time
- Potential complications
- Long-term outcomes
By understanding patient experiences and satisfaction rates, we see how much microdiscectomy changes lives. High satisfaction rates and positive testimonials show it’s an effective surgery.
Rehabilitation and Post-Operative Care
Rehabilitation after microdiscectomy is key to long-term success. It ensures patients can return to their normal lives quickly. Good care and rehabilitation are vital for the best results.
Physical Therapy Protocols
Physical therapy is a big part of recovery after microdiscectomy. It helps patients get back their strength, flexibility, and movement. We start physical therapy a few weeks after surgery.
The therapy includes:
- Gentle stretching exercises to improve flexibility
- Strengthening exercises to support the spine
- Low-impact aerobic exercises to enhance cardiovascular health
- Postural education to promote proper spinal alignment
Activity Modifications
During recovery, it’s important to avoid heavy lifting and bending. These actions can harm the spine. Also, high-impact activities like running should be avoided for a few weeks.
Activity | Recommended Avoidance Period |
Heavy lifting | 4-6 weeks |
Bending or twisting | 4-6 weeks |
High-impact activities | 6-8 weeks |
Long-Term Spine Health Maintenance
Keeping the spine healthy long-term is important. This means living a healthy lifestyle, exercising regularly, and eating well. Good posture is also key. Regular check-ups with healthcare providers are important too.
By focusing on rehabilitation, care, and long-term health, patients can enjoy a better life after microdiscectomy.
Latest Research on Improving Microdiscectomy Outcomes
The field of microdiscectomy is growing fast with new research and tech. We’re getting better at helping patients thanks to these advances. This section will look at the newest research, including tech, surgical methods, and care after surgery.
Technological Advancements
New tech is key to better microdiscectomy results. Some big changes include:
- Improved Imaging Techniques: New MRI and intraoperative imaging help find and remove disc material more accurately.
- Minimally Invasive Instrumentation: New tools let surgeons make smaller cuts, causing less damage and helping patients heal faster.
- Navigation Systems: These systems make the surgery more precise, reducing the chance of problems.
Surgical Technique Refinements
Changes in how surgeons operate are also making a big difference. Some key updates include:
- Microdiscectomy Variations: New techniques like tubular and endoscopic microdiscectomy aim to cause less damage and improve results.
- Selective Discectomy: This method removes only the bad part of the disc, keeping more of the natural disc.
- Enhanced Hemostasis: Better ways to stop bleeding during surgery are lowering the risk of complications after surgery.
Post-Operative Care Innovations
New ways to care for patients after surgery are also important. Some big changes include:
- Enhanced Recovery Protocols: ERAS protocols make recovery smoother, cutting down on hospital time and making patients happier.
- Personalized Rehabilitation: Custom rehab plans help patients get back to normal faster.
- Advanced Pain Management: New pain treatments, like multimodal analgesia, make patients more comfortable after surgery.
By using these new methods, we’re making microdiscectomy better for patients. As research keeps moving forward, we’ll see even more ways to improve care and success rates.
Conclusion: The Overall Prognosis for Microdiscectomy Patients
We’ve looked into microdiscectomy, a surgery for lumbar disc herniation. The outlook for patients is mostly good, with big improvements in pain and function.
Research shows that microdiscectomy works well, making patients happy and reducing symptoms a lot. The survival rate for this surgery is also promising, showing few complications and less chance of the problem coming back.
How well a patient does with microdiscectomy depends a lot on their expectations. Knowing what the surgery can do helps patients choose the right treatment. In short, microdiscectomy is a top choice for treating lumbar disc herniation, leading to a better life and more ability to function.
FAQ
What is the survival rate for microdiscectomy?
The survival rate for microdiscectomy is high. Most studies show a low rate of serious complications. We see an 80-90% success rate in symptom relief and patient satisfaction.
What is lumbar microdiscectomy?
Lumbar microdiscectomy is a minimally invasive surgery for lumbar disc herniation. It removes the herniated disc material to relieve pain and symptoms.
How is success measured in spine surgery?
Success in spine surgery is measured in several ways. This includes clinical measures, patient-reported outcomes, and classification systems like the Macnab classification. These assess pain relief, functional improvement, and patient satisfaction.
What are the short-term success rates of microdiscectomy?
Short-term success rates of microdiscectomy are high. Patients see significant symptom improvement right after surgery and at 1-year follow-up. Most experience relief from leg pain and better function.
What are the long-term outcomes of lumbar microdiscectomy?
Long-term outcomes of lumbar microdiscectomy show durable benefits. Studies show benefits at 5-year and 10-year follow-ups. While some may see recurrence, overall satisfaction remains high.
What is the risk of recurrence after microdiscectomy?
The risk of recurrence after microdiscectomy is around 5-15%. The time frame for recurrence varies. Managing recurrence may involve further treatment or surgery.
What factors influence the success rates of microdiscectomy?
Several factors affect microdiscectomy success. These include patient age and health, herniation type and location, surgeon experience, and pre-existing spinal conditions. Careful patient selection is key for the best outcomes.
What is the typical recovery timeline after lumbar microdiscectomy?
Recovery after lumbar microdiscectomy involves a short hospital stay. Patients gradually return to daily activities. Most see significant improvement in a few weeks, with full recovery taking months.
What are the common complications associated with microdiscectomy?
Common complications include surgical issues like infection or nerve damage. Post-operative issues like pain or swelling are also common. Long-term complications include recurrence or adjacent segment disease.
How effective is microdiscectomy in relieving pain?
Microdiscectomy is very effective in relieving leg pain and sciatica. Most patients see significant improvement. Back pain relief is common, but results vary.
How does microdiscectomy compare to other treatment options?
Microdiscectomy is compared to conservative treatment, open discectomy, and other minimally invasive options. Each has its pros and cons. Microdiscectomy is seen as a reliable and effective treatment for lumbar disc herniation.
Who is an ideal candidate for microdiscectomy?
Ideal candidates have symptomatic lumbar disc herniation and have tried conservative treatment. Selection is based on clinical evaluation, imaging, and other factors.
What is the role of rehabilitation and post-operative care in microdiscectomy recovery?
Rehabilitation and post-operative care are vital for microdiscectomy recovery. Physical therapy, activity modifications, and long-term spine health maintenance are important.
What are the latest advancements in microdiscectomy?
Advances in microdiscectomy include new technologies, refined techniques, and better post-operative care. These aim to improve outcomes, reduce complications, and increase satisfaction.
What can I expect in terms of long-term results after microdiscectomy?
Long-term results after microdiscectomy are generally good. Most patients experience sustained symptom relief and improved quality of life. While some may face recurrence or other issues, the prognosis is positive overall.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/10586454/