Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
Cancer is a broad term for a class of diseases characterized by the uncontrolled growth of abnormal cells. These cells can invade surrounding tissues and spread to other parts of the body, a process called metastasis. Understanding cancer involves recognizing its many forms and the biological processes that drive it. This overview covers the fundamental nature of cancer, its classification, and the differences between malignant and benign tumors.
The human body is made of trillions of cells that normally grow and divide as needed. When cells become old or damaged, they die, and new cells take their place. Cancer begins when this orderly process breaks down. Genetic changes, or mutations, interfere with these signals, leading to uncontrolled cell growth. These abnormal cells can form a mass of tissue called a tumor.
A tumor can be benign or malignant.

Cancers are classified by the type of cell or tissue where they originate. The main categories include:
Cancer’s signs can be general or specific to the affected organ. Less serious conditions often cause many symptoms. However, recognizing persistent changes and understanding risk factors are key to early detection, which significantly improves treatment outcomes.
While symptoms vary widely by cancer type, some general signs should prompt a medical consultation, especially if they are new or persistent. These include:

Cancer is caused by changes (mutations) to the DNA within cells. These changes can be inherited or acquired. Acquired mutations are far more common and can result from external factors, such as carcinogens, or from random errors during cell division. Often, it is a complex combination of these factors rather than a single cause.
A risk factor is anything that increases the chance of developing a disease.
Send us all your questions or requests, and our expert team will assist you.

A precise cancer diagnosis is essential for creating an effective treatment plan. The process begins with a physical exam and a review of medical history. While imaging tests like CT scans, MRIs, and PET scans provide images of a tumor’s size and location, a biopsy is the definitive diagnostic tool. This involves removing a small tissue sample for a pathologist to examine. Blood tests may also be used to detect tumor markers. This collective data is then used to “stage” the cancer, a critical step that determines the extent of the disease.
When a symptom suggests cancer, a doctor will begin with a thorough physical exam and a review of medical history. If a specific area is suspected, the next step is typically an imaging test to visualize the inside of the body. However, cancer can only be confirmed with a biopsy. This procedure involves a specialist (such as a surgeon or radiologist) taking a sample of the suspicious tissue. A pathologist then analyzes these cells under a microscope to confirm the presence of cancer and identify its specific type.
Doctors use several tools to diagnose cancer and determine if it has spread:
Staging is the process of finding out how much cancer is in the body. The most common system used is the TNM system:
Cancer treatment is highly personalized, based on the specific type, stage, and the patient’s overall health. Treatment plans often use a combination of methods. The primary goal may be curative (to remove all cancer), to control its spread, or palliative (to manage symptoms). These therapies are broadly divided into local treatments, like surgery and radiation, and systemic treatments, such as chemotherapy, which affect the entire body. A multidisciplinary team determines the optimal sequence.


Local treatments target the cancer in a specific part of the body.

Systemic treatments travel through the bloodstream to reach cancer cells throughout the body.

Palliative care is a specialized field focused on improving the quality of life for patients and their families. It is appropriate at any age and at any stage of a serious illness. This type of care focuses on relieving the symptoms and stress of the illness, such as pain, fatigue, and nausea. It can be provided alongside curative treatments.
Choosing a cancer center is a critical decision. At Liv Hospital, our approach is centered on a multidisciplinary “Tumor Board.” This collaborative team, including oncologists, surgeons, and radiologists, reviews each case to create a unified plan. We are committed to using advanced diagnostic technology and offering the latest treatment protocols. Our philosophy extends beyond the disease to holistic care, supporting the patient and their family through every step of this complex journey.
In our center, cancer care is not the responsibility of a single doctor. Our Tumor Board brings together specialists from medical oncology, radiation oncology, surgery, pathology, and radiology. This team collaborates to review complex cases, discuss all possible treatment avenues, and develop a single, comprehensive treatment plan that reflects the collective expertise of multiple disciplines.
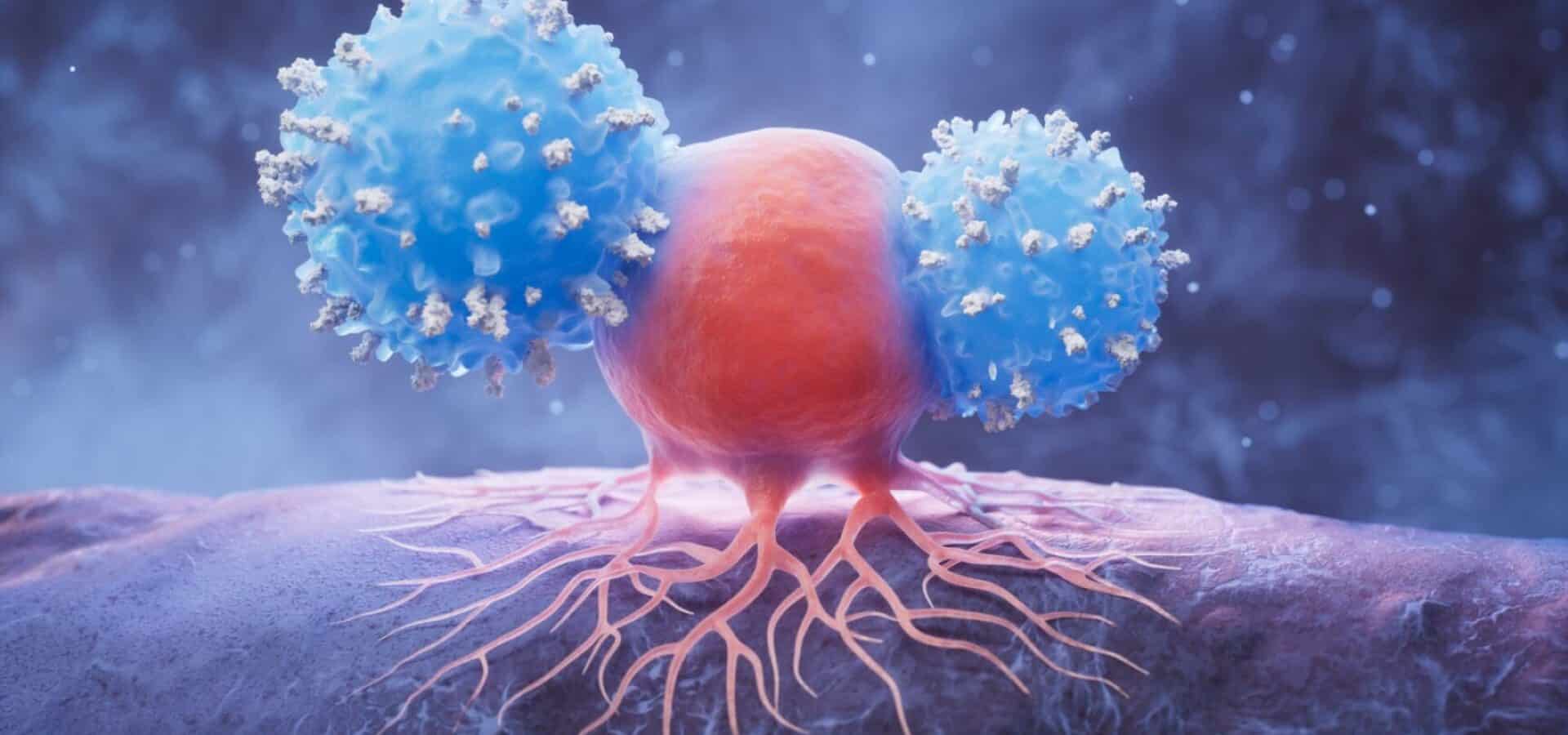
We utilize state-of-the-art technology for both precise diagnosis and effective treatment. This includes high-resolution imaging (such as PET/CT and 3T MRI) for accurate staging, and advanced radiation therapy techniques (like IMRT/VMAT) that target tumors while sparing healthy tissue. Our access to genomic testing also enables the use of targeted therapies and immunotherapies, positioning us at the forefront of personalized medicine.
We understand that a cancer diagnosis affects the entire family. Our commitment to holistic care includes dedicated patient navigators to guide you through the treatment process. We also provide integrated support services, including nutritional counseling to manage side effects, psychological support to address the emotional and mental burden, and palliative care to ensure optimal symptom control and quality of life.
