Last Updated on December 1, 2025 by Bilal Hasdemir

Retinoblastoma is a rare and serious eye cancer that mainly hits young kids. About 300 kids in the United States get it every year. The genetic basis of this disease is well-established, with mutations in the RB1 gene being a significant factor. Knowing what causes retinoblastoma is key to better treatments and better lives for patients.
Research has shown a strong link between main cause of retinoblastoma and the RB1 gene mutation. This means that changes in the RB1 gene can lead to retinoblastoma. This makes genetic screening and counseling very important for families dealing with this disease.
Key Takeaways
- Retinoblastoma is a rare eye cancer that mainly affects children.
- The RB1 gene mutation is a big factor in retinoblastoma.
- Understanding retinoblastoma genetics is key to good treatment.
- Genetic screening and counseling are vital for affected families.
- Research into retinoblastoma causes keeps improving treatment options.
Understanding Retinoblastoma: An Overview

Retinoblastoma is a serious eye cancer in kids. Knowing about it helps doctors treat it better. We’ll look at what it is, how it’s classified, and its spread to get a full picture.
Definition and Classification of Retinoblastoma
Retinoblastoma is a cancer in the retina, mainly in young kids. It comes in two types: hereditary and non-hereditary. The hereditary type is linked to a specific gene mutation, while the non-hereditary type is not.
Knowing the type of retinoblastoma is key for treatment. It can affect one or both eyes, with both-eye cases often being hereditary. This helps doctors plan the best care and watch for it closely.
Key classification factors include:
- Presence of germline or somatic RB1 mutations
- Laterality (unilateral or bilateral)
- Family history of retinoblastoma
Epidemiology and Global Incidence Rates
Studies have shown how common retinoblastoma is worldwide. It’s rare, happening in about 1 in 15,000 to 1 in 20,000 births. But, it’s more common in some places than others.
Here are the global incidence rates of retinoblastoma:
| Region | Incidence Rate |
| North America | 1 in 18,000 live births |
| Europe | 1 in 17,000 live births |
| Africa | 1 in 10,000 live births |
These numbers show we need to focus on different areas for awareness and early detection. By knowing where retinoblastoma is common, we can improve treatment and save more lives.
The Main Cause of Retinoblastoma: RB1 Gene Mutations
Mutations in the RB1 tumor suppressor gene are the main cause of retinoblastoma. The RB1 gene is key for controlling cell growth and division. It acts as a tumor suppressor to stop uncontrolled cell growth.
The Role of the RB1 Gene in Cell Growth Regulation
The RB1 gene makes a protein that controls the cell cycle, mainly at the G1 checkpoint. This protein, called pRb, stops cells from growing too much. It acts as a gatekeeper, ensuring cells divide correctly and damaged cells don’t grow.
In normal cells, the RB1 gene keeps the genome stable by managing genes for DNA replication and cell division. Its proper function is key to stopping tumors, including retinoblastoma.
How RB1 Mutations Lead to Cancer Development
A mutation in the RB1 gene can cause a faulty or non-working pRb protein. This loss of function lets cells grow without control. So, cells with damaged DNA keep dividing, getting more mutations that can cause tumors.
In retinoblastoma, RB1 gene mutations are critical. They mess up cell growth in the retina. This can cause tumors in one or both eyes, depending on the mutation’s spread.
Understanding RB1 gene mutations in retinoblastoma is key for better treatments. By learning about the genetic causes, researchers can find new ways to treat the disease. This could also lower the risk of secondary cancers in survivors.
Hereditary vs. Non-Hereditary Retinoblastoma
It’s important to know the genetic cause of retinoblastoma. It can be hereditary, from germline mutations, or non-hereditary, from somatic mutations. This knowledge helps with genetic counseling, risk assessment, and treatment planning.
Germline Mutations and Familial Patterns
Hereditary retinoblastoma comes from germline mutations in the RB1 gene. These mutations are in every cell and can be passed down from parents. Families often see a pattern of retinoblastoma, showing a strong family link. Germline mutations greatly raise the risk of retinoblastoma, often in both eyes.
Genetic counseling is key for families with germline mutations. We must think about the risk to future generations and the importance of early detection. Early detection and monitoring are critical in managing hereditary retinoblastoma.
- Germline mutations are inherited in an autosomal dominant pattern.
- Families with a history of retinoblastoma should undergo genetic testing.
- Regular screening for retinoblastoma is recommended for individuals with germline RB1 mutations.
Somatic Mutations and Sporadic Cases
Non-hereditary retinoblastoma comes from somatic mutations in the RB1 gene, in just one retinal cell. These mutations are not passed down and usually affect one eye. Somatic mutations are linked to sporadic cases, with no family history of the disease.
Somatic mutations lead to unilateral retinoblastoma, and the risk of passing it to offspring is much lower than with germline mutations. Yet, genetic testing is advised to confirm RB1 mutations.
- Somatic mutations occur post-zygotically, in a single cell.
- Non-hereditary retinoblastoma is typically unilateral.
- Genetic testing can help identify somatic mutations and guide management.
In conclusion, knowing the difference between hereditary and non-hereditary retinoblastoma is vital. It helps us provide the right care and counseling. We must look at the genetic cause to plan treatment and surveillance effectively.
Knudson’s Two-Hit Hypothesis Explained
To understand retinoblastoma, we must explore Knudson’s Two-Hit Hypothesis. This theory, by Alfred Knudson, explains how tumors form. It says two genetic changes, or “hits,” are needed for retinoblastoma to develop.
The Genetic Mechanism Behind Retinoblastoma Development
In families with a history of retinoblastoma, the first mutation is inherited. This mutation is in the RB1 gene. The second mutation happens later, in the eye cells. For those without a family history, both mutations occur in the eye cells after birth.
The Role of the RB1 Gene: The RB1 gene helps control cell growth. Without it, cells can grow out of control, leading to tumors.
Implications for Hereditary and Non-Hereditary Forms
Knudson’s theory helps us understand both types of retinoblastoma. Families with a history of the disease face a higher risk. The disease often affects both eyes. For those without a family history, the risk is less clear. Yet, the theory shows how genetic changes can cause tumors.
“The two-hit hypothesis provides a unifying concept for understanding the genetics of retinoblastoma, highlighting the critical role of the RB1 gene in tumor suppression.” – Alfred Knudson
This theory is more than just a disease explanation. It guides genetic counseling and risk assessment. Knowing the genetic cause helps doctors give better advice to families.
| Characteristics | Hereditary Retinoblastoma | Non-Hereditary Retinoblastoma |
| First Hit | Germline mutation in RB1 gene | Somatic mutation in RB1 gene |
| Second Hit | Somatic mutation in retinal cells | Somatic mutation in retinal cells |
| Laterality | Often bilateral | Usually unilateral |
Genetic Predisposition and Risk Factors
It’s key to spot genetic risk factors early for retinoblastoma. We’ll look into how genetics play a role in this cancer.
Family History as a Primary Risk Factor
A family history of retinoblastoma is a big warning sign. It shows a possible inherited link. People with such a history face a higher risk of getting retinoblastoma. Genetic counseling helps families understand their risk and what it means for their kids.
Research shows many retinoblastoma cases come from a mutated RB1 gene. This gene is passed down in a way that only one copy is needed to raise the risk of retinoblastoma.
Other Genetic Syndromes Associated with Retinoblastoma
Some genetic syndromes raise the risk of retinoblastoma. For example, Li-Fraumeni syndrome, caused by TP53 gene mutations, increases cancer risk, including retinoblastoma. Knowing about these syndromes is vital for early detection and treatment of retinoblastoma.
Genetic predisposition is complex, influenced by many genes and the environment. By grasping these risk factors, we can spot at-risk individuals. Then, we can offer the right watch and care plans.
Why Does Retinoblastoma Occur in Children?
To understand why retinoblastoma happens in kids, we need to look at how the retina grows in the womb and early childhood. The retina starts as a layer of cells in the embryo. It grows into a complex tissue through cell division and differentiation.
Developmental Timing and Cell Division in the Retina
The growth of retinoblastoma is tied to when retinal cells divide. In the womb and early childhood, the retina grows fast to form the vision needed tissue. Any problem in this process, like mutations in the RB1 gene, can cause retinoblastoma. The retina is very sensitive to genetic changes during this time, raising the risk of tumors.
Studies show most retinoblastoma cases are found in kids under five, sometimes at birth. This early detection points to a link with growth processes in the womb and early childhood.
Age Distribution and Onset Patterns
The age when kids are diagnosed with retinoblastoma differs between hereditary and non-hereditary types. Kids with hereditary retinoblastoma are often diagnosed younger and may have both eyes affected. Non-hereditary cases usually happen in older kids and affect one eye more.
Knowing how age and onset patterns of retinoblastoma vary helps us understand the disease better. It also guides us in creating better screening and early detection methods for at-risk kids.
Bilateral Retinoblastoma: Genetic Characteristics
It’s key to know the genetic traits of bilateral retinoblastoma to diagnose and treat it. This eye cancer hits both eyes and often runs in families.
Genetic Basis of Bilateral Disease
Bilateral retinoblastoma is usually tied to RB1 gene mutations. These mutations are in every cell and raise the risk of retinoblastoma, hitting both eyes. This shows why genetic tests and family counseling are vital.
Having a RB1 mutation affects not just the person but also their family. It’s important to do detailed genetic tests to spot at-risk family members. This helps in setting up the right watchful care plans.
Management Considerations for Bilateral Cases
Handling bilateral retinoblastoma needs a detailed plan. This plan considers the disease’s genetics, how far the tumors have spread, and the patient’s health. Treatments might include chemotherapy, laser or cryotherapy, or removing one or both eyes.
The aim is to save vision and life. A team of doctors, including eye specialists, cancer experts, and geneticists, should make treatment plans. Genetic counseling is also key. It helps families understand the risk of it coming back and its impact on future generations.
By grasping the genetic makeup of bilateral retinoblastoma and using a thorough treatment strategy, we can better help patients and their families. This approach improves outcomes for those facing this tough disease.
Environmental and Non-Genetic Risk Factors
Genetic predispositions are not the only risk for retinoblastoma. Environmental exposures and non-genetic factors also play a role. While genetic mutations, like in the RB1 gene, are the main cause, researchers look into other factors.
Parental Age and Possible Environmental Exposures
Older parents might face a higher risk of health issues, including some cancers. Studies suggest that older dads might increase the risk of retinoblastoma in kids. This could be because of genetic mutations in sperm that build up over time.
Exposure to chemicals or radiation might also be a risk. But, more research is needed to confirm this. The exact link between these factors and retinoblastoma is not yet clear.
Key factors being studied include:
- Parental exposure to certain chemicals or toxins
- Advanced parental age, mainly paternal age
- Exposure to ionizing radiation
Current Research on Contributing Factors
Scientists are working hard to understand how environment and non-genetic factors affect retinoblastoma. They use studies to find new risk factors and see how they work with genetics. This research could lead to better ways to prevent and treat retinoblastoma.
The complexity of retinoblastoma development highlights the need for ongoing research into both genetic and non-genetic factors. As we learn more, we might find new ways to lower the risk of this disease and help kids more.
The Molecular Pathogenesis of Retinoblastoma
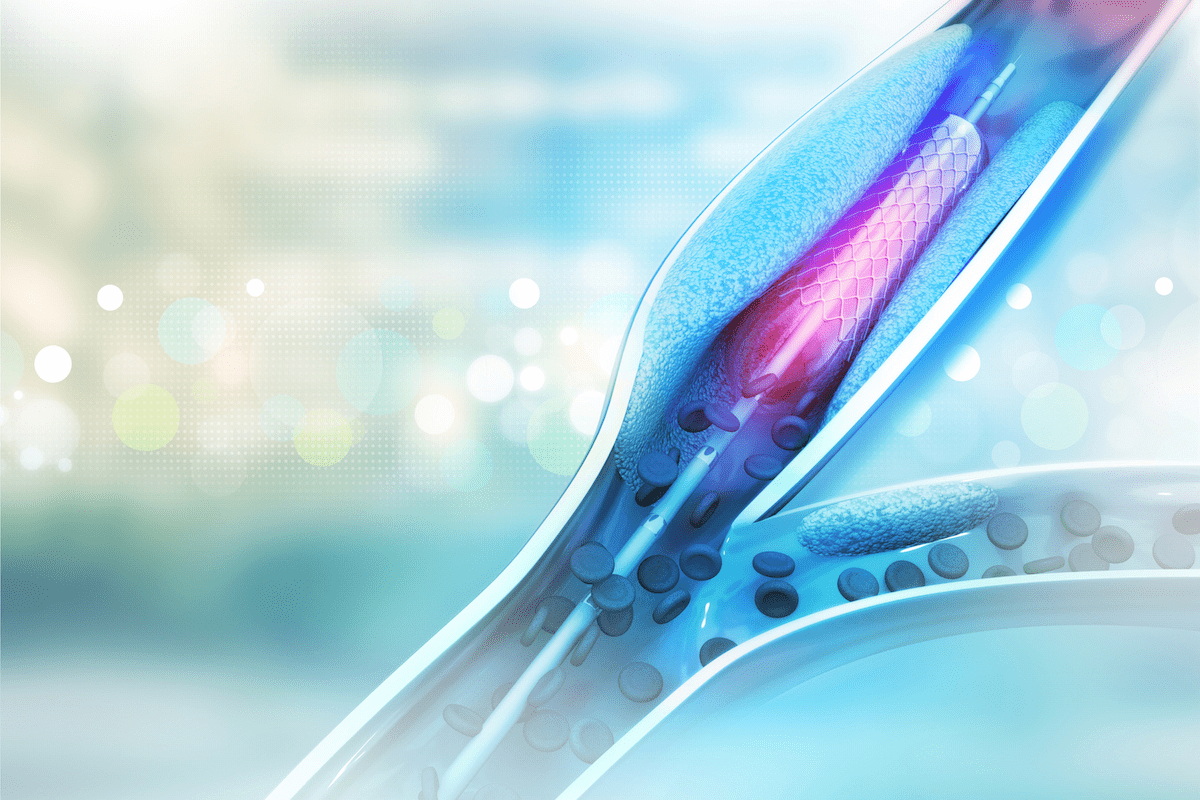
To understand retinoblastoma, we must look at the RB1 gene’s role in cell cycle control. The RB1 gene is a tumor suppressor that keeps cell division in check. Without it, cells can grow out of control, leading to tumors.
Cell Cycle Dysregulation in Tumor Development
The loss of RB1 is key in retinoblastoma. The RB1 protein stops cells from moving into the S phase, where DNA is copied. Without it, cells can divide without control, causing tumors.
Key mechanisms involved in cell cycle dysregulation include:
- Deregulation of E2F transcription factors
- Disruption of normal cell cycle checkpoints
- Increased cell proliferation and survival
Secondary Genetic Changes in Tumor Progression
While the first RB1 mutation starts retinoblastoma, more changes can make tumors worse. These changes affect different pathways, making tumors more varied.
| Genetic Change | Effect on Tumor |
| Mutations in MYCN | Associated with more aggressive tumor behavior |
| Alterations in the PI3K/AKT pathway | May enhance tumor cell survival |
| Changes in genes involved in DNA repair | Can influence treatment response and resistance |
As a study shows,
“The accumulation of secondary genetic alterations in retinoblastoma can significantly impact the clinical outcome and treatment response.”
In summary, retinoblastoma’s molecular pathogenesis involves losing RB1 and then getting more genetic changes. Knowing these steps is key to finding better treatments and helping patients.
Clinical Presentation and Symptoms of Retinoblastoma
Knowing the symptoms of retinoblastoma is key for quick medical help and good treatment. This rare eye cancer mainly hits young kids. It shows signs that are important for catching it early.
Early Warning Signs: Leukocoria and Strabismus
The first signs of retinoblastoma are leukocoria, a white glow in the pupil, and strabismus, or squint. Leukocoria happens when light bounces off a tumor in the eye. Strabismus can come from vision problems caused by the tumor.
Parents or doctors might notice these signs during check-ups. It’s important for parents to watch for these signs and get help if they see anything odd with their child’s eyes.
Advanced Symptoms and Complications
If retinoblastoma isn’t caught early, it can get worse. More serious symptoms include vision loss, eye pain, and in bad cases, the tumor can spread. This can lead to metastasis.
| Symptom | Description | Implication |
| Leukocoria | White pupillary reflex due to tumor reflection | Early sign of retinoblastoma |
| Strabismus | Squint or misalignment of the eyes | Potential vision disruption |
| Vision Loss | Loss of vision due to tumor growth | Advanced disease stage |
Spotting these symptoms early is vital for managing and treating retinoblastoma well. We stress the need for regular eye checks and for parents to be alert. This helps catch it early.
Diagnostic Approaches for Retinoblastoma
Diagnosing retinoblastoma involves several steps. These include imaging, clinical checks, and genetic tests. Getting the diagnosis right is key for good treatment and better patient care.
Imaging Techniques and Clinical Examination
Ultrasound is often the first tool used to check for retinoblastoma. It helps see how big and where the tumor is in the eye. Magnetic Resonance Imaging (MRI) is also important. It looks at the optic nerve and nearby areas for any tumor spread. MRI gives detailed pictures that help in knowing the disease’s stage.
Eye exams under anesthesia are also vital. They include fundoscopy. Fundoscopy lets doctors see the retina and spot any issues, like leukocoria. Leukocoria is a white glow in the eye that can be a sign of retinoblastoma.
Genetic Testing and Counseling
Genetic tests are a big part of diagnosing retinoblastoma. They look for RB1 gene mutations. Finding a mutation confirms the diagnosis and helps families understand their risks. Genetic counseling is given to families with retinoblastoma history to talk about testing.
Genetic testing checks a blood sample or tumor tissue for RB1 gene mutations. If a mutation is found, family members can get tested too. Knowing this helps catch retinoblastoma early in those at risk.
Histology and Pathology of Retinoblastoma
Understanding retinoblastoma’s histology and pathology is key to effective treatment. It’s a complex disease needing a detailed approach for diagnosis and treatment.
Microscopic Features as a Small Round Blue Cell Tumor
Retinoblastoma is a small round blue cell tumor, like neuroblastoma and Ewing’s sarcoma. It has small, round, and densely packed cells with large nuclei and little cytoplasm. This unique look helps tell it apart from other eye tumors.
The tumor cells often form Flexner-Wintersteiner rosettes. These look like normal retinal structures. They help pathologists confirm the diagnosis of retinoblastoma.
Molecular Markers and Diagnostic Criteria
Retinoblastoma is also diagnosed with molecular markers and specific criteria. Finding mutations in the RB1 gene is a key marker. Molecular tests can spot these mutations, aiding in diagnosis and treatment planning.
Diagnosing retinoblastoma involves clinical exams, imaging, and histopathology. Genetic testing is vital for identifying risk and managing the disease. This approach helps tailor treatments for better patient outcomes.
Treatment Modalities Based on Genetic Profile
Genetic profiling is key in finding the best treatments for retinoblastoma. It helps doctors create treatment plans that fit each patient’s needs.
Current Treatment Approaches
Doctors use a mix of treatments for retinoblastoma. Chemotherapy helps shrink tumors. Then, local treatments like laser therapy or cryotherapy can target the tumor more precisely. Radiation therapy is used in more serious cases or when there’s a high chance of the tumor coming back.
- Chemotherapy to shrink tumors
- Local treatments for precise tumor control
- Radiation therapy for advanced or high-risk cases
The right treatment depends on many things. These include the disease’s stage, the tumor’s genetic profile, and the patient’s health. Personalized medicine is becoming more important. It helps tailor treatments for better results.
Personalized Medicine in Retinoblastoma Management
Personalized medicine uses the tumor’s genetic info to choose treatments. This way, doctors pick the best therapies and avoid unnecessary ones. It can lead to fewer side effects and better results.
“The integration of genetic profiling into clinical practice has revolutionized the management of retinoblastoma, enabling more precise and effective treatment strategies.”
Expert Opinion
As research gets better, we’ll see even more improvements in treating retinoblastoma. Genetic profiling will keep playing a big role in making treatment choices.
Retinoblastoma Prognosis and Survival Rates
Retinoblastoma’s prognosis and survival rates change a lot based on several important factors. Knowing these factors helps patients, families, and doctors make better treatment choices.
Factors Affecting Prognosis
Many things can change a retinoblastoma patient’s outlook. These include the stage of the disease when it’s found, genetic mutations, and how well the first treatment works. Getting diagnosed early is key to a better chance of survival.
Having an RB1 gene mutation is a big deal. People with hereditary retinoblastoma, caused by a germline RB1 mutation, face a different future than those without it.
| Factor | Impact on Prognosis |
| Stage at Diagnosis | Early-stage diagnosis improves survival rates |
| Genetic Mutations | Presence of RB1 mutation affects prognosis |
| Treatment Response | Positive response to initial treatment improves prognosis |
Secondary Cancer Risks in Survivors with RB1 Mutations
People who survive retinoblastoma and have RB1 mutations are more likely to get other cancers. This is a big thing to think about when caring for retinoblastoma survivors long-term.
“The risk of secondary cancers in survivors of hereditary retinoblastoma highlights the need for lifelong monitoring and full care.”
— Expert in Retinoblastoma
Prevention Strategies and Future Research Directions
Genetic counseling and new technologies are helping us fight retinoblastoma better. We’re learning more about the disease’s genes. This knowledge helps us support families at risk and lower the cancer’s rate.
Genetic Counseling for High-Risk Families
Genetic counseling is key for families with retinoblastoma history. It helps find people with the RB1 mutation. This way, families can plan and watch for signs early.
For families at risk, counseling talks about reproductive choices. It includes options like preimplantation genetic diagnosis (PGD). PGD checks embryos for the RB1 mutation before they’re used, helping avoid the mutation.
Emerging Technologies in Early Detection and Prevention
New tools are changing how we find and prevent retinoblastoma. Next-generation sequencing (NGS) makes genetic tests faster and more accurate. Wide-field retinal imaging also helps spot tumors early.
New biomarkers and research into retinoblastoma’s biology are on the horizon. These could lead to better treatments and outcomes for patients.
It’s vital to keep funding research on retinoblastoma prevention and early detection. By using genetic counseling, new tech, and understanding the disease, we can improve care for those with retinoblastoma.
Conclusion: Understanding the Etiology of Retinoblastoma
Knowing how retinoblastoma starts is key to better treatments and better patient care. We’ve looked into the genetic roots of retinoblastoma. This includes how the RB1 gene controls cell growth and how mutations cause cancer.
It’s important to know if retinoblastoma runs in families or not. This knowledge helps with genetic advice and risk checks. More research is needed to find new ways to treat retinoblastoma.
By learning about what causes retinoblastoma, we can help patients and their families more. Our goal is to provide top-notch healthcare and support for patients from around the world. Raising awareness about retinoblastoma is a big part of this mission.
FAQ
What is retinoblastoma?
Retinoblastoma is a rare eye cancer in kids. It happens because of genetic changes, mainly in the RB1 gene.
What is the main cause of retinoblastoma?
The main cause is mutations in the RB1 gene. This gene helps control how cells grow and divide.
What is the difference between hereditary and non-hereditary retinoblastoma?
Hereditary retinoblastoma comes from inherited RB1 gene mutations. It often runs in families. Non-hereditary retinoblastoma is caused by mutations in one eye only.
What is Knudson’s two-hit hypothesis?
Knudson’s theory says two genetic changes are needed for retinoblastoma. In hereditary cases, the first change is inherited. In non-hereditary cases, both changes happen in one eye.
Why does retinoblastoma predominantly occur in children?
It mainly affects kids because their retina is most active during fetal and early childhood. This makes it more prone to mutations.
What are the early warning signs of retinoblastoma?
Look out for a white glow in the pupil (leukocoria) and squinting (strabismus).
How is retinoblastoma diagnosed?
Doctors use ultrasound, MRI, and fundoscopy to diagnose. They also test for RB1 gene mutations.
What are the treatment modalities for retinoblastoma?
Treatments include chemotherapy, radiation, and local therapies. Personalized treatment plans are becoming more common.
What is the prognosis for retinoblastoma patients?
The outcome depends on several factors, including RB1 mutations. Those with these mutations face a higher risk of other cancers.
How can retinoblastoma be prevented?
Prevention includes genetic counseling for at-risk families. New detection and prevention technologies are also being developed.
What is the genetic basis of bilateral retinoblastoma?
Bilateral retinoblastoma often comes from inherited RB1 gene mutations.
Are there any environmental risk factors associated with retinoblastoma?
Some studies suggest advanced parental age and certain exposures might increase risk. More research is needed to confirm this.
References
- MacCarthy, A., Birch, J. M., Draper, G. J., Kroll, M. E., & Vincent, T. J. (2009). Risk of subsequent primary neoplasms in survivors of retinoblastoma: a systematic review and meta-analysis. British Journal of Cancer, 100(12), 1875-1883.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3365233/