Last Updated on November 27, 2025 by Bilal Hasdemir
Prostate cancer is a common issue for men, with over 200,000 new cases in the U.S. each year. Treatment options vary, and prostate cancer treatment often includes surgery. But is this surgery considered minor or major?
Dealing with prostate surgery can be scary. It’s a big decision that needs careful thought and understanding. Prostate surgery is performed to address conditions such as cancer, BPH, and prostatitis.
Understanding prostate surgery is key. It’s important to know its role in treating prostate problems. We’ll give you an overview of what to expect and its implications.
The prostate gland is key to men’s health. Surgery is needed for some issues. This includes prostate cancer and benign prostatic hyperplasia (BPH).
The prostate gland is small, like a walnut, and sits below the bladder in men. It surrounds the urethra. It’s vital for the male reproductive system, producing seminal fluid to nourish sperm.
Several conditions may need prostate surgery. Prostate cancer is a big concern, often treated with removing the prostate gland. Other issues include benign prostatic hyperplasia (BPH) and prostatitis, an inflammation.
Surgeries like transurethral resection of the prostate (TURP) help with BPH. Knowing about these conditions and treatments is key for prostate health.
It’s important for patients and doctors to know what major prostate surgery is. It’s about complex surgeries that remove a lot of tissue or need big repairs. These surgeries also have big risks.
Major surgery is very invasive and needs a long time to recover. It also has big risks for the patient. For prostate surgery, it means removing the prostate gland or a big part of it.
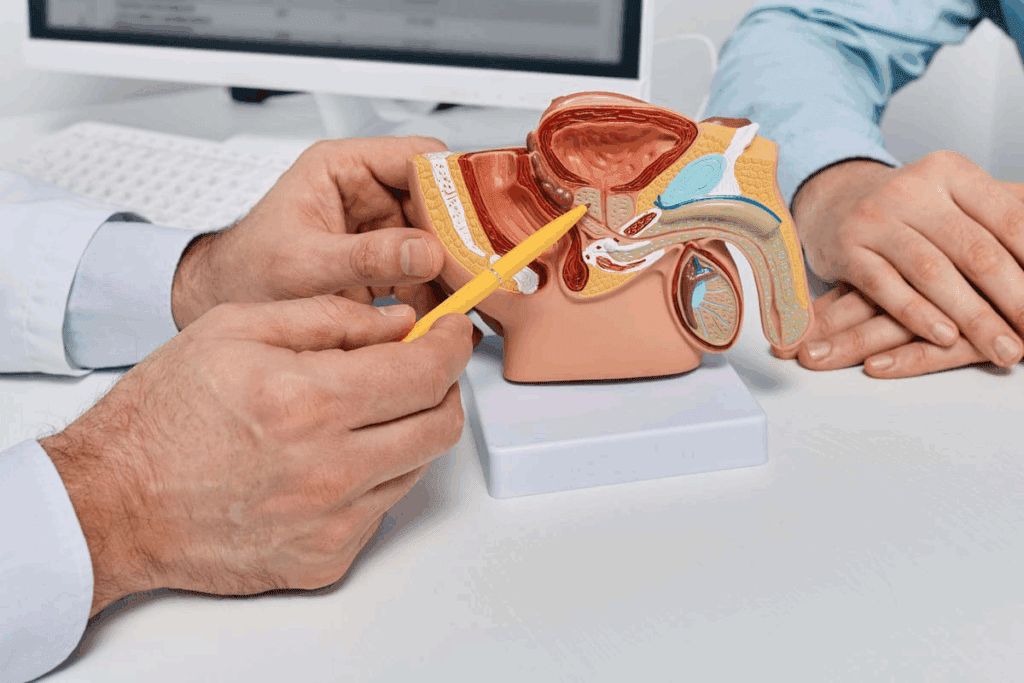
Radical prostatectomy is a major surgery. It removes the prostate gland, seminal vesicles, and nearby tissue. It’s often done for prostate cancer.
The complexity of prostate surgery depends on several things. These include how much tissue is removed, if reconstruction is needed, and the risk of bleeding. More invasive surgeries, like open prostatectomies, are more complex and riskier.
These factors make the surgery more complex. They also affect the surgical complication risks.
The hospital stay duration after major prostate surgery varies. It depends on the surgery’s complexity and the patient’s health. Usually, patients stay in the hospital for several days.
| Procedure | Typical Hospital Stay |
| Radical Prostatectomy | 2-3 days |
| Open Prostatectomy | 3-5 days |
Knowing about recovery and possible complications helps manage patient expectations. It also improves care after surgery.
Prostate surgery includes many procedures, each for different conditions. The right surgery depends on health, condition, and the doctor’s advice.
A radical prostatectomy removes the prostate gland. It’s mainly for prostate cancer. The surgeon takes out the gland, seminal vesicles, and some tissue. There are open, laparoscopic, and robotic-assisted ways to do it.
Transurethral Resection of the Prostate (TURP) treats an enlarged prostate. It removes tissue blocking urine flow. This method is less invasive than radical prostatectomy and helps with BPH symptoms.
TURP is done under anesthesia. A resectoscope is inserted through the urethra to remove tissue. It aims to improve urine flow and reduce symptoms.
There are more prostate surgeries, like:
Each procedure has its own use, benefits, and risks. The right one depends on the condition, health, and what the patient prefers.
For men with prostate cancer, radical prostatectomy is a big surgery that might cure them. It removes the prostate gland and nearby tissues. It’s a key treatment for prostate cancer that hasn’t spread.
Doctors suggest radical prostatectomy for men with cancer in the prostate. The choice to have surgery depends on the cancer’s stage and grade, the patient’s health, and their wishes.
Key indications for radical prostatectomy include:
The radical prostatectomy procedure is complex. Surgeons must carefully remove the prostate gland while preserving surrounding nerves and tissues to minimize the risk of complications. The surgery can be performed using different techniques, including open surgery, laparoscopic surgery, or robotic-assisted surgery.
The nerve-sparing approach is a key part of radical prostatectomy. It tries to keep nerves that help with erections intact. This reduces the chance of erectile dysfunction after surgery. The success of nerve sparing depends on the patient’s age, the extent of nerve damage during surgery, and the surgeon’s expertise.
Having a radical prostatectomy can be scary. But, with better surgery techniques and care after surgery, many men recover well. They can go back to their usual activities.
Choosing between open prostate surgery and minimally invasive methods is a big decision. It depends on the patient’s health, the cancer stage, and the surgeon’s skills.
Open prostate surgery uses a big incision in the belly to reach the prostate. It’s been around for a long time. It’s often chosen for more serious cases or when other options fail.
Advantages: This method gives direct access to the prostate. It’s a tried-and-true technique with a long history.
Laparoscopic prostatectomy is a minimally invasive surgery. It uses small cuts for instruments and a camera to remove the prostate. It’s less invasive and leads to faster recovery.
Benefits: It causes less blood loss, pain, and hospital time than open surgery. The small cuts also mean less scarring.
The surgery’s invasiveness and recovery time are key for patients. Open surgery is more invasive and takes longer to recover. But, laparoscopic surgery is quicker.
| Surgical Aspect | Open Prostate Surgery | Laparoscopic Prostatectomy |
| Invasiveness | More invasive, larger incision | Less invasive, smaller incisions |
| Recovery Time | Typically longer | Generally shorter |
| Blood Loss | More significant | Less |
| Hospital Stay | Longer stays are common | Shorter stays are typical |
The choice between open surgery and laparoscopic prostatectomy depends on the patient’s situation. It’s based on their prostate condition and health.
Robotic prostate removal with the Da Vinci System is a big step in urology. It combines precision with less invasiveness. This technology has changed prostate surgery, giving patients a better and less invasive option.
The Da Vinci System is a top-notch robotic platform. It lets surgeons do complex surgeries with better precision and control. During a robotic prostate removal, the surgeon uses a console to control robotic arms with surgical tools.
This setup allows for precise dissection and removal of the prostate gland. It also helps in minimizing damage to nearby tissues and nerves.
The robotic system’s high-definition 3D visualization gives a clear view of the surgical site. This helps the surgeon to navigate complex anatomy with more accuracy. This precision is key in keeping urinary and sexual function intact after surgery.
Robotic-assisted surgery, like with the Da Vinci System, has many benefits. These include:
While robotic prostate removal has many benefits, it has its limits. The availability and cost of robotic surgery can be a big factor. Not all healthcare facilities have the Da Vinci System. Also, the surgeon’s expertise in robotic surgery is key to a successful procedure.
Patients should talk to their healthcare provider about their situation. It’s important to understand the surgical complication risks and how robotic-assisted surgery reduces them. This helps in making an informed decision.
Before prostate surgery, patients go through a detailed evaluation. This includes checking surgical risks and picking the right anesthesia. This careful planning is key to the best results.
Prostate surgery can use different anesthetics. These include general anesthesia, regional anesthesia (like spinal or epidural), and local anesthesia with sedation. The choice depends on the patient’s health, surgery complexity, and personal preferences.
General anesthesia makes the patient sleep through the surgery. Regional anesthesia numbs the lower body. Local anesthesia with sedation is less common but might be used for simpler procedures.
The pre-surgery evaluation is a vital step. It includes a detailed medical history, physical check-up, and diagnostic tests. These help assess the patient’s health and spot any risks.
We thoroughly review the patient’s medical history. This helps us find any conditions that might impact the surgery or anesthesia. Conditions like heart disease, diabetes, or past surgery problems are checked.
Some factors can make prostate surgery harder. These include being older, overweight, smoking, and having health issues like high blood pressure or heart disease. Finding these risks early helps us take steps to reduce them.
Knowing about anesthesia types, the evaluation process, and risk factors helps us prepare patients better. This improves their surgery outcomes.
Knowing how long you’ll stay in the hospital after prostate surgery is key. The time you spend there depends on the surgery type, your health, and any surgery complications.
The surgery type greatly affects how long you’ll stay in the hospital. For example:
Several things can make your hospital stay longer after prostate surgery, including:
Understanding these factors helps you prepare for your hospital stay and recovery. Always follow your doctor’s advice and go to all follow-up appointments for a smooth recovery.
After prostate surgery, patients go through several recovery phases. These phases range from immediate care to long-term healing. Knowing this timeline helps manage expectations and eases the recovery journey.
The first 24 to 48 hours after surgery are critical. Patients are closely watched for any issues. Pain management is a top priority to keep them comfortable.
In this time, patients are usually in the hospital. The medical team looks for signs of bleeding, infection, or other problems. They may feel pain, discomfort, or trouble urinating, which are managed with medication.
In the first few weeks, patients slowly get back to normal. They should avoid heavy lifting, bending, or strenuous exercises. Most can start with light activities in 1 to 3 weeks, depending on their health and surgery type.
During this time, some may experience urinary incontinence or erectile dysfunction. These symptoms usually get better with time and proper management.
Long-term recovery can take months. Patients continue to heal and their body functions return to normal. We recommend a healthy lifestyle, including a balanced diet and regular exercise, to aid in recovery.
Most men can get back to their normal activities in 3 to 6 months. But, full recovery, including urinary and sexual function, can take up to a year or more.
To better understand the recovery process, let’s look at a general timeline for prostate surgery patients:
| Recovery Stage | Typical Duration | Key Activities/Expectations |
| Immediate Post-Operative | 1-2 days | Hospital stay, pain management, monitoring for complications |
| Short-term Recovery | 1-3 weeks | Gradual return to light activities, avoiding heavy lifting or strenuous exercises |
| Long-term Recovery | 3-6 months (up to 1 year or more for full recovery) | Continued healing, return to normal activities, improvement in urinary and sexual function |
Throughout recovery, following your healthcare provider’s instructions is key. Also, attending follow-up appointments is vital for a smooth and effective recovery.
It’s important to know the risks and complications of prostate surgery. This knowledge helps you make better choices. Prostate surgery, like any big surgery, can have risks that affect your recovery and life quality.
Urinary incontinence is a big risk with prostate surgery. It can be stress incontinence, where you leak urine when you cough or sneeze. Or it can be urge incontinence, where you really need to go fast. The risk depends on the surgery type and your health before surgery.
Risk Factors for Urinary Incontinence:
Erectile dysfunction (ED) is another risk of prostate surgery. The chance of ED changes based on the surgery, the surgeon, and your health before surgery. Using nerve-sparing techniques can lower this risk.
Factors Influencing Erectile Dysfunction:
Other risks include infection, bleeding, and damage to nearby organs. These are less common but serious.
| Complication | Description | Management |
| Infection | Bacterial infection post-surgery | Antibiotics |
| Bleeding | Excessive bleeding during or after surgery | Transfusion, surgical intervention |
To manage and lower risks, you need a good pre-surgery check-up. Choosing the right surgery and post-care is also key. Talk to your surgeon about your specific risks.
“The key to minimizing complications is a thorough pre-surgical evaluation and choosing a surgeon with extensive experience in prostate surgery.” – Expert in Urology
Knowing these risks and how to lessen them helps you make smart choices about your care.
Understanding the costs of prostate surgery is key. It’s a big part of treating prostate cancer. Knowing the financial side is important for patients and their families.
The cost of prostate surgery changes a lot. It depends on the procedure, the surgeon’s fees, hospital costs, and where you are. Radical prostatectomy, for example, is a big surgery with big costs.
| Procedure | Average Cost | Insurance Coverage |
| Radical Prostatectomy | $20,000 – $40,000 | Majority covered by insurance |
| TURP | $10,000 – $20,000 | Generally covered |
| Robotic Prostatectomy | $25,000 – $50,000 | Often covered, check with provider |
In the U.S., most insurance plans cover prostate surgery. This includes radical prostatectomy and other treatments. But, how much they cover can differ a lot.
It’s vital for patients to check their insurance before surgery. Knowing what you’ll pay out of pocket, deductibles, and any pre-approval needs is key.
If you’re struggling financially, there are help options. Non-profit organizations and patient advocacy groups offer support. They help with the financial side of prostate surgery.
We know medical costs can be tough to handle. We aim to help by sharing info on costs and insurance. This way, patients can make better choices about their care.
Choosing the right surgeon and hospital for prostate surgery is key. Your outcome can be greatly affected by their expertise. It’s important to make informed decisions about your care.
Your surgeon’s experience is critical for a successful prostate surgery. An experienced prostate surgeon has done many surgeries. This means they have better skills and results.
Look at these factors when checking a surgeon’s experience:
It’s important to talk to your surgeon before deciding. Here are some questions to ask:
These questions help you understand your surgeon’s approach. This way, you can make a better decision about your care.
Conclusion
Prostate surgery is a complex treatment for prostate issues, like cancer. We’ve looked at different surgeries, like radical prostatectomy and TURP. We also talked about what makes a surgery major.
Knowing about prostate cancer treatment and recovery is key for patients. Advances in surgery, like robotic-assisted methods, have made recovery faster and better for many.
In conclusion, choosing prostate surgery requires careful thought. It involves looking at the surgery type, possible complications, and recovery. With the right information and healthcare team, patients can face their surgery with confidence and hope for the best results.
Prostate surgery is done to treat prostate issues, like cancer. Some surgeries are minor, but others, like radical prostatectomy, are major. This is because of their complexity and how invasive they are.
There are several prostate surgeries. These include radical prostatectomy, Transurethral Resection of the Prostate (TURP), and robotic surgery with the Da Vinci System. Each has its own use and benefits.
Radical prostatectomy is a big surgery for prostate cancer. It removes the prostate gland. It’s for those with localized cancer who can handle surgery.
Open surgery uses a big cut, while laparoscopic surgery uses small cuts. Laparoscopic surgery usually means less blood loss, less pain, and a quicker recovery.
Robotic surgery uses the Da Vinci System. A surgeon controls robotic arms for the surgery. It offers better precision, less blood loss, and a faster recovery.
Risks include urinary problems, erectile issues, and infections. A good pre-surgery check and a skilled surgeon can lower these risks.
Stay time varies by procedure and patient. Most stay one to three days after surgery.
Recovery starts right after surgery. It takes weeks for short-term recovery and months for long-term. Most can get back to normal in a few weeks to months.
Costs depend on the surgery, location, and insurance. In the U.S., insurance often covers necessary procedures. There are also financial help options.
Look at the surgeon’s experience and the hospital’s reputation. Make sure they offer advanced technologies like robotic surgery. Ask about their success rates.
This technique tries to keep nerves around the prostate during surgery. It helps keep urinary and erectile functions.
Complications include urinary issues, erectile problems, and infections. To manage these, a thorough check before surgery, careful surgery, and good care after are key.
Cambridge University Hospitals. Bladder Care and Management https://www.cuh.nhs.uk/patient-information/bladder-care-and-management/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!