Last Updated on December 2, 2025 by Bilal Hasdemir
Melanoma in the head and neck region is a big worry. It makes up about 30 percent of all melanoma cases globally. We stress the need for early detection and treatment. The 5 key signs of malignant melanoma on head and neck, including the critical importance of recognizing the ABCDE rule.
Melanoma is a skin cancer that happens when cells called melanocytes change and grow too much. The American Cancer Society says there will be about 100,640 new melanoma cases in 2024.
At Liv Hospital, we have top experts in oncology, dermatology, and surgical oncology. They work together to care for patients with melanoma on the head.
Key Takeaways
- Melanoma is a serious type of skin cancer.
- The head and neck region is a common area for melanoma to occur.
- Early detection is key for effective treatment.
- Liv Hospital offers complete care for melanoma patients.
- A team of specialists works together to provide personalized treatment plans.
The Alarming Rise of Head and Neck Melanoma
Recent studies show a sharp rise in melanoma in the head and neck area. This is not just a number; it’s a call to action. We need to be more aware and quick to diagnose and treat melanoma in this key area.
30% of Melanomas Occur in Head and Neck Region
The head and neck are common places for melanoma to develop. About 30% of all melanomas happen here. The American Cancer Society says melanoma can pop up anywhere, but it’s more common in sun-exposed spots like the head and neck.
| Body Region | Percentage of Melanomas |
| Head and Neck | 30% |
| Other Body Areas | 70% |
5% Annual Increase Over Past 30-40 Years
The rate of head and neck melanoma has been going up by about 5% each year for 30 to 40 years. This steady rise shows how vital it is to know the risks and find melanoma early, like melanoma on the neck and other head and neck spots.
This trend is alarming and needs our immediate focus. The growing number of melanoma neck cases calls for a strong push towards education and prevention.
As we watch this trend, it’s key to stress the importance of checking yourself and getting checked by a doctor early. This is even more important in high-risk spots like the back of the neck.
Why Malignant Melanoma on Head and Neck Is More Dangerous

The head and neck area is special because of its anatomy. It has a lot of blood vessels and lymphatic channels. These factors make malignant melanoma on the head more dangerous.
Rich Vascularization and Lymphatic Drainage
The head and neck have lots of blood vessels and lymphatic channels. This helps melanoma cells spread quickly. So, melanomas here are more likely to spread to other parts of the body.
“The rich vascular supply and lymphatic drainage of the head and neck region contribute to the aggressive behavior of melanoma,” says a leading oncologist. This is why melanoma on the head often has a worse prognosis.
Increased Risk of Metastasis
Melanoma on the head and neck is more likely to spread. This is a big worry because it makes treatment harder and the outlook worse. Catching it early is key to stopping it from spreading.
- Rich vascular supply facilitates the spread of melanoma cells.
- Extensive lymphatic drainage increases the risk of metastasis.
- Early detection is critical to prevent metastasis.
Poorer Prognosis Compared to Other Body Sites
Research shows that forehead melanoma and other head and neck melanomas have a worse outlook. This is mainly because of the area’s rich blood and lymphatic systems.
It’s important for both patients and doctors to understand this. Being careful and getting quick medical checks is key when you notice strange spots on your head or neck.
Key Sign #1: Asymmetrical Lesions
Asymmetrical lesions are a key sign of malignant melanoma on the head and neck. The ABCDE rule helps identify melanoma by looking for asymmetry. This rule says “A” for asymmetry, meaning one half of a mole doesn’t match the other.
What Asymmetry Looks Like in Head and Neck Melanomas
Asymmetry in head and neck melanomas looks different in various areas. For example, on the scalp, an asymmetrical melanoma might look like an irregular mole. On the face, it might show up as color or texture differences in the lesion.
Asymmetry is not just about shape; it also includes color, elevation, or texture differences. These irregularities are important signs that a mole might be dangerous.
How to Evaluate Asymmetry in Different Head Regions
Checking for asymmetry needs a careful look. On the scalp, use a mirror or ask someone to help. For facial melanomas, a simple look can show asymmetry.
- Use good lighting to illuminate the area.
- Compare both halves of the mole or lesion.
- Look for irregularities in shape, color, or texture.
Common Asymmetrical Patterns in Scalp vs. Facial Melanomas
Asymmetry is a concern in both scalp and facial melanomas. But, they look different. Scalp melanomas often have irregular borders. Facial melanomas might show varied colors due to sun exposure.
“The asymmetry of a melanoma can be a subtle yet critical warning sign. Early detection relies on recognizing these irregularities.”
Knowing these differences helps catch melanomas early and treat them effectively.
Key Sign #2: Border Irregularity
Malignant melanomas often have irregular borders. This is key when checking lesions on the scalp, face, and neck. The “B” in the ABCDE rule means the edges are not smooth. This is important for catching dangerous lesions early.
Characteristics of Irregular Borders
Irregular borders in melanomas can look different. They might be ragged or notched. Sometimes, they can be blurred, making it hard to see where the lesion starts and ends.
When we check a lesion, we look for uneven edges. Benign lesions have clear edges. But melanomas have uneven edges, which means they might be cancerous.
Differences Between Scalp, Facial, and Neck Melanoma Borders
The look of border irregularity changes based on where the melanoma is. On the scalp, it’s harder to see because of the hair. Facial melanomas are easier to spot. Melanomas on the back of the neck can be tricky because they might not be noticed until they grow a lot.
It’s important to know these differences for early detection. Scalp melanomas are often found later because their borders are hidden by hair.
When Border Changes Signal Danger
Changes in border irregularity can mean the melanoma is getting worse. If a stable lesion starts to have more irregular edges, it might be turning aggressive. Watching for these changes is vital.
It’s good to check yourself and get a doctor’s opinion regularly. This helps catch melanomas early, which is very important for treating them, even more so for head and neck melanomas.
Key Sign #3: Color Variations
The ‘C’ in the ABCDE rule stands for color, which is key in diagnosing melanoma. When checking lesions on the head and neck, look for uneven shades and colors. These can signal malignant melanoma.
Concerning Color Patterns in Head and Neck Melanomas
Melanomas on the head and neck often show a mix of colors. You might see shades of brown, black, and sometimes red or pink. These color changes can show how aggressive the lesion is.
Multiple colors within a lesion are a red flag for melanoma. It’s important to watch for any color changes over time.
Region-Specific Color Presentations
Different areas of the head and neck show different color patterns. This is because of skin tone and sun exposure differences. For example, melanomas on the scalp might look different from those on the face or neck.
Knowing these regional differences is key for accurate diagnosis.
Differentiating from Normal Pigmentation and Age Spots
It’s important to tell the difference between benign pigmentation and melanoma. Benign age spots usually have one color and clear borders. Melanomas, on the other hand, have multiple colors and irregular borders.
| Characteristic | Benign Lesion | Melanoma |
| Color | Uniform | Multiple colors |
| Border | Clear | Irregular |
| Size | Small, stable | Large, growing |
Key Sign #4: Diameter and Elevation Changes
The fourth key sign in identifying malignant melanoma involves monitoring diameter and elevation changes. As we explore the critical indicators of melanoma on the head and neck, understanding size and elevation changes is vital for early detection.
Size Thresholds That Warrant Concern
The “D” in the ABCDE rule stands for diameter, indicating a spot larger than 6 millimeters might be cancerous. We should be cautious about any new or changing lesions that exceed this size. It’s essential to measure lesions accurately and monitor any changes over time.
| Diameter Size | Level of Concern | Recommended Action |
| <6 mm | Low | Regular monitoring |
| 6 mm – 10 mm | Moderate | Dermatological examination |
| >10 mm | High | Immediate dermatological evaluation |
Elevation and Texture Changes
Changes in elevation and texture are also critical indicators of melanoma. Lesions that become raised or develop uneven surfaces warrant closer examination. We should be aware of any new symptoms such as itching, bleeding, or pain, as these can be associated with more aggressive melanomas.
Monitoring Growth Patterns in Hard-to-See Areas
Monitoring growth patterns in areas like the scalp can be challenging. We recommend regular self-examinations using mirrors and, if possible, having a partner or family member check hard-to-see areas. Photography can also be a useful tool for tracking changes over time.
By being vigilant about diameter and elevation changes, we can improve our chances of detecting melanoma on the head and neck at an early stage, when it is more treatable.
Key Sign #5: Evolving Lesions and Symptomatic Changes
The “E” in the ABCDE rule stands for evolving, showing how important it is to watch moles change over time. For head and neck skin cancer, evolving lesions are a big warning sign. We’ll look at why evolution is key, symptoms to watch for, and when changes are concerning.
Evolution as a Critical Warning Sign
Evolution means any change in a mole’s size, shape, or color. This could be growth, darkening, or texture changes. It’s vital to keep an eye on moles on the head and neck for these signs of melanoma on the neck or other head areas.
Regular self-examinations are essential for catching these changes early. Use a mirror and, if needed, ask someone to check hard-to-see spots like the scalp.
Associated Symptoms
Some malignant melanomas on the neck may also cause symptoms like bleeding, itching, or pain. These symptoms are concerning and need immediate doctor’s attention.
- Bleeding or oozing from a mole
- Itching or tenderness around a mole
- Pain or discomfort in a mole
Timeline of Concerning Changes
How fast changes happen can vary a lot from person to person. Some melanomas grow quickly in weeks, while others change slowly over months or years.
| Change Type | Timeline | Concern Level |
| Rapid growth or darkening | Weeks to months | High |
| Gradual change in shape or color | Months to years | Moderate to High |
| New symptoms (bleeding, itching, pain) | Anytime | High |
High-Risk Locations for Malignant Melanoma on Head
Knowing where malignant melanoma often appears on the head is key to catching it early. This cancer can show up anywhere on the head, but some spots are more likely to grow fast or have worse signs. These signs, like Breslow thickness and mitotic rates, affect how well a person will do.
Scalp Melanoma: Higher Breslow Thickness and Mitotic Rates
Scalp melanomas are a big worry because they tend to grow deeper and faster. The Breslow thickness shows how deep the cancer has grown. A higher thickness means a worse outlook. The mitotic rate, or how fast cells are dividing, also matters a lot. Scalp melanomas usually have a higher rate, showing they’re more aggressive.
A study in the Journal of the American Academy of Dermatology found scalp melanomas are thicker than others. This makes checking the scalp very important during doctor visits.
Temple and Facial Melanoma Characteristics
Melanomas on the temple and face have their own traits. The temple gets a lot of sun, which increases the risk of melanoma. Facial melanomas can be hard to spot because of the face’s complex shape and many harmless spots.
These melanomas often have uneven edges and colors. This makes the ABCDE rule useful for spotting them. The temple’s flat shape makes it harder to notice changes in size and shape early on.
“The diagnosis of melanoma on the face can be challenging due to the presence of numerous benign lesions. A high index of suspicion and thorough examination are critical.” – Medical Expert, Dermatologist
Back of Neck and Forehead Melanoma Concerns
The back of the neck and forehead are also at high risk for melanoma. They get a lot of sun, which can cause damage and lead to melanoma. The back of the neck is hard to check by yourself, so getting help or regular doctor visits is key.
| Location | Risk Factors | Detection Challenges |
| Scalp | Higher Breslow thickness, mitotic rates | Hidden by hair, difficult self-examination |
| Temple/Face | High sun exposure, complex anatomy | Distinguishing from benign lesions |
| Back of Neck/Forehead | Sun exposure, difficult self-examination | Less visible, requires partner-assisted checks |
In summary, knowing about the risks and signs of melanoma on the head is essential for catching it early. Regular self-checks, doctor visits, and knowing the high-risk spots can greatly improve treatment outcomes.
Self-Examination Techniques for Head and Neck Areas
Checking your head and neck for melanoma on the head and melanoma on neck is key. Doing this regularly can spot problems early. This could lead to better treatment results.
Using Mirrors and Photography for Difficult-to-See Areas
It’s hard to see some parts of your head and neck. Mirrors can help. Use a handheld mirror with a wall mirror to see better. This way, you can check the back of your neck and scalp.
Also, taking photos of these spots can track changes. This makes spotting new or growing lesions easier.
Photography tips: Use bright light and a camera with a good sensor. Take clear, close-up photos. Keep the angle and distance the same for comparison.
Partner-Assisted Examination for Scalp and Back of Neck
Getting help from a partner is great for hard-to-reach spots like the scalp and back of the neck. A partner can do a better job of checking these areas. They look for signs of head melanoma like new moles or changes in existing ones.
It’s important to talk clearly about what to look for and how to do it gently but thoroughly.
Recommended Frequency and Documentation Methods
Do self-exams once a month to be effective. Keeping records is also key. Write down and photograph any changes. This helps track your skin’s history and informs your doctor.
- Use a calendar reminder to schedule self-exams.
- Keep a notebook or digital file for your findings.
- Share your records with your doctor at check-ups.
By using these self-exam methods, you can help keep your skin healthy. You might catch melanoma on the head or melanoma on neck early.
Diagnosis and Treatment Approaches
It’s important to know how to diagnose and treat head and neck melanoma. We’ll look at the different ways to find and treat this condition. This way, patients get the best care possible.
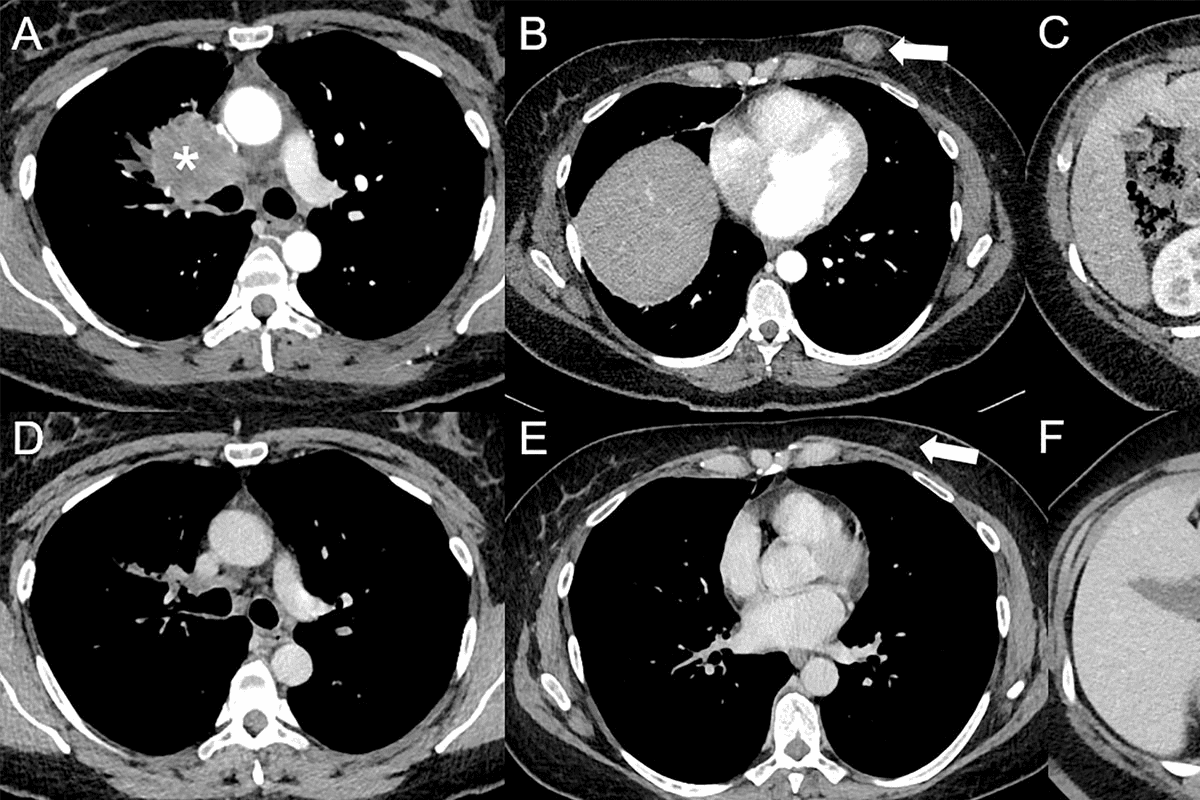
Diagnostic Procedures Specific to Head and Neck Melanoma
To diagnose melanoma on the head and neck, doctors use several methods. They start with a clinical exam. This helps them check the lesion’s shape, color, size, and how it looks.
Biopsy is key to finding out if it’s cancer. They take a piece of the lesion to look at under a microscope. For head and neck melanomas, they might use excisional biopsy or incisional biopsy, depending on the size and where it is.
Treatment Options Based on Location and Stage
The treatment for head and neck melanoma depends on the stage, location, and the patient’s health. Surgical excision is often the first step. It aims to remove the tumor and some healthy tissue around it.
- For early-stage melanomas, surgery might be enough.
- For more advanced cases, treatments like adjuvant therapy (immunotherapy or targeted therapy) might be needed to lower the chance of it coming back.
Reconstructive Considerations for Head and Neck Region
The head and neck area is complex and important for how we look and function. Reconstructive surgery is vital to fix how things look and work after removing the tumor. They use different methods, from simple stitches to more complex grafts or flaps.
We work with patients to find the best way to fix things. We think about how it will look and how it will work. This way, we make sure patients get care that covers everything, not just the cancer.
Conclusion: Early Detection and Professional Evaluation
Early detection and professional evaluation are key to better outcomes for head and neck melanoma patients. We’ve talked about the signs that need attention, like asymmetrical shapes and color changes. Also, look out for lesions that grow or change shape.
Knowing these signs and the risks of head and neck melanoma can help a lot. Regular self-checks and doctor visits are vital, even more so for those at high risk.
Understanding head melanoma helps us catch it early. This knowledge lets us act fast if we see something odd. It leads to better treatment results.
If you’re worried about a mole or lesion on your head or neck, see a doctor. Their skills are essential for diagnosing and treating melanoma right.
FAQ
What are the most common locations for malignant melanoma on the head and neck?
Malignant melanoma can appear in many places on the head and neck. High-risk spots include the scalp, temple, face, back of the neck, and forehead. Each area has its own traits that can affect how melanoma is found and treated.
How can I identify asymmetrical lesions on my head or neck?
Look for moles or marks that are not symmetrical. If you draw a line through the middle, the two sides won’t match. Asymmetry is a key sign of melanoma, even in hard-to-see spots like the scalp.
What does border irregularity in melanoma look like?
Border irregularity means the edges of a mole or lesion are not smooth. They might be notched, ragged, or blurred. This can vary in different areas, like the scalp, face, or neck.
Are color variations always a sign of melanoma?
Color variations can be a sign of melanoma, but not all changes mean cancer. Look out for multiple colors or uneven color in a lesion. It’s important to tell these changes apart from normal skin color and age spots.
How can I monitor diameter and elevation changes in lesions on my head or neck?
Check your skin regularly, using mirrors and photography to track changes. Measure the size of lesions and note any increases. Also, watch for elevation or texture changes, as these can be signs of melanoma.
What are the symptoms associated with evolving lesions?
Evolving lesions might bleed, itch, or hurt. These changes can happen over time and may mean melanoma is getting worse. It’s important to watch for these symptoms, even in high-risk spots.
How often should I perform self-examinations for head and neck melanoma?
Do self-exams monthly, using mirrors and photography for hard-to-see areas. Getting help from a partner can be useful for spots like the scalp and back of the neck. Keeping a record of your findings helps track changes.
What diagnostic procedures are used for head and neck melanoma?
To diagnose head and neck melanoma, doctors use visual checks, dermoscopy, and biopsies. These methods help find out if melanoma is present and how far it has spread, guiding treatment choices.
What are the treatment options for head and neck melanoma?
Treatment for head and neck melanoma varies based on the location, stage, and other factors. It might include surgery, lymph node removal, and reconstructive surgery. Other treatments, like immunotherapy or targeted therapy, might also be considered.
Why is early detection critical for malignant melanoma on the head and neck?
Early detection is key because it greatly improves treatment success. Melanoma on the head and neck is more dangerous because of its blood and lymph system connections. Recognizing key signs and knowing high-risk areas helps catch it early.
References
- National Center for Biotechnology Information. (2025). 5 Key Signs of Malignant Melanoma on Head. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513248/