Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects millions of women worldwide. It is marked by multiple follicles on ovaries. This condition is a major cause of infertility and irregular periods. Getting a PCOS diagnosis can feel overwhelming, but with the right care, Understanding the significance of many follicles on ovaries in a diagnosis of Polycystic Ovary Syndrome.
At Liv Hospital, we offer expert, patient-centered care. We help women understand their diagnosis and create a personalized treatment plan. Our team of specialists will work with you to address both your reproductive and metabolic health. We use the latest medical evidence and innovative healthcare practices.
Key Takeaways
- PCOS is a common endocrine disorder affecting reproductive-aged women.
- The presence of multiple follicles in the ovaries is a hallmark of PCOS.
- PCOS can cause irregular menstrual cycles and excess androgen levels.
- Understanding PCOS is key to managing symptoms and improving overall health.
- Personalized treatment plans can help address reproductive and metabolic health.
Understanding PCOS: A Common Endocrine Disorder

PCOS is a key health issue for women, affecting many in their reproductive years. It’s a complex condition with hormonal imbalances, ovulation issues, and multiple ovarian follicles or cysts.
Definition and Prevalence
PCOS affects hormone levels, ovulation, and has multiple ovarian follicles. It’s found in 5% to 26% of women of childbearing age. In the U.S., it’s estimated that 6% to 12% of women in this age group have PCOS.
The varying prevalence rates come from different diagnostic criteria. The Centers for Disease Control and Prevention say PCOS is a top cause of female infertility, affecting about 1 in 10 women.
Impact on Women’s Health
PCOS affects more than just reproductive health. It also raises the risk of insulin resistance, type 2 diabetes, and heart disease. It can also lead to anxiety and depression.
The hormonal imbalances in PCOS cause symptoms like irregular periods, excess hair, and acne. These symptoms can greatly impact a woman’s life, making early diagnosis and treatment vital.
| Health Aspect | Impact of PCOS | Prevalence |
|---|---|---|
| Reproductive Health | Infertility, irregular menstrual cycles | High |
| Metabolic Health | Insulin resistance, type 2 diabetes | Moderate to High |
| Mental Health | Anxiety, depression | Moderate |
It’s vital to understand PCOS fully to provide the best care for those affected. Recognizing its prevalence and impact helps healthcare providers improve women’s lives.
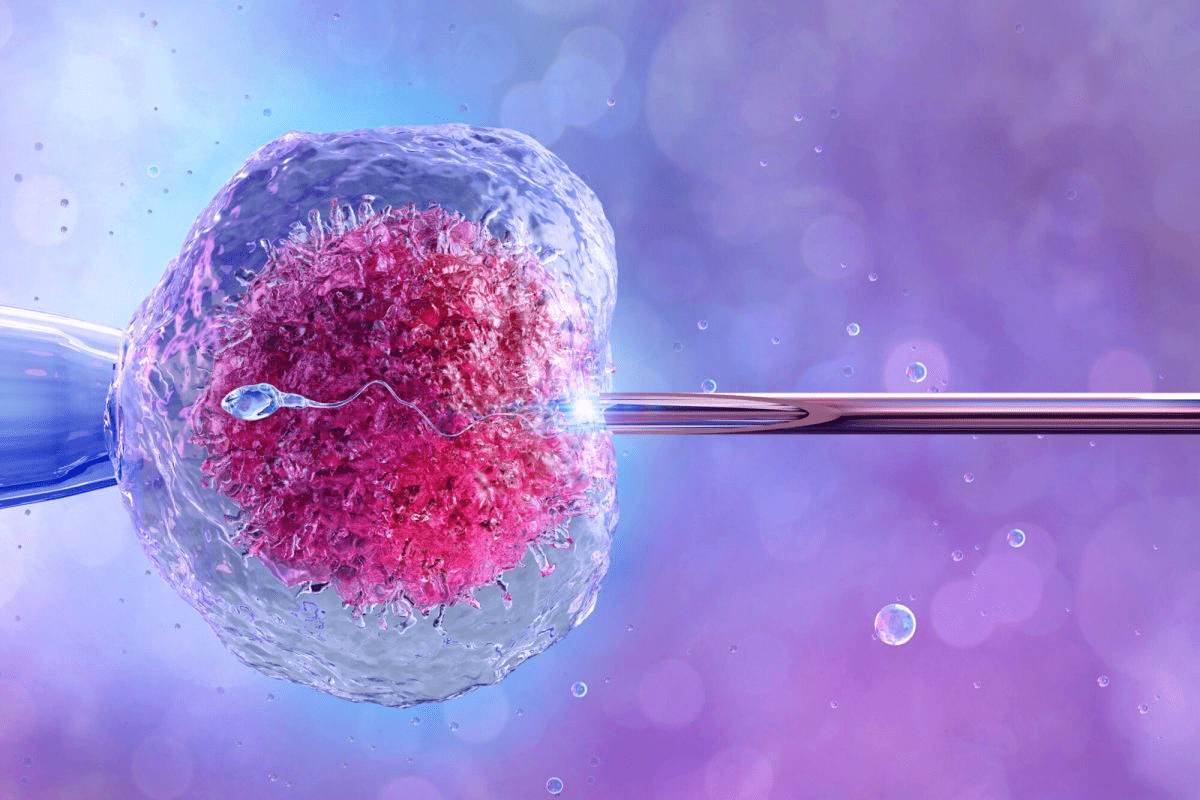
Many Follicles on Ovaries: The Hallmark of PCOS

In PCOS, the ovaries have many follicles that don’t mature right. This is a key sign of the disorder. It affects how well a woman can ovulate and get pregnant.
Normal Follicle Development
Normally, follicles in the ovaries grow and mature in a set order. Each month, several start to grow, but only one becomes the egg-releasing follicle. The others stop growing and are absorbed by the body.
This process is key for regular periods and being able to get pregnant. Hormones like FSH and LH control how follicles grow. In a normal cycle, these hormones work together to help follicles mature and ovulate.
How PCOS Disrupts Follicular Growth
In PCOS, this balance is broken. Many immature follicles build up in the ovaries instead of growing normally. This usually happens because of hormonal imbalances, like too much LH compared to FSH.
The ovaries in PCOS often have small peripheral follicles. These are found around the edges of the ovaries and can be seen with ultrasound. Having these follicles on both ovaries is a common sign of PCOS.
This problem with follicle growth causes ovulation issues. This leads to trouble getting pregnant and other symptoms of PCOS. Knowing how this works is key to managing the condition.
- Multiple immature follicles in the ovaries
- Hormonal imbalances affecting follicular development
- Ovulation problems leading to infertility
Spotting these signs helps doctors diagnose and treat PCOS better. We’ll look at more about how to diagnose and manage PCOS in the next parts.
Diagnostic Criteria for PCOS
It’s important to know the diagnostic criteria for PCOS to manage this common disorder well. The diagnosis involves clinical, hormonal, and ultrasound findings.
Rotterdam Criteria
The Rotterdam criteria, set in 2003, are key for diagnosing PCOS. A diagnosis is made if a person has at least two of three features. These are oligo-anovulation, clinical or biochemical hyperandrogenism, and polycystic ovaries seen on ultrasound. The presence of multiple bilateral ovarian follicles is a key finding.
- Oligo-anovulation: Infrequent or absent ovulation
- Clinical or biochemical hyperandrogenism: Excess androgen levels or symptoms like hirsutism
- Polycystic ovaries on ultrasound: Presence of bilateral ovarian follicles, typically 12 or more follicles in each ovary
Androgen Excess and PCOS Society Criteria
The Androgen Excess and PCOS Society criteria, from 2006, focus on hyperandrogenism. PCOS is diagnosed when there’s hyperandrogenism and either oligo-anovulation or polycystic ovaries on ultrasound. This shows how androgen excess is key in PCOS.
Recent Updates in Diagnostic Standards
Recent updates in diagnostic standards have brought new tech to ultrasound. Transvaginal ultrasound now better spots polycystic ovary follicles. Now, having 20 or more follicles in one or both ovaries is seen as PCOS. These changes show how our understanding of PCOS is growing.
Diagnosing PCOS is tricky because it can show up in many ways. But, by using clinical checks, hormone tests, and advanced imaging, doctors can now accurately diagnose and treat PCOS.
Identifying Polycystic Ovarian Morphology
Healthcare providers use ultrasound to check for polycystic ovarian morphology. This method is key to spotting the signs of polycystic ovaries.
Ultrasound Imaging Techniques
Ultrasound is a safe way to see the ovaries and their follicles. There are two main types: transvaginal and transabdominal ultrasound.
Transvaginal vs. Transabdominal Ultrasound
Transvaginal ultrasound is better for looking at the ovaries because it gives a clearer view. Transabdominal ultrasound is used when the other isn’t possible.
The choice between these methods depends on the patient’s comfort and the situation.
What Doctors Look For: Follicle Count and Size
Doctors check the number and size of follicles in the ovaries. In polycystic ovaries, there are 12 or more small follicles measuring 2-9 mm in diameter. They look for multiple bilateral ovarian follicles as a key sign.
Counting and measuring follicles is important for diagnosing polycystic ovarian morphology. Here’s what doctors look for during ultrasound:
| Feature | Normal Ovaries | Polycystic Ovaries |
|---|---|---|
| Follicle Count | Typically fewer than 12 | Usually 12 or more |
| Follicle Size | Varied, often larger | Typically 2-9 mm in diameter |
| Ovarian Volume | Normal size | Often enlarged |
By looking at these features, doctors can accurately diagnose polycystic ovarian morphology. They can then plan the right treatment.
Types of Follicular Patterns in PCOS
PCOS is marked by specific follicular patterns. These include small peripheral follicles and multiple bilateral ovarian follicles. These patterns are key to understanding PCOS and its effects on women’s health.
Small Peripheral Follicles in Ovaries
One key feature of PCOS is the presence of small peripheral follicles in the ovaries. These follicles are found at the ovary’s edge, resembling a “string of pearls” on ultrasound. “The presence of multiple small follicles in the ovaries is a hallmark of PCOS,” experts say.
Multiple Bilateral Ovarian Follicles
Women with PCOS often have multiple bilateral ovarian follicles. This means both ovaries are affected. The number of follicles can vary, but seeing a dozen or more in each ovary is common. This is a key sign of PCOS.
Distinguishing Between Normal and PCOS Follicles
It’s important to tell normal ovarian follicles from those in PCOS through ultrasound. In PCOS, follicles are smaller and more numerous, often stuck in development. As one study found,
“The diagnosis of PCOS is supported by the presence of 20 or more follicles in either ovary, or an ovarian volume greater than 10 mL.”
Knowing these differences is vital for accurate diagnosis and treatment planning.
By recognizing PCOS’s unique follicular patterns, healthcare providers can better diagnose and manage it. This improves outcomes for women with this common endocrine disorder.
Hormonal Imbalances Affecting Follicular Development
Hormonal issues, like too much androgens and insulin resistance, play a big role in PCOS. These problems stop follicles from growing and maturing properly. This leads to many small follicles in the ovaries.
We will look at how these hormonal problems affect follicle growth in PCOS. We will focus on three main areas: too much androgens, insulin resistance, and an abnormal LH/FSH ratio.
Elevated Androgens and Their Effects
PCOS is often marked by high androgen levels. High androgens mess with normal follicle growth. This stops follicles from fully developing and prevents ovulation.
- Increased androgen production by the ovarian stroma and adrenal glands
- Peripheral conversion of androgens to estrogens, further disrupting the hormonal balance
- Androgen-induced changes in the follicular microenvironment, impairing follicle maturation
A study found that high androgens in PCOS are not just a sign. They also help cause the syndrome. This shows how hormonal imbalances and follicle growth are linked in PCOS.
Insulin Resistance and Follicular Development
Insulin resistance is a big problem in PCOS, affecting follicle growth and ovulation. Insulin resistance leads to too much insulin, which makes androgen levels go up. This messes with how the ovaries work.
The link between insulin resistance and follicle growth is complex:
- Too much insulin makes the ovaries produce more androgens
- Insulin resistance stops follicles from maturing and ovulating
- Drugs that make the body more sensitive to insulin can help women with PCOS ovulate and get pregnant
LH/FSH Ratio Abnormalities
The LH/FSH ratio is often off in PCOS, causing hormonal and follicular problems. An elevated LH/FSH ratio is common in PCOS. It messes with follicle growth and ovulation.
A study found that an abnormal LH/FSH ratio in PCOS affects follicle development and ovulation. It shows how important hormonal balance is for reproductive health.
We’ve seen how hormonal imbalances, like too much androgens, insulin resistance, and an abnormal LH/FSH ratio, affect follicle growth in PCOS. Understanding these factors is key to finding good treatments for women with PCOS.
Common Symptoms Beyond Ovarian Changes
PCOS is not just about ovarian changes. Women with PCOS often face many other symptoms that affect their daily life. These symptoms can differ from person to person, showing how PCOS can affect everyone differently.
Menstrual Irregularities
Menstrual irregularities are a big sign of PCOS. Women with PCOS might have infrequent or prolonged menstrual periods. This can cause a lot of stress and impact their daily routines.
These irregularities can vary a lot. Some women might not get their period at all, while others might get it too infrequently. These issues are not just annoying; they can also lead to serious health problems like endometrial hyperplasia.
Hirsutism and Skin Changes
Hirsutism, or too much hair growth on the face and body, is common in PCOS. It can really affect a woman’s self-esteem and how she sees her body. This happens because of the high androgen levels in PCOS.
Women with PCOS might also have acne and skin changes. These skin problems are linked to the hormonal imbalances and insulin resistance found in PCOS. To manage these symptoms, it’s important to tackle the hormonal and metabolic issues at the root.
Weight Management Challenges
Many women with PCOS find it hard to manage their weight. This is because of the metabolic and hormonal issues in PCOS. Insulin resistance, a common problem in PCOS, can cause weight gain and make losing weight tough.
To manage weight in PCOS, a complete plan is needed. This includes changing what you eat, being more active, and sometimes getting medical help. By tackling these weight challenges, women with PCOS can improve their health and lower the risk of related problems.
PCOS and Fertility Challenges
PCOS and fertility are closely linked, with many factors affecting ovulation. It’s a common cause of female infertility, impacting ovulation and pregnancy risks.
Impact of Immature Follicles on Ovulation
Women with PCOS often have many follicles on their ovaries. These follicles are usually immature and can’t release an egg. This is a key step for getting pregnant.
PCOS also causes hormonal imbalances. This affects how eggs are released from the ovaries. It can lead to cycles where no egg is released, making it hard to get pregnant naturally.
Pregnancy Complications Associated with PCOS
Women with PCOS face higher risks of pregnancy problems. These include gestational diabetes, high blood pressure, and miscarriage. The presence of many follicles can make these risks worse by altering the hormonal balance needed for a healthy pregnancy.
| Pregnancy Complication | Description | Risk Level in PCOS |
|---|---|---|
| Gestational Diabetes | High blood sugar levels during pregnancy | High |
| Hypertension | High blood pressure during pregnancy | High |
| Miscarriage | Loss of pregnancy before 20 weeks | Moderate to High |
Fertility Treatment Options
There are many fertility treatments for women with PCOS. These aim to regulate ovulation and boost conception chances.
Some common treatments include:
- Medications like clomiphene citrate to induce ovulation
- Lifestyle changes, such as diet and exercise, to improve insulin sensitivity
- Assisted reproductive technologies (ART) like in vitro fertilization (IVF)
Understanding PCOS fertility challenges and exploring treatment options can help women conceive and have a healthy pregnancy.
Long-term Health Risks of Untreated PCOS
Untreated PCOS can lead to serious health problems. We will discuss the risks and why early treatment is key.
Metabolic Syndrome and Diabetes
Women with PCOS face a higher risk of metabolic syndrome. This includes high blood pressure, high blood sugar, and more. It also raises the risk of type 2 diabetes and heart disease.
Key components of metabolic syndrome include:
- Insulin resistance
- Hypertension
- Dyslipidemia
- Obesity, mainly around the waist
| Metabolic Syndrome Component | Risk Factor for Women with PCOS | Potential Complication |
|---|---|---|
| Insulin Resistance | High | Type 2 Diabetes |
| Hypertension | Elevated | Cardiovascular Disease |
| Dyslipidemia | Common | Atherosclerosis |
| Central Obesity | Prevalent | Metabolic Syndrome |
Cardiovascular Disease Risk
PCOS increases the risk of heart disease. This is due to high blood pressure, bad cholesterol, and insulin resistance.
Women with PCOS need to manage these risks through lifestyle changes and medical help.
Endometrial Cancer Concerns
Untreated PCOS raises the risk of endometrial cancer. This is because of unbalanced estrogen levels. Women with PCOS, and those with irregular periods, should talk to their doctor about this risk.
Preventive measures may include:
- Regular check-ups
- Hormonal treatments to regulate menstrual cycles
- Lifestyle changes to manage weight and insulin resistance
In conclusion, untreated PCOS can lead to serious health issues. These include metabolic syndrome, heart disease, and endometrial cancer. Early treatment is vital to prevent these problems. Women with PCOS should work with their doctors to manage their condition.
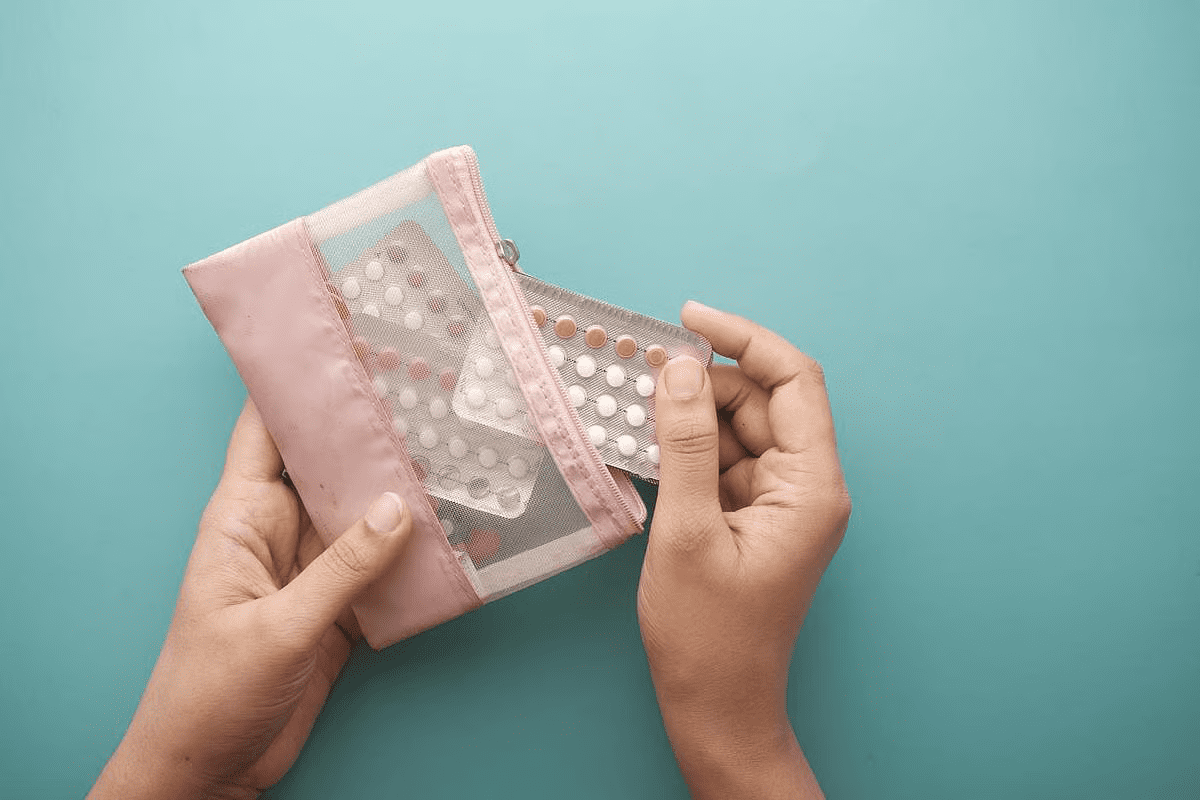
Medical Management of PCOS
PCOS treatment often includes hormonal therapies, insulin-sensitizing drugs, and sometimes surgery. These treatments aim to ease symptoms, enhance quality of life, and prevent future health issues linked to PCOS.
Hormonal Treatments
Hormonal treatments are a common first step in managing PCOS. Birth control pills help regulate menstrual cycles and lower androgen levels. This can improve symptoms like excessive hair growth and acne. For those wanting to get pregnant, fertility medications like clomiphene or letrozole can help induce ovulation.
“Hormonal contraceptives can also regulate menstrual cycles and lower the risk of endometrial hyperplasia and cancer in women with PCOS,” studies show.
Insulin-Sensitizing Medications
Many women with PCOS have insulin resistance, which raises the risk of type 2 diabetes. Metformin is a medication that helps improve insulin sensitivity. It can also aid in weight management and may help with ovulation.
Metformin is beneficial for women with PCOS who are trying to conceive. It can improve ovulation rates and lower the risk of early pregnancy loss.
Surgical Interventions
Surgical options are sometimes considered for women with PCOS, mainly for those trying to conceive. Ovarian drilling involves making small holes in the ovaries to stimulate ovulation. It’s not a first choice but can be effective for some.
PCOS treatment is tailored to each woman’s needs, considering her symptoms, reproductive goals, and health. This personalized approach helps manage symptoms and reduces the risk of future health problems.
Lifestyle Modifications for PCOS Management
Lifestyle changes are key to easing PCOS symptoms and boosting health. Managing PCOS well means using medicine, making lifestyle changes, and getting support.
Nutrition Strategies
Eating a balanced diet is vital for PCOS management. Focus on whole foods like veggies, fruits, whole grains, lean proteins, and healthy fats. These foods help control blood sugar and insulin levels, which PCOS often disrupts.
Stay away from sugary drinks and foods with lots of saturated and trans fats. Eating foods high in fiber can help with weight and insulin sensitivity.
| Nutritional Element | Benefit for PCOS | Food Examples |
|---|---|---|
| Fiber | Improves insulin sensitivity | Whole grains, fruits, vegetables |
| Lean Protein | Supports weight management | Chicken, fish, legumes |
| Healthy Fats | Regulates hormones | Nuts, seeds, avocados |
Exercise Recommendations
Exercise is a key part of managing PCOS. It improves insulin sensitivity, lowers androgen levels, and aids in weight loss. Aim for a mix of cardio and strength training to build muscle and boost metabolism.
Even moderate exercise, like brisk walking, can help a lot. The goal is to find fun and lasting activities.
Stress Management and Sleep
Stress can worsen PCOS symptoms, so managing stress is important. Yoga, meditation, and deep breathing can help. Also, getting enough sleep is key for hormone balance and health.
“Stress management is not just about reducing stress, but about creating a lifestyle that promotes overall well-being.” – Expert in Women’s Health
By making these lifestyle changes, women with PCOS can manage their symptoms better. It’s about making lasting changes for better health and well-being.
Conclusion: Living Well with PCOS
Women with PCOS can live healthy and fulfilling lives. Early diagnosis and proper treatment are key. Making lifestyle changes also helps a lot.
Managing PCOS means tackling hormonal imbalances and ovulation issues. It also means dealing with metabolic risks. Knowing about PCOS and its impact on ovaries helps women make better choices.
With the right care and lifestyle changes, women with PCOS can feel better. They can also improve their chances of getting pregnant. We urge women to work with their doctors to create a plan that fits their needs.
FAQ
What is PCOS and how does it relate to many follicles on ovaries?
PCOS, or Polycystic Ovary Syndrome, is a hormonal disorder. It causes irregular periods and high androgen levels. Many follicles in the ovaries are a key sign of PCOS, seen on ultrasound.
What are the diagnostic criteria for PCOS?
Doctors use several criteria to diagnose PCOS. These include clinical signs, hormone levels, and ultrasound findings. The Rotterdam and Androgen Excess criteria are common standards.
How does PCOS disrupt normal follicle development?
PCOS stops follicles from growing right. Hormonal imbalances, like high androgens and insulin resistance, are key. This leads to many immature follicles.
What is the role of ultrasound imaging in diagnosing PCOS?
Ultrasound, like transvaginal ultrasound, finds many small follicles in PCOS. Doctors count and measure follicles to help diagnose.
What are the common symptoms associated with PCOS beyond ovarian changes?
Symptoms of PCOS include irregular periods, excess hair, skin changes, and weight issues. These symptoms can greatly affect a woman’s life.
How does PCOS affect fertility?
PCOS often leads to infertility due to ovulation problems. Immature follicles make it hard to get pregnant. Hormonal treatments can help.
What are the long-term health risks associated with untreated PCOS?
Untreated PCOS raises the risk of metabolic syndrome, heart disease, and endometrial cancer. Early treatment is key to avoiding these risks.
What are the treatment options for managing PCOS symptoms?
Treatments for PCOS include hormonal therapies, medications, and surgery. Lifestyle changes like diet, exercise, and stress management also help manage symptoms.
Can lifestyle changes help manage PCOS symptoms?
Yes, lifestyle changes are important in managing PCOS. A healthy diet, regular exercise, and stress management improve health and well-being.
How can women with PCOS manage their condition and reduce long-term health risks?
Women with PCOS can manage their condition by working with their doctor. They should make lifestyle changes and stay informed about their condition.
What is the significance of multiple bilateral ovarian follicles in PCOS?
Multiple bilateral ovarian follicles are a key sign of PCOS, seen on ultrasound. They are used with other criteria to diagnose PCOS.
How do hormonal imbalances affect follicular development in PCOS?
Hormonal imbalances, like high androgens and insulin resistance, affect follicular development in PCOS. They disrupt ovulation and follicle growth.
References
National Center for Biotechnology Information. PCOS: Polycystic Ovaries, Infertility, and Irregular Periods. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3872139/