Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that women with early-stage breast cancer in one breast have similar survival rates? They can either have lumpectomy followed by radiation or a double mastectomy. This shows how complex it is to figure out mastectomy life expectancy.
Knowing how long you might live after a single mastectomy is very important. At our place, we aim to give top-notch international healthcare. We offer personalized VIP service and full medical support. We know that breast cancer prognosis depends on many things. These include the cancer’s stage, the treatments chosen, and your overall health.
Key Takeaways
- Women with early-stage breast cancer have similar survival rates with lumpectomy and radiation therapy as with double mastectomy.
- Mastectomy survival statistics vary based on cancer stage, treatment, and overall health.
- Understanding breast cancer prognosis is essential for patients and their families.
- Personalized care and full medical support are key for the best results.
- Our institution is dedicated to delivering exceptional international healthcare with a focus on premium service quality and expertise.
Understanding Mastectomy and Its Purpose

For many breast cancer patients, mastectomy is a necessary and life-saving surgical procedure. Choosing to undergo a mastectomy is a significant decision, and understanding the procedure is crucial.
A mastectomy is a surgery where one or both breasts are removed. It’s often done to treat breast cancer. This surgery can help manage the disease and improve survival chances.
Definition of Mastectomy
A mastectomy is a surgery where breast tissue is removed. The amount removed depends on the type of mastectomy and the patient’s situation. Our team of experts is dedicated to providing premium care and support throughout the treatment process.
Types of Mastectomy
There are several types of mastectomy procedures, including:
- Simple or Total Mastectomy: Removal of the entire breast.
- Modified Radical Mastectomy: Removal of the breast and some of the lymph nodes under the arm.
- Double or Bilateral Mastectomy: Removal of both breasts.
- Skin-Sparing Mastectomy: Removal of the breast tissue while preserving the skin over the breast.
Each type is chosen based on the patient’s specific needs and the stage of their cancer.
Reasons for Undergoing Mastectomy
Patients may undergo mastectomy for several reasons, mainly as a treatment for breast cancer. Other reasons include:
- Diagnosis of breast cancer that is at an advanced stage or has spread.
- Presence of genetic mutations that increase the risk of breast cancer.
- Recurrence of cancer in the same breast after previous treatments.
We emphasize the importance of discussing these options with healthcare professionals to determine the best course of action for each individual.
Understanding mastectomy and its implications is vital for making informed decisions about breast cancer treatment. Our commitment is to provide complete support and care to our patients throughout their journey.
Factors Influencing Life Expectancy

Choosing to undergo a mastectomy is a significant decision, and understanding the procedure is crucial.
Stage of Cancer at Diagnosis
The cancer’s stage at diagnosis greatly affects life expectancy. Early cancer is usually easier to treat than late-stage cancer. Breast cancer statistics show early detection leads to better survival rates.
Recent data shows a big difference in post mastectomy survival rates for early versus late diagnosis. This highlights the need for catching cancer early and acting fast.
Overall Health and Age
A person’s health and age are big factors in life expectancy after a mastectomy. Older or those with health issues face unique challenges compared to younger, healthier people.
When looking at breast cancer mortality rates, these factors are key. Doctors must tailor treatments to fit each patient’s needs.
Type of Treatment Post-Surgery
The treatment after surgery also affects life expectancy. This can include chemotherapy, radiation, hormone, or targeted therapy. The choice depends on cancer stage and overall health.
The mastectomy success rate improves with the right treatment after surgery. Knowing about treatment options helps patients make informed choices about their care.
Life Expectancy Statistics for Mastectomy
Knowing the life expectancy after a mastectomy is key for health decisions. We’ll look at survival rates, compare single and bilateral mastectomies, and how early detection affects life expectancy.
General Survival Rates
Studies have shown that survival rates after mastectomy are high. Women who have lumpectomy and radiation have survival rates similar to those who have mastectomy. The 5-year survival rate for breast cancer patients is very high, thanks to early detection.
We present the following survival rate statistics:
| Stage at Diagnosis | 5-Year Survival Rate | 10-Year Survival Rate |
| Stage I | 99% | 95% |
| Stage II | 85% | 70% |
| Stage III | 60% | 40% |
Comparison of Single vs. Bilateral Mastectomy
Choosing between single and bilateral mastectomy depends on cancer stage and health. Bilateral mastectomy may lower the risk of cancer in the other breast. But, it doesn’t always improve survival for unilateral breast cancer patients.
Key findings include:
- Bilateral mastectomy reduces the risk of contralateral breast cancer.
- Survival rates for single mastectomy are comparable to bilateral mastectomy for early-stage breast cancer.
- The decision between single and bilateral mastectomy should be based on individual risk factors and preferences.
Impact of Early Detection
Early detection of breast cancer greatly improves treatment outcomes and survival rates. Early detection means more effective treatments and higher survival chances.
Benefits of Early Detection:
- Improved survival rates due to timely intervention.
- Less aggressive treatment options, potentially avoiding mastectomy.
- Better overall prognosis and quality of life.
In conclusion, understanding life expectancy after mastectomy is vital. By looking at survival rates, the differences between single and bilateral mastectomies, and the benefits of early detection, we can make better decisions about breast cancer treatment.
Emotional and Psychological Effects
Choosing to undergo a mastectomy is a significant decision, and understanding the procedure is crucial.
Coping Mechanisms
Dealing with a mastectomy’s aftermath needs a variety of strategies. Patients find comfort in different ways, such as:
- Meditation and Mindfulness: These practices help lower stress and improve mental health.
- Counseling: Getting help from professionals to face emotional challenges.
- Support Groups: Sharing experiences with others who have gone through the same.
These methods help patients manage the emotional and psychological effects of mastectomy.
Support Systems
Having a robust support network, which includes family, friends, and healthcare professionals, is essential for effective recovery after a mastectomy. This includes:
- Family and Friends: The love and support from loved ones is essential.
- Healthcare Professionals: Doctors, nurses, and other healthcare workers offer valuable guidance.
- Community Resources: Access to resources and services that aid in recovery.
A well-rounded support system greatly aids in a patient’s recovery.
Long-Term Mental Health Considerations
The emotional and psychological effects of mastectomy can last long after recovery. Important long-term considerations include:
- Monitoring for Anxiety and Depression: Recognizing signs and getting help when needed.
- Maintaining a Healthy Lifestyle: Staying active, eating well, and getting enough rest.
- Ongoing Support: Continuing to have access to counseling and support groups.
By focusing on these long-term aspects, patients can better handle the emotional and psychological challenges after mastectomy.
Role of Follow-Up Care
Effective follow-up care is key for patients after mastectomy. It affects survival rates and quality of life. At our institution, we know how important a good follow-up plan is. It helps achieve the best breast cancer outcomes and improves patient prognosis.
Regular Check-Ups
Regular check-ups are vital in post-mastectomy care. They let healthcare providers watch for signs of recurrence and fix any issues quickly. We suggest:
- Follow-up appointments every 3-6 months for the first few years post-surgery
- Annual mammograms on the remaining breast, as well as other imaging tests as needed
- Physical examinations to check for any abnormalities or signs of recurrence
Screening for Recurrence
Screening for recurrence is a key part of follow-up care. It helps catch problems early. We use a mix of:
- Mammography and other imaging modalities to monitor for any changes
- Clinical examinations to assess for signs of local recurrence
- Patient education on self-examination techniques to encourage active participation in monitoring
Managing Side Effects
Managing side effects is vital for a good quality of life after mastectomy. Our team works hard to help with issues like:
- Lymphedema management through physical therapy and compression garments
- Pain management strategies, including medication and alternative therapies
- Emotional support through counseling and support groups
By focusing on follow-up care, we can greatly improve mastectomy prognosis and patient outcomes. Our dedication to delivering top-notch international healthcare with personalized VIP service ensures our patients get all the support they need.
Nutritional Considerations Post-Mastectomy
Recovering from a mastectomy needs more than just medical care. A good diet is key to helping your body heal. Eating well can improve breast cancer treatment outcomes.
We suggest eating a variety of foods full of important nutrients. Foods like fruits, vegetables, whole grains, and lean proteins are great. They can really help with mastectomy recovery outcomes.
Importance of a Balanced Diet
Eating a balanced diet is vital for your health and recovery. It helps in:
- Rebuilding tissues
- Boosting the immune system
- Providing energy
A balanced diet should include:
- Protein-rich foods like lean meats, fish, and legumes
- Complex carbohydrates such as whole grains
- Healthy fats found in nuts, seeds, and avocados
Supplements and Their Benefits
While a balanced diet is key, some supplements can also help. But, always talk to your doctor before taking any supplements.
Some good supplements include:
- Omega-3 fatty acids for their anti-inflammatory properties
- Vitamin D for its role in bone health and immune function
- Probiotics for maintaining gut health
Foods that Promote Healing
Adding certain foods to your diet can help with healing. These include:
- Antioxidant-rich foods like berries and leafy greens
- Foods high in fiber such as whole grains and vegetables
- Lean proteins that support tissue repair
By eating a nutrient-rich diet and choosing the right supplements, patients can improve their breast surgery survival rate. This can also help with overall breast cancer recovery.
The Influence of Lifestyle Choices
Making smart lifestyle choices can improve life quality and survival rates for breast cancer patients after mastectomy. Diet, exercise, and managing stress are key to recovery and health.
Exercise and Physical Activity
Regular exercise is key to getting strong and healthy again after mastectomy. Physical activity can lower the risk of cancer coming back and improve survival chances. We suggest a blend of cardio and strength training to build muscle.
- Aerobic exercises like walking, cycling, or swimming for at least 150 minutes per week.
- Strength training exercises to be done 2-3 times a week, focusing on all major muscle groups.
- Flexibility and stretching exercises to improve range of motion and reduce stiffness.
A study found that exercise is good for breast cancer survivors. It improves physical function and quality of life.
“Physical activity is not only beneficial for physical health but also for mental well-being, reducing symptoms of anxiety and depression.”
Smoking and Alcohol Consumption
Smoking and drinking too much alcohol can harm health after mastectomy. Quitting smoking and drinking less can greatly improve outcomes. We suggest getting help to stop smoking and drinking in moderation.
- Resources for smoking cessation, including counseling and medication.
- Limiting alcohol intake to no more than one drink per day for women.
Stress Management Techniques
Managing stress well is important for overall health. Practices like meditation, yoga, and deep breathing can help. Adding these to daily routines can boost mental health and resilience.
- Mindfulness and meditation practices to reduce stress and anxiety.
- Yoga and tai chi for improving flexibility and balance.
- Deep breathing exercises for immediate stress relief.
By choosing these lifestyle options, people can actively improve their recovery and long-term health. We urge patients to create a personalized plan with their healthcare team.
The Importance of Family History
Family history is key in figuring out your risk for breast cancer. Knowing your genetic factors helps you understand your risk. This knowledge lets you take steps to prevent it.
Genetic Factors in Breast Cancer
Genetic mutations, like in the BRCA1 and BRCA2 genes, raise your breast cancer risk a lot. These can come from either parent. If your family has a history of breast cancer, it might mean you’re at higher risk too.
If you have a family history of breast cancer, think about getting genetic counseling. It helps you understand your family’s health history. You’ll learn about the risks and benefits of genetic tests and what they mean.
Talking to Family about Risks
Talking about breast cancer risk with your family is important. It helps catch problems early. We suggest making a family tree to keep track of health issues.
When you talk about risks, be ready with info on genetic tests and how to lower your risk. This includes talking about the good and bad of genetic tests. You can also discuss ways to watch your health closely.
Options for Genetic Testing
Genetic tests can find mutations in genes like BRCA1 and BRCA2. If you have a big family history, testing can tell you a lot about your risk. We offer genetic testing and counseling to help you understand your results.
The test is a blood test, and it takes a few weeks to get the results. We stress the need for counseling before the test. This way, you’ll know what the results mean and what you can do next.
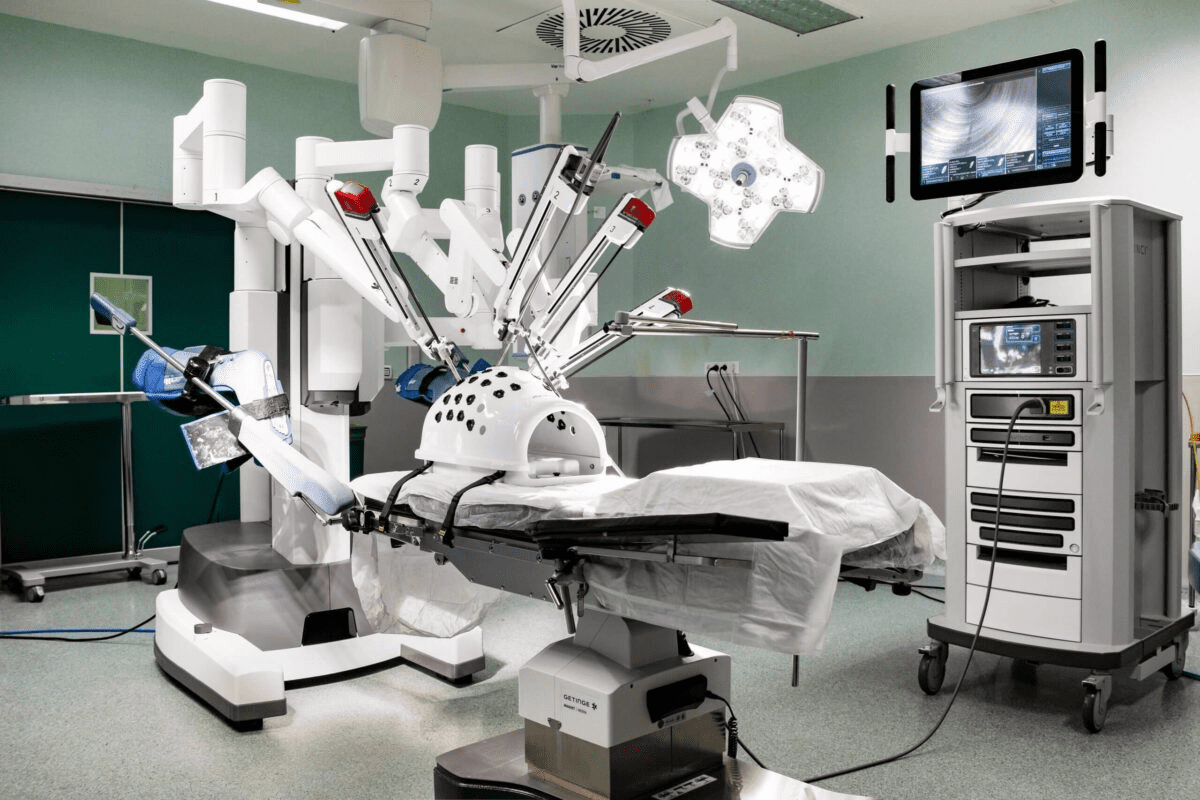
Advances in Mastectomy Techniques
New surgical methods have changed mastectomy for the better. They help patients recover faster and live longer. These improvements are big steps forward.
Minimally Invasive Procedures
Minimally invasive mastectomies are becoming more common. They cause less damage and help patients heal quicker. This is because they use smaller cuts, leading to less pain and scarring.
Now, doctors are using techniques like nipple-sparing mastectomy. This keeps the nipple and areola area intact. It makes the breast look more natural after reconstruction.
Innovations in Breast Reconstruction
Breast reconstruction is now a big part of mastectomy care. New methods in both implant and tissue reconstruction are being used. 3D printing and bioengineered scaffolds are making reconstructions more accurate and personal.
Microsurgery has also gotten better. This has made autologous flap reconstructions look and feel more natural. It’s a big win for patients.
Research and Future Treatments
Research is always looking to make mastectomy and reconstruction better. Scientists are studying how to use immunotherapy and targeted therapy with surgery. This could lead to even better results for breast cancer patients.
We expect even more progress in the future. New technologies and personalized treatments will likely improve survival rates. This is exciting for the future of mastectomy and reconstruction.
Personal Stories and Experiences
We know how important it is to share personal stories of those who have had a mastectomy. These stories offer valuable insights and support to those going through breast cancer recovery.
Real-Life Survivor Testimonials
Many women have shared their experiences after a mastectomy. They talk about how early detection and treatment helped them. Their stories show the strength and resilience of those facing mastectomy recovery.
Support Communities and Resources
Having a robust support network, which includes family, friends, and healthcare professionals, is essential for effective recovery after a mastectomy.
Inspiring Journeys to Recovery
The inspiring stories of breast cancer survivors show our ability to overcome challenges. By sharing these stories, we aim to create a supportive environment. This encourages healing and growth.
FAQ
What is the average life expectancy after a single mastectomy?
Life expectancy after a single mastectomy varies. It depends on cancer stage, health, and treatment type. Generally, the 5-year survival rate is about 90% for breast cancer patients who have had a mastectomy.
How does the stage of cancer at diagnosis affect life expectancy after mastectomy?
Cancer stage at diagnosis greatly affects life expectancy after mastectomy. Early-stage cancer patients usually have a better prognosis and higher survival rates. Those with advanced-stage cancer face lower survival rates.
What are the differences in survival rates between single and bilateral mastectomy?
Survival rates for single and bilateral mastectomy are often similar. But, bilateral mastectomy might slightly increase survival chances for those with high-risk genetic mutations or past cancer in one breast.
How important is follow-up care after mastectomy?
Follow-up care after mastectomy is very important. It helps monitor for recurrence, manage side effects, and keep overall health in check. Regular check-ups and screenings can catch issues early, improving survival rates.
What nutritional considerations should be taken into account after mastectomy?
Eating a balanced diet is key for recovery after mastectomy. Foods high in antioxidants and omega-3 fatty acids help healing. Healthcare professionals might also recommend vitamin D and calcium supplements.
How do lifestyle choices influence recovery and overall health after mastectomy?
Lifestyle choices like regular exercise, healthy diet, and stress management greatly impact recovery and health after mastectomy. Avoiding smoking and limiting alcohol can also reduce complications and improve outcomes.
What is the significance of family history in breast cancer?
Family history is very important in breast cancer risk. Those with a family history may benefit from genetic testing and counseling. This helps assess risk and plan for prevention and early detection.
What advances have been made in mastectomy techniques?
New mastectomy techniques include minimally invasive procedures and breast reconstruction innovations. These aim to improve outcomes, shorten recovery times, and enhance quality of life for patients.
Where can I find support and resources after mastectomy?
Many resources support individuals after mastectomy, like survivor communities, online forums, and local groups. These offer emotional support, guidance, and connection with others who’ve gone through similar experiences.
What are the benefits of genetic testing for breast cancer?
Genetic testing can identify high-risk genetic mutations like BRCA1 and BRCA2. This information helps in making prevention, early detection, and treatment decisions, improving outcomes.
How can I manage stress and anxiety after mastectomy?
Stress and anxiety after mastectomy can be managed with meditation, yoga, and counseling. These practices support emotional well-being and recovery.
JAMA Network. Evidence-Based Medical Insight. Retrieved from
https://jamanetwork.com/journals/jama/article-abstract/2668160