Last Updated on December 2, 2025 by Bilal Hasdemir
Getting diagnosed with breast cancer can change your life. Choosing the right surgery is a big decision. Nearly 1 in 8 women will be diagnosed with breast cancer in their lifetime. It’s key to know your treatment options.Mastectomy vs lumpectomy: the ultimate choice. Our guide breaks down the critical pros and cons to help you make the best decision.
Patients often debate between mastectomy and lumpectomy for breast cancer surgery. We’ll look at the differences. This will help you decide on your breast cancer treatment.
Key Takeaways
- Understanding the differences between mastectomy and lumpectomy is key for breast cancer patients.
- Both options have benefits and downsides.
- The right choice depends on cancer stage and personal preference.
- Some patients might choose breast-conserving surgery, like lumpectomy.
- Talking to a healthcare provider is vital to pick the best surgery.
Understanding Breast Cancer Surgery Options

Understanding breast cancer surgery can significantly aid patients in making informed choices about their treatment options. Surgery is key in treating breast cancer. The type of surgery chosen can greatly affect the outcome and the patient’s life quality.
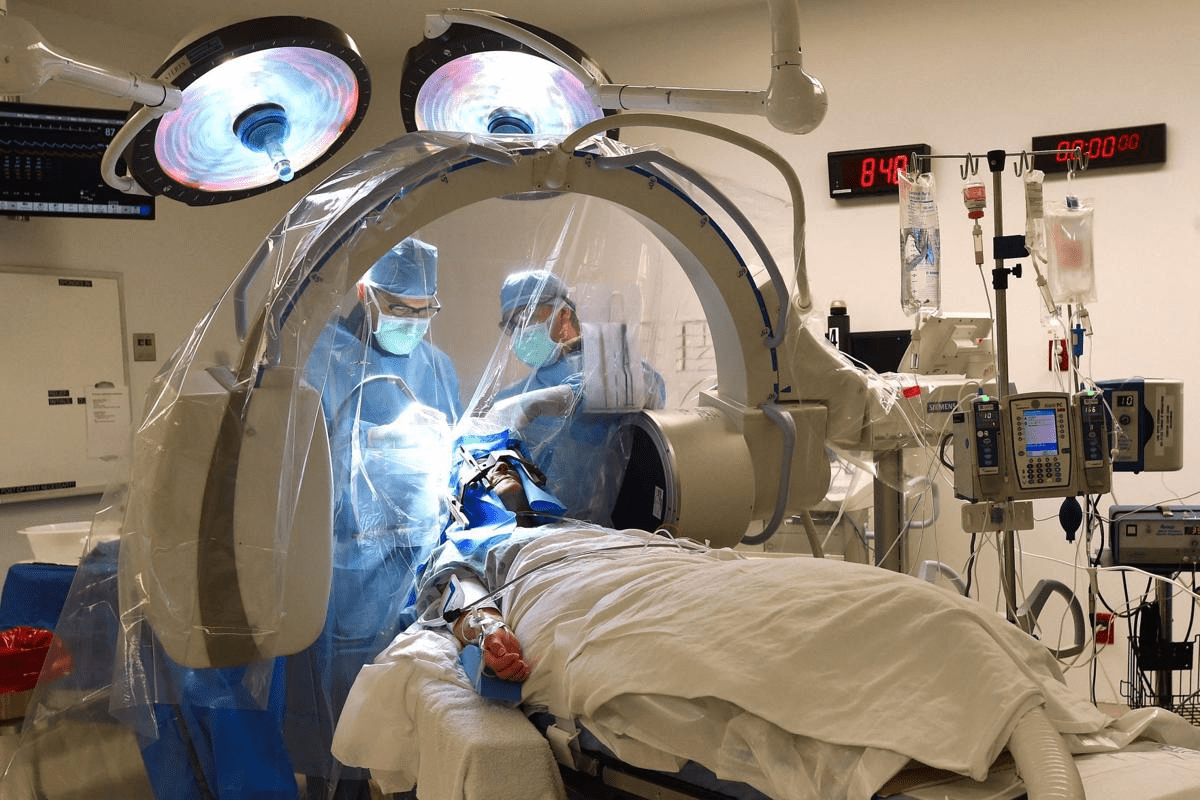
The Role of Surgery in Breast Cancer Treatment
Surgery is vital in treating breast cancer. It offers various options based on the patient’s condition. The main goal is to remove the cancerous tissue.
Breast cancer surgery is often the first treatment. The choice of procedure depends on several factors. These include the cancer’s stage and type.
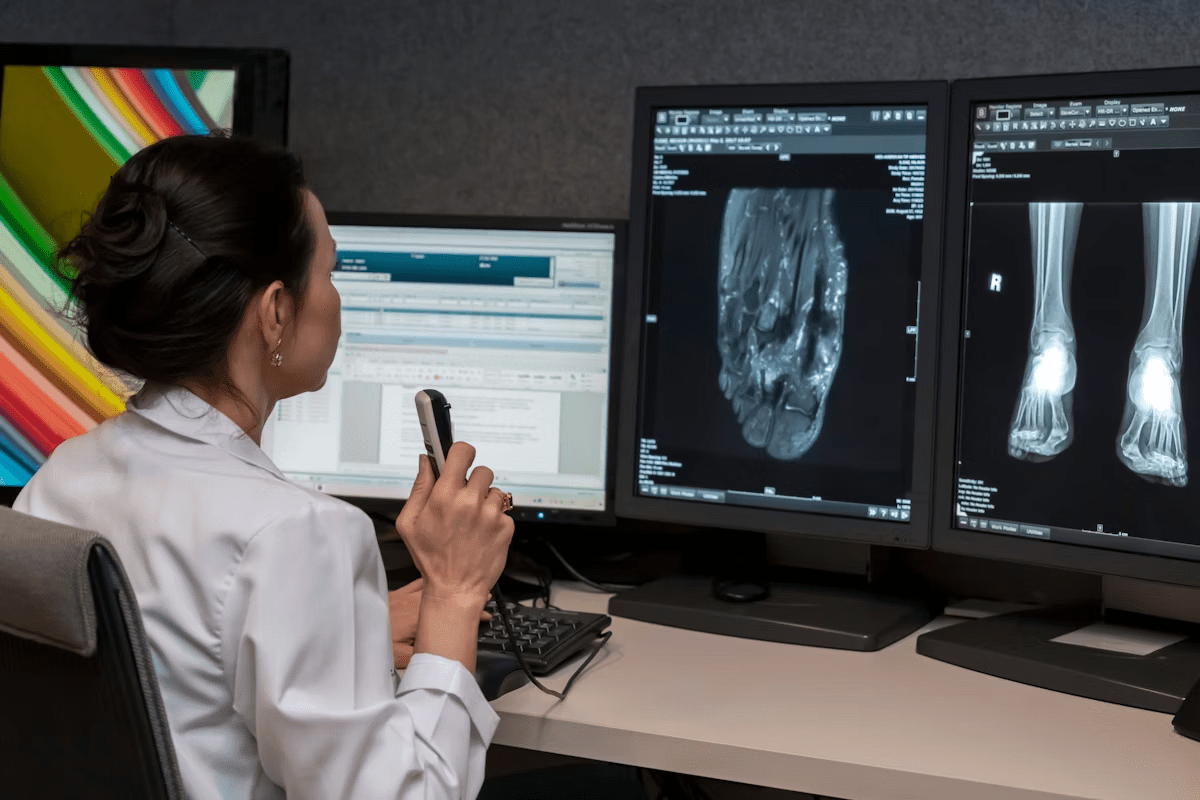
Factors That Influence Surgical Decisions
Many factors affect the choice of surgical procedures. These include the cancer’s stage and type, patient preferences, and overall health. The decision between a lumpectomy and a mastectomy is complex.
It involves considering the patient’s specific circumstances. It also looks at the risk of cancer coming back and survival rates. Understanding these factors is key for making informed decisions.
When deciding between lumpectomy vs mastectomy, patients and doctors must weigh the pros and cons. They consider the risk of cancer coming back, the need for more treatments like radiation, and the impact on physical and emotional well-being.
What Is a Lumpectomy?
Lumpectomy is a surgery that removes a cancerous lump and some healthy tissue around it. It’s a conservative way to treat breast cancer. This method tries to keep as much of the breast as possible.
Breast-Conserving Surgery Explained
Lumpectomy is a surgery for women with early-stage breast cancer. It aims to remove the tumor and some healthy tissue. This way, it’s less invasive than mastectomy and keeps more of the breast.
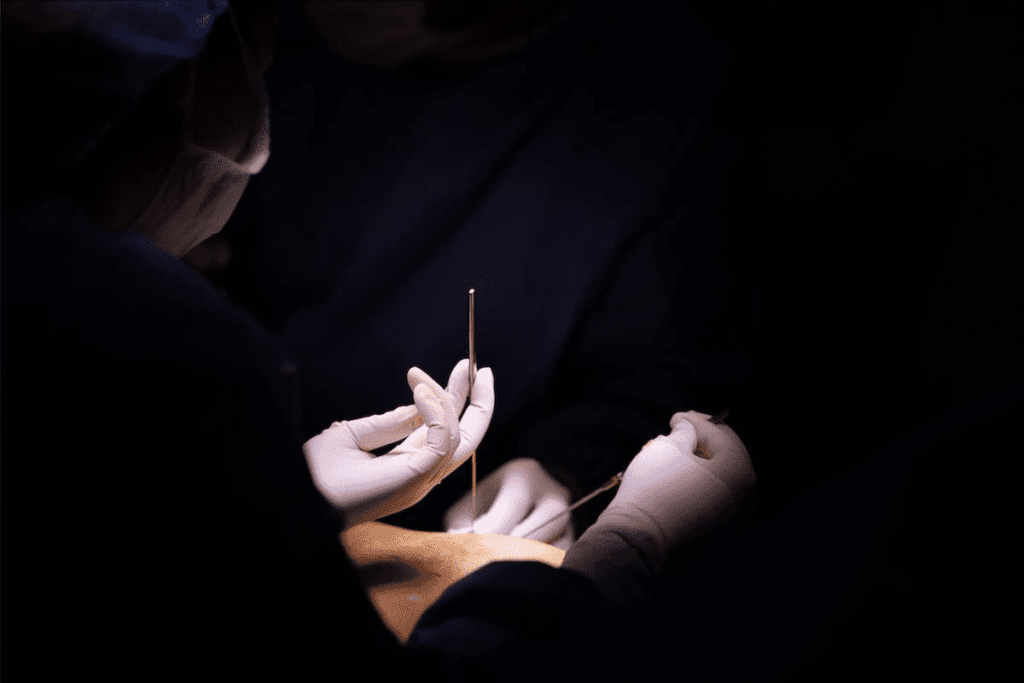
The surgery involves making an incision to reach the tumor. The surgeon then takes out the tumor and some healthy tissue around it. This tissue is checked to make sure no cancer cells are left.
Procedure Details and Technique
The way a lumpectomy is done can change based on the tumor’s size and location. It also depends on the patient’s breast size and shape. We use different techniques to reduce scarring and improve the breast’s look.
After removing the tumor, the area is closed with sutures. The incision is also closed with sutures or staples. The surgery is done under general anesthesia, and its length varies.
Ideal Candidates for Lumpectomy
Not everyone with breast cancer can have a lumpectomy. The choice depends on the cancer’s size and stage, the breast’s size, and the patient’s health. Lumpectomy is usually for those with small tumors and early-stage cancer.
It’s also important if the patient wants to keep their breast. They must be ready for radiation therapy after surgery. Radiation helps lower the chance of cancer coming back.
What Is a Mastectomy?
Mastectomy is a surgery to remove breast tissue. It’s a common treatment for breast cancer. There are different types to meet various needs. Choosing to have a mastectomy is a big decision. It’s important to know what it involves.
Types of Mastectomy Procedures
There are several mastectomy procedures. Each has its own purpose and benefits. Here are the main types:
- Simple or Total Mastectomy: This removes the whole breast, including the nipple and areola, and most skin.
- Modified Radical Mastectomy: This removes the breast and some lymph nodes under the arm.
- Skin-Sparing Mastectomy: It removes the breast tissue but keeps as much skin as possible. This makes breast reconstruction easier.
- Nipple-Sparing Mastectomy: The breast tissue is removed, but the nipple and areola are kept. This is often for early-stage cancer.
Each type of mastectomy has its own benefits. The choice depends on the cancer type, size, and the patient’s wishes for reconstruction.
When Mastectomy Is Recommended
A mastectomy is recommended in certain situations. These include:
- Large Tumors: If the tumor is big compared to the breast, mastectomy might be the best choice.
- Multicentric Cancer: If there are many areas of cancer in the breast, mastectomy is often suggested.
- Genetic Predisposition: Women with a strong family history or certain genetic markers might choose preventive mastectomy.
- Recurrence: If cancer comes back after other treatments, mastectomy might be considered.
Knowing the mastectomy benefits and the types of mastectomy is key to making a good decision. We’re here to support you, ensuring you get the care that’s right for you.
After a mastectomy, recovery starts. You can also explore reconstruction after mastectomy. We’ll help you through these steps, providing all the care and support you need.
Mastectomy vs Lumpectomy: Key Differences
Mastectomy and lumpectomy are two main ways to treat breast cancer. Each has its own features. Knowing these differences helps patients choose the right treatment.
Surgical Approach Comparison
The main difference is in how the surgery is done. A lumpectomy takes out the tumor and a bit of tissue around it. This way, the breast might look the same. On the other hand, a mastectomy removes one or both breasts, either partly or completely.
“The choice of surgery can significantly impact a patient’s quality of life and should be made after careful consideration of all available options.”
Impact on Breast Tissue
Lumpectomy keeps most of the breast tissue, keeping its look. Mastectomy takes out more or all of it, which can change how the breast looks. It might need to be rebuilt.
Surgical Procedure | Breast Tissue Removed | Potential for Reconstruction |
Lumpectomy | Minimal | Less likely |
Mastectomy | Significant to all | Yes |
Hospital Stay Requirements
Lumpectomy is usually done as an outpatient, so patients go home the same day. Mastectomy is more serious and might need a longer stay, from one to several days.
Knowing these differences helps patients and doctors make better choices for breast cancer treatment. Every person’s case is different. What’s right for one might not be for another.
Survival Rates: Lumpectomy vs Mastectomy
When looking at breast cancer treatment, knowing the survival rates for lumpectomy and mastectomy is key. We dive into the long-term survival stats and what affects them. This helps us see how these surgeries impact survival.
Long-term Survival Statistics
Many studies have looked at survival rates for lumpectomy and mastectomy. They found that for early-stage breast cancer, survival rates are often the same for both.
Long-term Survival Rates: Studies show that the 10-year survival rates for both lumpectomy and mastectomy are about the same. Some research suggests that lumpectomy with radiation might lead to slightly better survival rates for some patients.
Surgical Procedure | 5-Year Survival Rate | 10-Year Survival Rate |
Lumpectomy with Radiation | 90-95% | 80-85% |
Mastectomy | 85-90% | 75-80% |
Factors Affecting Survival Outcomes
The surgery is important, but it’s not the only thing that matters. Other factors also play a big role:
- Cancer Stage: The stage at which breast cancer is found greatly affects survival.
- Tumor Characteristics: The size, grade, and receptor status of the tumor also matter.
- Patient Health: A person’s overall health, including other health issues, impacts survival.
- Adjuvant Therapies: Treatments like radiation, chemotherapy, and hormone therapy can improve survival rates.
It’s important to understand these factors and how they relate to the choice of surgery. This helps patients make informed decisions about their treatment.
Recurrence Risk Comparison
Knowing the risk of cancer coming back is key for patients choosing between lumpectomy and mastectomy. The chance of local recurrence differs between these surgeries. This affects patient choices and treatment results.
Local Recurrence After Lumpectomy
Lumpectomy removes the tumor and some tissue around it. It’s effective but comes with a risk of local recurrence. Radiation therapy can lower this risk.
Radiation therapy is vital after lumpectomy, mainly for early-stage breast cancer. It kills any cancer cells left in the breast, cutting down recurrence chances.
Local Recurrence After Mastectomy
Mastectomy removes one or both breasts, partially or fully. The risk of local recurrence after mastectomy is usually lower than after lumpectomy. This is when combined with treatments like radiation and chemotherapy. The choice to have mastectomy depends on the disease’s extent and personal factors.
In some cases, reconstruction surgery is done after mastectomy. It offers psychological benefits but doesn’t change recurrence risk.
Surgical Approach | Local Recurrence Risk | Role of Radiation Therapy |
Lumpectomy | Higher without radiation | Significantly reduces recurrence risk |
Mastectomy | Generally lower | May be recommended for high-risk patients |
It’s important to compare recurrence risks between lumpectomy and mastectomy. Both surgeries have their roles in treatment. But knowing how each affects local recurrence is critical for patient care.
Recovery Time and Process
When choosing between lumpectomy and mastectomy, recovery time is a big factor. Knowing what to expect can help patients deal with surgery better and get back to their lives sooner.
Lumpectomy Recovery Timeline
Lumpectomy recovery is usually shorter than mastectomy. Most people can get back to normal in a few weeks. The recovery process after a lumpectomy is often easier, with less scarring and a quicker return to life before surgery.
It’s important for patients to follow a care plan after surgery. This includes gentle exercises to keep flexibility and prevent problems. The recovery timeline can vary, depending on health and surgery extent.
Mastectomy Recovery Timeline
Mastectomy recovery takes longer and is more complex. The mastectomy recovery process can last weeks to months. This depends on if it was done alone or with other treatments like reconstruction.
Patients should prepare for a longer recovery with mastectomy. This includes drainage tubes, follow-up visits, and a slow return to activities. A detailed care plan is key to avoid complications and support healing.
Both lumpectomy and mastectomy have their own recovery paths. Understanding these differences helps patients make better choices about their surgery.
Radiation Therapy Requirements
Radiation therapy is key in treating breast cancer. It depends on the surgery type. We’ll look at when it’s needed after lumpectomy and mastectomy. This helps patients understand their treatment choices.
Radiation After Lumpectomy
After a lumpectomy, radiation is often advised. It kills any cancer cells left in the breast. This lowers the chance of cancer coming back. Lumpectomy radiation uses external beam radiation therapy (EBRT) at the tumor site. It’s given over weeks.
The aim is to get rid of any tiny cancer cells. This means less chance for more surgery.
When Radiation Is Needed After Mastectomy
Even with mastectomy, radiation therapy after mastectomy might be needed. This is true if cancer has spread to lymph nodes or if the tumor is big. The choice for mastectomy radiation depends on the patient’s risk for recurrence.
It’s a decision made with the healthcare provider. Knowing about radiation therapy in breast cancer treatment is important. It helps patients make informed choices about their surgery and care after.
Cosmetic Outcomes and Reconstruction
It’s important for patients to know about the looks of lumpectomy and mastectomy before surgery. The looks after surgery can really affect how a person feels about themselves.
Aesthetic Results of Lumpectomy
A lumpectomy tries to keep most of the breast while removing the tumor. The looks after a lumpectomy can change based on the tumor’s size and where it is. It also depends on the size and shape of the breast.
Most people who have a lumpectomy keep a lot of their natural breast look. But, there might be some scarring or changes in how the breast feels. Sometimes, more surgery is needed to make the breast look better.
Aesthetic Results of Mastectomy
A mastectomy means removing one or both breasts, either partly or completely. The looks after a mastectomy can be more different than after a lumpectomy because more of the breast is removed.
People who have a mastectomy might feel different about their body. But, new surgery methods and ways to rebuild the breast have made things better for many.
Reconstruction Options After Mastectomy
Choosing to rebuild the breast after a mastectomy is a personal choice. It can help people feel more like themselves again. There are a few ways to do this, like using implants or the patient’s own tissue.
Reconstruction Method | Description | Advantages |
Implant-Based Reconstruction | Uses silicone or saline implants to recreate the breast | Less invasive, shorter recovery time |
Autologous Tissue Reconstruction | Uses the patient’s own tissue from another part of the body | More natural feel and appearance, long-term results |
Each way to rebuild the breast has its own good points and things to think about. Patients should talk to their doctors to find the best choice for them.
Emotional and Psychological Impact
Breast cancer surgery, like mastectomy or lumpectomy, affects patients deeply. It goes beyond just the physical. The emotional and psychological effects can change a patient’s life in many ways.
Body Image and Self-Esteem Considerations
When a breast is changed or removed, it can really affect a woman’s body image and self-esteem. Patients often feel a deep loss. This loss is not just about the breast but also about feeling feminine or attractive.
Healthcare providers need to be understanding and caring. They should talk about these feelings with sensitivity.
Research shows that body image can be different for mastectomy and lumpectomy patients. Some might feel less changed after a lumpectomy. But, everyone reacts differently. Health, support, and personal strength are key factors.
Coping Strategies and Support Resources
Dealing with the emotional and psychological effects of surgery needs a variety of approaches. Coping strategies include counseling, support groups, and mindfulness. These help patients deal with their feelings and adjust to their new life.
- Support groups, online or in-person, offer a place to share and find support.
- Professional counseling helps with specific emotional challenges like anxiety or depression.
- Mindfulness and relaxation can help reduce stress and improve well-being.
By understanding the emotional and psychological effects of surgery, healthcare providers can offer better care. This care goes beyond just the physical. It supports the patient’s emotional and psychological healing too.
How to Make Your Decision
Choosing between a mastectomy and a lumpectomy is a big decision. It involves looking at both medical and personal factors. We need to think about what’s best for us, based on our health and personal choices.
Medical Factors to Consider
Medical aspects are key when deciding between mastectomy and lumpectomy. We need to think about the cancer’s stage, tumor size, and genetic risks. Knowing these details helps choose the right surgery.
For example, if the cancer is small and caught early, a lumpectomy might be a good choice. This could be followed by radiation to lower the chance of cancer coming back. But if the cancer is bigger or there are more tumors, a mastectomy might be better.
Personal Preferences and Lifestyle Impact
Our personal feelings and lifestyle also matter a lot. Think about how each surgery might change how we see ourselves and our life.
Some might want to keep more of their natural breast tissue, making lumpectomy appealing. Others might choose mastectomy to lower cancer risk. We should also think about recovery time, the need for reconstruction, and how it affects our daily life.
“The decision between mastectomy and lumpectomy is not just about removing the cancer; it’s about choosing a path that aligns with our personal values, lifestyle, and long-term well-being.”
Questions to Ask Your Healthcare Team
Talking to our healthcare team is key to making a good choice. Here are some important questions to ask:
- What are the specific advantages and disadvantages of mastectomy and lumpectomy in my case?
- How will the chosen surgical approach impact my risk of recurrence?
- What are the possible side effects and complications of each option?
- How will surgery and treatments affect my daily life and activities?
- Are there any extra treatments, like radiation or chemotherapy, needed?
By asking these questions and talking with our healthcare team, we can make a choice that fits our unique situation and goals.
Conclusion
Looking at mastectomy vs lumpectomy, we see both are key in fighting breast cancer. The choice depends on the cancer’s stage, type, and the patient’s health and wishes.
A summary of mastectomy vs lumpectomy shows their different ways to treat cancer. A lumpectomy saves more of the breast, while a mastectomy removes one or both. Knowing these differences helps patients make better choices.
We’ve talked about what to consider when choosing between mastectomy and lumpectomy. Patients can decide based on what’s best for them medically and personally. A detailed look at breast cancer treatment shows the need for a plan that fits each patient’s needs for the best results.
FAQ
What is the main difference between a mastectomy and a lumpectomy?
A mastectomy removes the whole breast. A lumpectomy takes out just the tumor and a bit of tissue around it. This aims to keep the breast looking normal.
Which surgical option is more effective in treating breast cancer?
Both mastectomy and lumpectomy can treat breast cancer well. They have similar survival rates for early-stage cancer. The choice depends on the cancer’s stage, size, and your preference.
Do I need radiation therapy after a lumpectomy?
Yes, usually, you’ll need radiation after a lumpectomy. It helps kill any cancer cells left in the breast. This lowers the chance of cancer coming back.
How long is the recovery time for a lumpectomy compared to a mastectomy?
Recovery from a lumpectomy is quicker, taking a few days to weeks. Mastectomy recovery can take weeks to months.
Can I choose to have a mastectomy even if a lumpectomy is an option?
Yes, you can choose mastectomy over lumpectomy for personal reasons. It depends on your cancer, breast size, and what you prefer.
Are there any differences in the risk of local recurrence between mastectomy and lumpectomy?
With radiation, the risk of cancer coming back is similar for both. This is true for early-stage breast cancer.
How does the cost of mastectomy compare to lumpectomy?
Costs vary by location, insurance, and treatments needed. Mastectomy might be pricier, mainly if you choose reconstruction.
What are the cosmetic outcomes of lumpectomy versus mastectomy?
Lumpectomy usually looks better because it keeps more of the breast. Mastectomy can change the breast’s look, more so without reconstruction.
Can I have breast reconstruction after a mastectomy?
Yes, you can get breast reconstruction after mastectomy. It can be done right after or later, using different methods and materials.
How do I decide between mastectomy and lumpectomy?
Talk to your healthcare team to decide. Consider your cancer, breast size, personal wishes, and lifestyle. Knowing the pros and cons of each helps choose what’s best for you.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8555933/