Mastocytosis is one of the rare blood diseases that can be very dangerous if not treated right away. Mastocytosis affects the blood and can lead to serious complications.
We are here to help you understand the risks of rare blood diseases. Mastocytosis is a condition where abnormal mast cells accumulate in various parts of the body. This can cause a range of symptoms, from mild to severe.
It’s important to know about these conditions for effective management and treatment. In this article, we will explore rare blood diseases, their symptoms, diagnosis, and treatment options.
Key Takeaways
- Rare blood diseases can be life-threatening if not properly diagnosed and treated.
- Mastocytosis is a disorder that affects the blood and can lead to serious complications.
- Understanding the symptoms and risks of rare blood diseases is key for timely medical intervention.
- Effective management and treatment of rare blood diseases require a thorough approach.
- Timely diagnosis can greatly improve outcomes for patients with rare blood diseases.
Understanding Rare Blood Diseases
It’s key to understand rare blood diseases to help patients and grow medical knowledge. These diseases, though rare, affect many people around the world.
Definition and Classification
Rare blood diseases include many disorders affecting blood cells or proteins. Mastocytosis is one, causing symptoms from mild to severe due to mast cell buildup.
Classifying these diseases is complex. We sort them by the blood cell type, genetic cause, or symptoms. This helps in planning treatment and understanding the disease’s progression.
Prevalence and Impact
The number of people with rare blood diseases varies. Some are very rare, affecting only a few worldwide. Yet, these diseases have a big impact on patients and their families.
They often lead to chronic illness, disability, and sometimes a shorter life. Knowing about these diseases helps raise awareness and fund research for better treatments. It’s a global healthcare issue.
Mastocytosis: An Overview
Mastocytosis is a complex condition where mast cells build up in body tissues. This buildup can cause many symptoms and affect different organs. It’s hard to diagnose and manage.
Defining Mastocytosis
Mastocytosis is a group of disorders with too many mast cells. Mast cells are important for the immune system, helping with allergies and inflammation. In mastocytosis, these cells gather in tissues like the skin, bone marrow, and gut.
This buildup can release chemicals that cause symptoms like flushing, itching, and stomach pain. How bad these symptoms are can vary a lot from person to person.
Types of Mastocytosis
Mastocytosis can be divided into several types based on where mast cells gather. The main types are:
- Cutaneous Mastocytosis: Mainly affects the skin, showing up as lesions or rashes.
- Systemic Mastocytosis: Mast cells spread to organs like the bone marrow, liver, and spleen.
- Localized Mast Cell Tumors: Rare cases where mast cells form a tumor in one place.
Knowing the type of mastocytosis is key to finding the right treatment and managing it well.
Living with mastocytosis can be tough, both physically and emotionally. We aim to offer full care and support to those affected. Our goal is to help them deal with mastocytosis and improve their life quality.
Mastocytosis in Adults vs. Children
Mastocytosis is a condition where mast cells build up abnormally. It affects adults and children differently, leading to unique challenges in diagnosis and treatment. Let’s dive into these differences to understand how mastocytosis impacts people of various ages.
Pediatric Mastocytosis Presentation
In kids, mastocytosis often shows up as urticaria pigmentosa on the skin. This usually happens in the early years of life. The skin lesions can itch and turn red when touched, a sign known as Darier’s sign.
For many children, mastocytosis only affects the skin. It often goes away on its own by the time they reach their teens. But some kids might have other symptoms like stomach problems, flushing, and severe allergic reactions.
Adult-Onset Mastocytosis
Adults with mastocytosis face a more complex situation. Their mast cells build up in the skin and organs like the bone marrow, liver, and spleen. Symptoms can range from mild skin issues to serious problems like bone loss, stomach troubles, and a higher risk of severe allergic reactions.
Diagnosing mastocytosis in adults requires a detailed check-up, including a bone marrow biopsy and genetic tests for KIT D816V mutations. Knowing the specific traits of adult mastocytosis helps doctors create a treatment plan that fits each person’s needs.
By understanding the differences between mastocytosis in kids and adults, we can better diagnose and treat this condition. This approach can lead to better health outcomes for everyone affected.
Systemic Mastocytosis and Its Life-Threatening Potential
It’s key to know about systemic mastocytosis to see its dangers. This disease makes mast cells build up in organs. This can cause many health problems.
Indolent Systemic Mastocytosis
Indolent systemic mastocytosis is a milder form. People with this type usually get symptoms slower. Symptoms can be managed well in many cases, making life better. But, it’s important to watch it closely because it can get worse.
Aggressive Systemic Mastocytosis
Aggressive systemic mastocytosis is more serious. It causes big problems because mast cells invade organs. This type needs quick and strong treatment to avoid big risks and help live longer.
Mast Cell Leukemia
Mast cell leukemia is a rare and fast-growing type. It shows up in the blood with mast cells. It has a bad outlook and needs quick doctor help. Doctors use many treatments to fight mast cells and ease symptoms.
We know systemic mastocytosis is a range of diseases, each with its own challenges. Understanding these differences helps doctors give better care. This can lead to better results for patients.
Symptoms and Signs of Mastocytosis
Mastocytosis can show mild skin symptoms or severe reactions, including anaphylaxis. It’s important to know these signs for quick diagnosis and treatment.
Cutaneous Symptoms
Cutaneous symptoms are common in mastocytosis. These include:
- Urticaria Pigmentosa: Brownish skin lesions that can appear anywhere.
- Darier’s Sign: Skin lesions become itchy, red, and swollen when rubbed.
- Pruritus: Many patients experience persistent itching.
Systemic Symptoms
Systemic symptoms happen when mastocytosis affects organs beyond the skin. These symptoms include:
- Gastrointestinal Issues: Abdominal cramps, diarrhea, and nausea are common.
- Musculoskeletal Pain: Bone pain and osteoporosis are concerns.
- Cardiovascular Symptoms: Flushing, hypotension, and tachycardia can occur.
Anaphylaxis Risk
Anaphylaxis is a severe complication of mastocytosis. It’s a life-threatening allergic reaction. Patients with mastocytosis are at higher risk. Triggers include:
- Insect Stings: Certain stings can cause severe reactions.
- Medications: Some drugs can trigger anaphylaxis.
- Foods and Other Allergens: Common allergens can also cause anaphylactic reactions.
It’s vital for healthcare providers to understand mastocytosis symptoms. Early diagnosis and treatment can greatly improve patient outcomes.
| Symptom Category | Common Symptoms |
| Cutaneous | Urticaria pigmentosa, pruritus, Darier’s sign |
| Systemic | Gastrointestinal issues, musculoskeletal pain, cardiovascular symptoms |
| Anaphylaxis Risk | Insect stings, medications, foods, and other allergens |
Diagnosing Mastocytosis
Diagnosing mastocytosis involves both clinical checks and special tests. Getting the diagnosis right is key to a good treatment plan.
Diagnostic Criteria
Healthcare providers use certain criteria to diagnose mastocytosis. They look for specific skin lesions and symptoms. They also check for mast cells in places like the bone marrow or gut.
The World Health Organization (WHO) has clear guidelines for diagnosing systemic mastocytosis. They have major and minor criteria. The major criterion is finding lots of mast cells in the bone marrow or other organs.
Testing Methods
There are several ways to diagnose mastocytosis, including:
- Bone Marrow Biopsy: This is the top test for systemic mastocytosis. It checks the bone marrow for mast cells.
- Blood Tests: Blood tests, like checking serum tryptase levels, can show if you have mastocytosis.
- Imaging Studies: CT scans or MRI help see how far the disease has spread and which organs are affected.
- Genetic Testing: Looking for the KIT gene mutation, like D816V, helps confirm systemic mastocytosis.
Finding a Mastocytosis Specialist
Finding a specialist in mastocytosis is very important. Look for doctors at big medical centers or those known for mast cell disorders.
A specialist can give a detailed check-up, accurate diagnosis, and a treatment plan just for you. They can also help manage symptoms and improve your life quality.
Treatment Options for Mastocytosis
The treatment for mastocytosis is varied, aiming to manage symptoms and slow disease growth. It’s important to know the different treatments to manage the condition well.
Symptom Management
Managing symptoms is key in treating mastocytosis. Antihistamines help with itching and flushing.
- H1 antihistamines for itching and flushing
- H2 antihistamines for stomach issues
- Corticosteroids for serious skin or stomach problems
Cromolyn sodium also helps with stomach symptoms, making life better for patients.
Disease-Modifying Therapies
These therapies aim to lower mast cell numbers and slow disease. Tyrosine kinase inhibitors (TKIs) are a big help, with imatinib being used sometimes.
- Imatinib for certain genetic cases
- Cladribine for aggressive mastocytosis
- New TKIs and agents are being researched
Emerging Treatments
New treatments for mastocytosis are on the horizon. These include targeted therapies and immunotherapies to better help patients.
- Trials on new TKIs with better safety and results
- Studies on CD117 therapies
- Looking into combo therapies for better results
As research grows, more treatment options for mastocytosis will come. This brings hope for patients and doctors.
Polycythemia Vera (PCV): When Blood Thickens
When blood thickens because of too many red blood cells, it might mean you have Polycythemia Vera. This condition can be serious. We’ll look into what PCV is, how it affects the body, and the dangers it poses.
Understanding High Hematocrit and PCV
Polycythemia Vera means your blood has too many red blood cells. This makes your blood thicker. It’s harder for your heart to pump blood around your body.
The reasons for PCV often start with genetic changes, like in the JAK2 gene. Knowing this helps doctors figure out what to do next.
Complications and Mortality Risk
PCV can lead to serious problems. These include:
- Thrombosis: Blood clots that can cause strokes or heart attacks.
- Hemorrhage: Bleeding issues because of the abnormal blood cells.
- Myelofibrosis: Bone marrow scarring, which can cause anemia and more.
It’s important to manage PCV well to avoid these issues. Regular check-ups and personalized treatment plans are key to keeping patients safe.
Essential Thrombocythemia: When Platelets Proliferate
Essential Thrombocythemia (ET) is a rare blood disorder. It causes the bone marrow to make too many platelets. This is part of a group of diseases called myeloproliferative neoplasms (MPNs). We will look into ET, covering its causes, symptoms, and treatments.
Pathophysiology and Symptoms
ET happens when genes like JAK2, CALR, or MPL mutate. This leads to too many platelets in the blood. The blood gets thicker, raising the risk of blood clots. Symptoms can vary but often include:
- Headaches
- Dizziness or lightheadedness
- Numbness or tingling in the hands and feet
- Weakness or fatigue
- Bleeding or bruising easily
Some people also get erythromelalgia. This is pain, redness, and warmth in the hands and feet.
Treatment Approaches
Treating ET aims to prevent blood clots and manage symptoms. We look at several things to choose the right treatment. These include the patient’s age, medical history, and heart risks. Common treatments are:
- Low-dose aspirin to prevent blood clots
- Cytoreductive therapy to lower platelet counts, using drugs like hydroxyurea or interferon-alpha
- Plateletpheresis in emergencies to quickly lower platelet counts
We also stress the need for regular check-ups. This helps adjust treatments and handle any new problems quickly.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Mastocytosis is a disorder that affects the blood and can lead to serious complications.
Mechanism of Disease
The main cause of PNH is a gene mutation in the PIGA gene. This gene is key for a protein that protects red blood cells from the immune system. Without this protein, red blood cells are destroyed by the immune system.
PNH’s cause is complex, involving genetics and the immune system. Knowing this helps us find better treatments.
Clinical Manifestations
PNH shows different symptoms, including:
- Hemolytic anemia, causing fatigue, shortness of breath, and jaundice.
- Bone marrow failure, leading to low blood counts and increased risk of infections and bleeding.
- Thrombosis, or blood clots, which can be dangerous.
These symptoms can differ a lot between patients. A detailed diagnosis is key to identifying PNH.
Modern Treatment Options
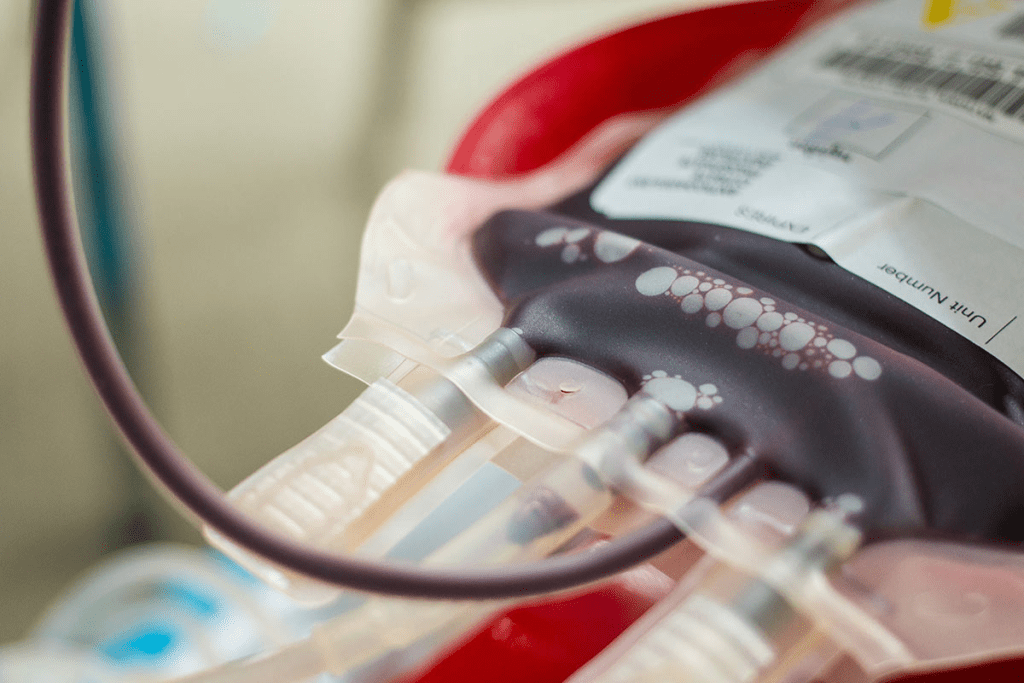
Treatments for PNH have improved a lot. Complement inhibitors like eculizumab are now used. These drugs block the complement system, reducing hemolysis and improving patient health.
| Treatment | Mechanism | Benefits |
| Eculizumab | Complement inhibitor | Reduces hemolysis, improves quality of life |
| Ravulizumab | Long-acting complement inhibitor | Less frequent dosing, improved patient compliance |
We are dedicated to leading in PNH treatment. We offer the newest therapies and care to manage this complex condition well.
Langerhans Cell Histiocytosis (LCH)
LCH, or Langerhans Cell Histiocytosis, is a unique challenge in blood disorders. It involves abnormal growth of Langerhans cells, a type of immune cell. This condition can show up in different ways, from single bone lesions to affecting many organs, making it hard to diagnose and treat.
The Complexity of LCH as a Blood Disorder
LCH affects the blood system. It causes Langerhans cells to build up in organs like bones, skin, and lymph nodes. The exact cause of LCH is not known, but it’s thought to be a mix of genetics and environment.
Understanding LCH shows that early diagnosis is key for good management. Symptoms can vary, from bone pain and swelling to fever and weight loss.
Current Treatment Approaches and Prognosis
Treatment for LCH depends on the patient’s situation. Chemotherapy is often used, sometimes with surgery or radiation for specific cases. For mild symptoms, a wait-and-see approach might be taken.
“The management of LCH requires a multidisciplinary approach, involving hematologists, oncologists, and other specialists to address the complex needs of these patients.” – Expert in Hematology
The outlook for LCH patients varies. Some may see their symptoms go away on their own, while others face a tougher road with possible long-term issues. Better treatments have helped, but more research is needed to fully understand and treat LCH.
Erdheim-Chester Disease: A Rare Form of Histiocytosis
Mastocytosis is a disorder that affects the blood and can lead to serious complications.
Clinical Features
This disease can cause a variety of symptoms. These include:
- Bone pain and skeletal abnormalities
- Neurological symptoms due to central nervous system involvement
- Cardiovascular issues, including periaortic fibrosis
- Pulmonary symptoms, such as cough and dyspnea
ECD can lead to serious health problems. It’s important to manage it well to avoid severe complications.
Diagnostic Challenges and Treatment
Diagnosing Erdheim-Chester Disease is hard because it’s rare and symptoms can be similar to other diseases. Doctors use imaging, biopsies, and lab tests to make a diagnosis.
Treatment for ECD varies based on how severe it is. It might include:
| Treatment Approach | Description |
| Targeted Therapy | Use of drugs targeting specific molecular pathways involved in ECD |
| Chemotherapy | Application of chemotherapeutic agents to reduce histiocyte proliferation |
| Interferon Therapy | Use of interferons to modulate the immune response |
Thanks to medical research, we now understand and can treat Erdheim-Chester Disease better. This gives patients hope for a better future.
Rosai-Dorfman Disease and Other Rare Histiocytic Disorders
Rare histiocytic disorders, like Rosai-Dorfman disease, need a deep understanding for good care. These conditions involve abnormal growth of histiocytes, a kind of immune cell. Rosai-Dorfman disease stands out for its unique signs and the hurdles in diagnosing and treating it.
Pathophysiology and Presentation
Rosai-Dorfman disease causes histiocytes to build up in lymph nodes and other areas. This leads to symptoms like swollen lymph nodes, fever, and weight loss. The disease can affect people in different ways, from just one area to all over the body. Knowing how it works helps doctors spot it and tell it apart from other similar diseases.
“The histopathological hallmark of Rosai-Dorfman disease is the presence of emperipolesis, where lymphocytes are seen within the cytoplasm of histiocytes,” a key sign that helps doctors diagnose it.
“emperipolesis, where lymphocytes are seen within the cytoplasm of histiocytes
Management Strategies
How to manage Rosai-Dorfman disease and other rare histiocytic disorders depends on how bad the disease is. Treatment can range from just watching it in mild cases to strong treatments like corticosteroids and chemotherapy for more serious cases. Getting a diagnosis early and creating a treatment plan that fits the patient is key to better results.
- Corticosteroids to lower inflammation
- Chemotherapy for aggressive or widespread disease
- Supportive care to manage symptoms
Eosinophilia and Hypereosinophilic Syndromes
Eosinophilia often leads to a search for its causes. These can include parasitic infections or even blood cancers. It’s marked by high eosinophil counts. These cells fight infections and play a part in allergic reactions.
When Eosinophils Indicate Serious Disease
High eosinophil counts can signal serious health issues. Hypereosinophilic syndromes (HES) are rare conditions where eosinophils are made in excess. This can harm organs if not treated.
There are many reasons for eosinophilia, such as:
- Parasitic infections
- Allergic diseases
- Malignancies, like lymphoma or leukemia
- Other blood disorders
Finding the cause of eosinophilia requires detailed tests. These include blood tests, bone marrow biopsies, and imaging. Knowing the cause helps choose the right treatment.
Treatment Approaches
Treatment for eosinophilia and HES depends on the cause and how severe it is. Treatment approaches include:
- Corticosteroids to lower eosinophil counts
- Immunomodulatory therapies to control the immune system
- Targeted therapies, like tyrosine kinase inhibitors, for certain HES types
- Supportive care to manage symptoms and prevent complications
Every patient’s situation is different. Treatment plans are made with a healthcare provider to get the best results.
When to Seek Medical Attention
Knowing when to seek help is key for patients with rare blood conditions. It’s important to recognize the signs and symptoms that mean you need to see a doctor right away.
Warning Signs and Symptoms
Certain symptoms can show that your condition is getting worse or that you’re facing an emergency. Look out for severe fatigue, unexplained bruising, and difficulty breathing. If you notice any of these, you should seek medical attention quickly.
Other signs to watch for include persistent pain, fever, or big changes in how you feel. Keep an eye on your health and tell your doctor about any symptoms that worry you.
Emergency Situations
If you have a severe reaction or anaphylaxis, you need to get help fast. Signs of anaphylaxis are swelling of the face, lips, or throat, trouble breathing, and a fast heartbeat. If you or someone you know is showing these signs, call for emergency help or go to the hospital right away.
Being ready and knowing when to act is very important for managing rare blood diseases well.
Conclusion
It’s important to understand rare blood diseases like mastocytosis to give good medical care. This article has covered many rare blood disorders. We talked about what they are, their symptoms, how to diagnose them, and how to treat them.
Mastocytosis affects patients’ lives a lot. It’s caused by too many mast cells. Knowing the signs and symptoms is key to helping patients.
We want to spread the word about these diseases. This will help doctors and patients learn more. Our aim is to support those with rare blood diseases. We want to make sure they get the care they need.
FAQ
What are rare blood diseases, and why are they a concern?
Rare blood diseases affect the blood and can be serious. They can be life-threatening if not treated quickly.
What is mastocytosis, and how does it affect patients?
Mastocytosis is when mast cells build up in tissues. This can cause skin issues and even life-threatening reactions.
How does mastocytosis present differently in adults and children?
In kids, mastocytosis often shows as skin problems. Adults may have it in many organs, making it more complex.
What is systemic mastocytosis, and what are its risks?
Systemic mastocytosis affects the bone marrow and other organs. It can be mild or severe, even life-threatening in some cases.
What are the symptoms of mastocytosis, and how is it diagnosed?
Symptoms include skin issues, stomach problems, and severe allergic reactions. Doctors use tests and biopsies to diagnose it.
What are the treatment options for mastocytosis?
Treatments aim to manage symptoms and slow disease progress. The right treatment depends on the disease’s severity.
What is polycythemia vera (PCV), and what are its complications?
PCV makes blood thick by producing too many red blood cells. This can lead to blood clots, stroke, and heart attacks.
What is paroxysmal nocturnal hemoglobinuria (PNH), and how is it treated?
PNH destroys red blood cells. Doctors use specific medicines to treat it.
What is Langerhans cell histiocytosis (LCH), and what are its treatment options?
LCH is when Langerhans cells grow too much. Treatment varies based on how severe it is.
What is Erdheim-Chester disease, and how is it diagnosed?
Erdheim-Chester disease is a rare histiocytosis affecting organs. Diagnosing it is hard and involves several tests.
When should I seek medical attention for a rare blood disease?
See a doctor if you have unexplained bleeding, bruising, or anemia. A family history of rare blood diseases is also a reason to seek help.
What is eosinophilia, and when does it indicate serious disease?
Eosinophilia means too many eosinophils in the blood. It can signal serious conditions and needs further check-ups.
What are the warning signs and symptoms of rare blood diseases?
Look out for fatigue, weight loss, and bleeding or bruising. If you notice these, get medical help right away.
References
Rare Diseases Official Database (NORD). (2025). List of Rare Diseases.
https://rarediseases.org/rare-diseases
Comprehensive resource cataloging rare blood diseases including mastocytosis, paroxysmal nocturnal hemoglobinuria (PNH), and histiocytic disorders.























