Last Updated on November 25, 2025 by

Certain medicines can cause blood to appear in the urine. The medical term for blood in urine is hematuria. It’s a sign that something might be wrong and needs to be checked. We’ll look at the types of drugs that can lead to this issue.
Some drugs can change the color of your urine or cause pink peeing. This might mean there’s a blood trace in the urinalysis. Knowing how medicines can cause hematuria is key for both patients and doctors to provide the best care.
Blood in urine, or hematuria, can range from tiny amounts to clear visible bleeding. It’s a symptom that can be caused by many factors, including some medications. Knowing about hematuria is key to figuring out its causes and what to do next.
Hematuria can show up in different ways. If you can see it, urine might look pink, red, or cola-colored because of red blood cells. Sometimes, the blood is too small to see with the naked eye, and tests are needed to find it.
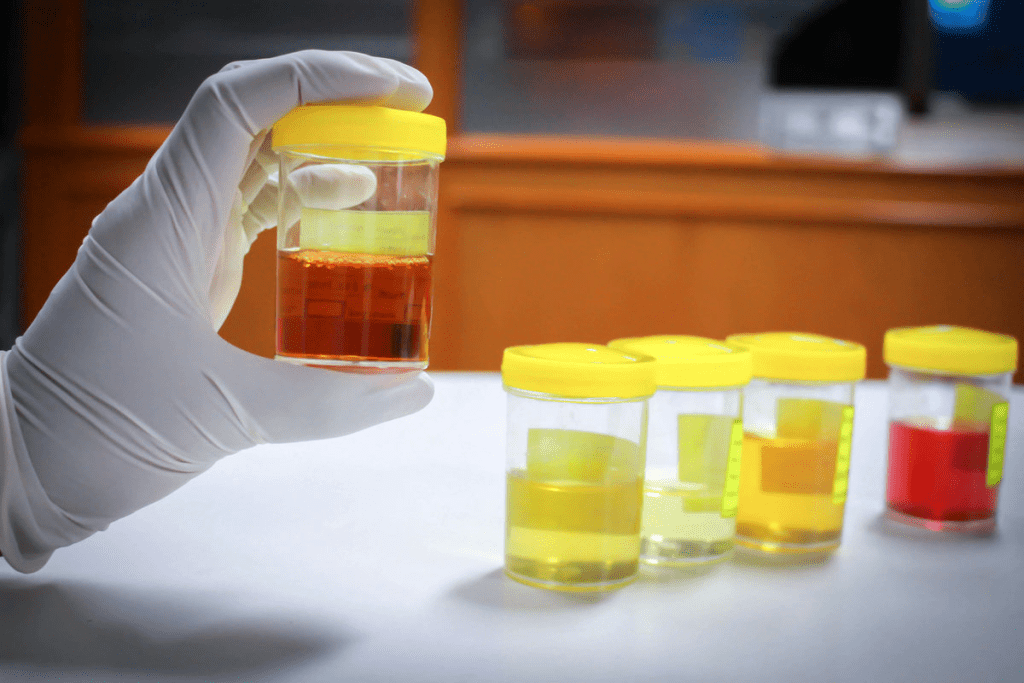
There are two main types of hematuria: visible (or gross) and microscopic. Visible hematuria makes urine look discolored because of blood. Microscopic hematuria needs a microscope to spot red blood cells in the urine. Certain medications can cause both types, making it important to see a doctor to find out why.
Hematuria is a common condition that can affect anyone at any age. Some drugs are more likely to cause it. For example, some antibiotics and anticoagulants can increase the risk of bleeding in the urine. Knowing how common and important hematuria is helps in treating it well.
We know that hematuria can mean there’s a health problem underneath. It’s vital to find out why it’s happening to give the right care. By understanding the different types and causes of hematuria, doctors can give better treatments to fix the problem.
It’s important to know how some medicines can cause bleeding in the urine. We’ll look at how drugs can lead to hematuria, which is blood in the urine.
Some medicines can directly cause bleeding in the urinary tract. For example, certain drugs can irritate the bladder or harm the kidneys, leading to blood in the urine. Chemotherapy agents can cause bleeding from the bladder, known as hemorrhagic cystitis.

Some medicines can harm the kidneys or urinary tract, causing bleeding. Nonsteroidal anti-inflammatory drugs (NSAIDs) can damage the kidneys if used too much, leading to blood in the urine. Some antibiotics can also harm the urinary tract, raising the risk of bleeding.
Some medicines change how platelets work or how blood clots. Anticoagulants are meant to stop blood clots, but can increase the risk of blood in the urine. Antiplatelet drugs also prevent platelets from forming clots.
Healthcare providers can manage patients better by knowing these effects. It’s key to watch for signs of blood in the urine and adjust treatments to lower risks.
Anticoagulant medications, like direct oral anticoagulants and traditional ones, are key in causing hematuria. They help prevent blood clots but can also lead to bleeding, including in the urinary tract.
DOACs, such as apixaban and rivaroxaban, often cause hematuria in patients. About 8.5% of those on DOACs have at least one episode of hematuria. Their fixed dosing and lack of routine monitoring make them popular for preventing stroke and treating venous thromboembolism.
Traditional anticoagulants, like warfarin, also increase the risk of hematuria. This is partly because they have a narrow therapeutic window, needing regular monitoring. Despite their effectiveness, they pose a high risk of urinary tract bleeding, mainly in patients with urological conditions.
It’s important to weigh the benefits of anticoagulation therapy against the risks, like hematuria. For patients on blood thinners, watching for signs of urinary bleeding is key. Healthcare providers must be careful in managing these patients to reduce risks.
Chemotherapy and cancer medications can cause hematuria, or blood in urine. This is a serious symptom that needs immediate medical help. We will look at how some chemotherapy agents can lead to this problem. We will also talk about what increases the risk of severe bleeding.
Cyclophosphamide is a chemotherapy drug that can cause hemorrhagic cystitis. This is a condition where the bladder bleeds. It can lead to a lot of blood in the urine, which might need medical treatment. In some cases, it has caused fatal bleeding in about 7.2% of patients, showing the need for close monitoring.
To lower this risk, patients on cyclophosphamide often get extra medications to protect their bladders. Mesna is one such drug that helps prevent bladder bleeding.
While cyclophosphamide is known for causing bladder bleeding, other drugs can also lead to hematuria. Some drugs might irritate the urinary tract or affect blood clotting. It’s key for doctors to watch for signs of bleeding in patients on chemotherapy.
Several things can make bleeding more likely in patients on chemotherapy. These include the amount and length of treatment, kidney or bladder problems, and other medications that affect blood clotting. Knowing these risk factors can help manage and possibly lower the chance of bleeding.
We suggest patients talk to their healthcare provider about their specific risks. This way, they can understand their situation better and take the right precautions.
Certain antibiotics can increase the risk of hematuria, which is blood in the urine. Hematuria can be a concerning symptom. It’s important for both patients and healthcare providers to know which antibiotics are linked to it.
Cephalosporins are a type of β-lactam antibiotic similar to penicillins. Some studies show they might raise the risk of hematuria, more so in kids. For example, a study found that some cephalosporins can cause hematuria in children.
Sulfa drugs, like sulfamethoxazole, are linked to hematuria. They’re used to fight bacterial infections. But, they can cause kidney stones or hematuria. Monitoring urinary output and ensuring adequate hydration is key when using these drugs.
“The use of sulfa drugs requires careful consideration of the risks, including hematuria, especialy in patients with pre-existing renal conditions.” “ A Nephrologist
Penicillin and related antibiotics are usually safe. But there have been cases of hematuria linked to them. The risk is low, but healthcare providers should watch for it, mainly in patients with urinary tract problems.
Nitrofurantoin is used for urinary tract infections. It’s effective but can cause side effects like hematuria. The risk is higher with long-term use or in those with kidney issues. Careful patient selection and monitoring can reduce this risk.
In summary, while antibiotics are vital for fighting infections, some increase the risk of hematuria. Knowing these risks helps in managing patient care better.
Hematuria can happen due to many medications, not just those linked to the bladder. We’ve talked about some drugs that can cause this issue. But there are other common ones to watch out for, too.
Some psychiatric drugs can lead to hematuria. For example, antipsychotic medications might affect how the body clots or irritate the urinary tract. Antidepressants, like SSRIs, can also cause urinary bleeding in rare cases.
If you’re taking these meds and notice blood in your urine, talk to your doctor right away. They can help figure out what to do next.
Many other prescription drugs can also cause hematuria. For instance, some antihypertensive medications might lead to urinary bleeding. This can happen if they change your blood pressure a lot or mix with other drugs.
It’s important to know the side effects of your medications. Always talk to your doctor about any concerns or unusual symptoms. This way, they can help you quickly.
Knowing when to get medical help is key if you see blood in your urine. Some medicines can cause this, but it often means there’s a bigger issue. You should get checked out by a doctor.
We talked about medicines that might cause blood in your urine. These include blood thinners, chemotherapy drugs, and some antibiotics. If you’re taking these and see blood, talk to your doctor right away.
If you have severe pain, a lot of bleeding, or trouble peeing, don’t wait. Getting medical help fast can help find the cause and stop worse problems.
Your doctor will look at your health, past medical issues, and medicines to figure out what to do next. Getting help when you need it means you’ll get the right care for your health.
Blood in urine, or hematuria, can show up in different ways. It might be visible, making the urine look pink, red, or cola-colored. Or, it could be microscopic, only seen through lab tests.
Some medications can lead to hematuria. This includes blood thinners and anticoagulants, chemotherapy, certain antibiotics, and psychiatric drugs.
Blood thinners and anticoagulants can cause hematuria. They affect platelet function or coagulation. This increases the risk of bleeding in the urinary tract.
Yes, some antibiotics can increase the risk of hematuria. These include cephalosporins, sulfa drugs, penicillin, and nitrofurantoin. They can damage the kidneys or urinary tract, causing bleeding.
Chemotherapy and cancer medications, like cyclophosphamide, can cause hematuria. Cyclophosphamide is linked to hemorrhagic cystitis, a serious condition that can cause significant bleeding.
If you notice blood in your urine, seek medical help right away. It could be a sign of a serious condition. See a healthcare professional if you have blood in your urine, along with pain or trouble urinating.
Yes, some medications can cause both visible and microscopic hematuria. The type and severity depend on the medication and individual factors.
Yes, certain factors can increase the risk of severe bleeding with medications like chemotherapy. These include the type and dose of the medication, as well as individual patient characteristics.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!