Last Updated on October 21, 2025 by mcelik

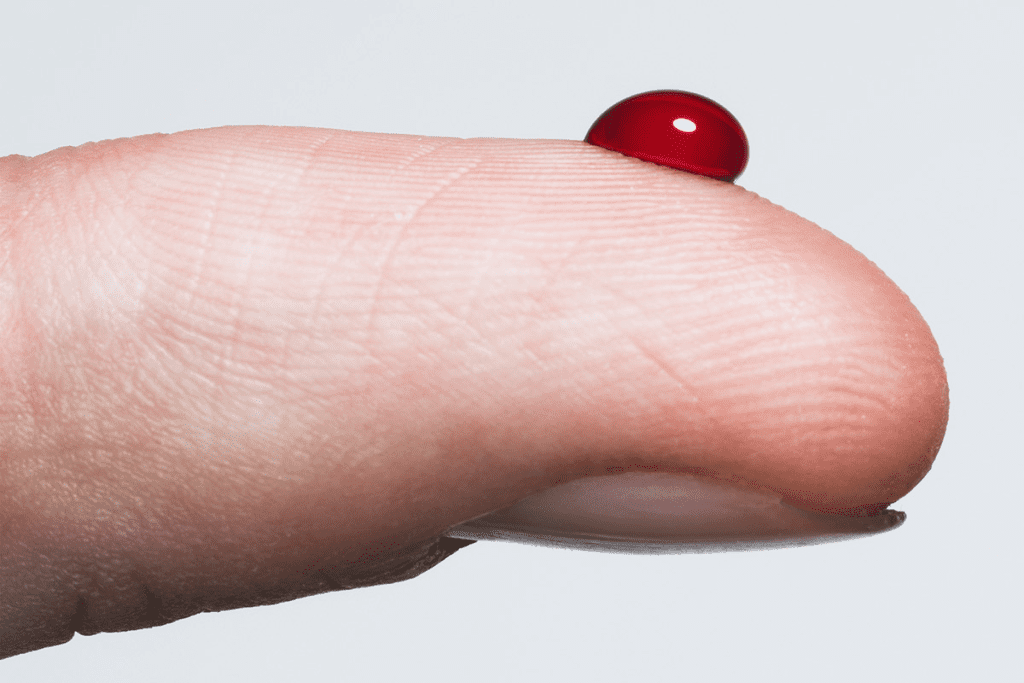
Hemolytic anemia is when red blood cells get destroyed too quickly. Did you know that some medicines can cause this? It’s a big worry in healthcare because it can cause serious problems if not handled right.
We’ll look at the medications that cause hemolytic anemia and why they are linked to this condition. This shows how important it is to manage medicines carefully. Knowing the risks and side effects helps catch and treat it early.
We’ll find out which medications that cause hemolytic anemia have been identified in research and how they affect people. By looking at the latest studies and medical knowledge, we want to give a full picture of this important health issue.
Hemolytic anemia happens when red blood cells are destroyed too quickly. This leads to a shortage of these cells. It can be caused by genetic disorders, infections, or certain medicines.
Hemolytic anemia is when red blood cells are destroyed early. Normally, they last about 120 days. But in this condition, they don’t last long.
This imbalance between making and destroying red blood cells causes anemia. The destruction can happen inside or outside blood vessels, mainly in the spleen. Knowing how hemolysis works is key to treating hemolytic anemia.
The symptoms of hemolytic anemia vary. They include feeling tired, short of breath, and having pale or yellowish skin. Dark urine is also common. In severe cases, patients might feel dizzy, have chest pain, or irregular heartbeats.
Some people might have an enlarged spleen. This is because the spleen works harder to filter out damaged red blood cells. These symptoms need a detailed medical check-up to find the cause.
Hemolytic anemia can greatly affect a person’s health. It can lower the quality of life and lead to serious problems if not treated well. Chronic hemolysis can cause iron overload, which can harm the heart and liver.
| Aspect of Health | Impact of Hemolytic Anemia |
| Quality of Life | Fatigue, shortness of breath, and other symptoms can significantly impair daily activities. |
| Organ Function | Potential for organ damage due to chronic hemolysis and iron overload. |
| Risk of Complications | Increased risk of infections, gallstones, and cardiovascular issues. |
Managing hemolytic anemia well means treating the anemia and the cause. It also means preventing complications. This approach is vital for better patient outcomes and health.
It’s important to understand how drug-induced hemolytic anemia works. This condition happens when some medicines destroy red blood cells. We’ll look at the different ways this can happen.
One way drugs cause hemolytic anemia is through immune reactions. The drug or its byproducts attach to red blood cells. This makes the immune system attack them. Medicines like penicillin and some cephalosporins can trigger this reaction.
Another way drugs can cause hemolytic anemia is through oxidative stress. Some medicines create harmful oxygen species. These can damage the red blood cell membrane. Primaquine, used to treat malaria, is a drug that can cause this damage, mainly in people with G6PD deficiency.
Drugs can also directly harm red blood cells. Some medicines change the red blood cell membrane or disrupt its functions. This can cause the cells to burst. For example, some antiviral and chemotherapy drugs can directly harm red blood cells.
Certain medications can lead to hemolytic anemia, a serious blood disorder. This happens when red blood cells are destroyed too quickly. It can cause health problems, from mild to severe.
Several types of medications increase the risk of hemolytic anemia. These include:
The risk of drug-induced hemolytic anemia varies. It depends on the drug and the patient. Genetic factors, like G6PD deficiency, can increase the risk.
Studies show drug-induced hemolytic anemia is rare but serious. It’s more common in people with certain blood disorders or genetic conditions.
To lower the risk of drug-induced hemolytic anemia, healthcare providers should:
By knowing which medications can cause hemolytic anemia and using proper risk assessment, we can lower its occurrence.
Certain antibiotics can cause hemolytic anemia, a serious blood condition. This condition makes it hard for blood to carry oxygen. We will look at which antibiotics are linked to this issue.
Penicillin is a common antibiotic. But, it can cause hemolytic anemia in some people. This happens when the body attacks the red blood cells coated with penicillin.
Key points about penicillin-induced hemolytic anemia:
Cephalosporins, another type of antibiotic, can also cause hemolytic anemia. The risk is lower than with penicillin, but cases have been reported. This is more common with certain types of cephalosporins.
Notable aspects of cephalosporin-induced hemolysis:
Sulfonamide antibiotics are used to treat many infections. They can cause hemolytic anemia in some people. This can happen due to an unusual reaction or in those with G6PD deficiency.
Important considerations for sulfonamide-induced hemolytic anemia:
We have talked about how some antibiotics can lead to hemolytic anemia. It’s important to be careful and monitor patients when using these medications.
Antimalarial drugs are key in fighting malaria. Yet, some can cause hemolytic anemia in certain people. This is when red blood cells break down too quickly. It’s a big worry for those with glucose-6-phosphate dehydrogenase (G6PD) deficiency.
Primaquine is a drug used to fight malaria. It can lead to hemolytic anemia, mainly in those with G6PD deficiency. This is because their red blood cells can’t handle oxidative stress, causing them to break down early.
Key factors contributing to primaquine-induced hemolysis include:

Chloroquine is another drug used to fight malaria. It can also cause hemolytic anemia, but the risk is lower than with primaquine. Yet, it’s a concern, mainly for those with G6PD deficiency.
“The risk of hemolysis associated with chloroquine and related compounds necessitates careful consideration before prescribing these medications, specially in regions where G6PD deficiency is prevalent.”
” World Health Organization
Before starting antimalarial drugs, it’s important to check for hemolytic anemia risk. This means:
| Risk Factor | Assessment Strategy |
| G6PD Deficiency | Screening for G6PD deficiency before starting primaquine or chloroquine |
| Medical History | Reviewing patient history for previous hemolytic episodes or relevant comorbidities |
| Dosage and Monitoring | Careful dosing and monitoring for signs of hemolysis during treatment |
Knowing the risks of antimalarial drugs and doing the right assessments can help. Healthcare providers can then lower the chance of hemolytic anemia in patients.
Sulfa drugs are a type of antibiotic that can cause hemolytic reactions in some people. They are used to fight bacterial infections but can have bad side effects for a few.
Sulfa drugs, or sulfonamides, include medicines like sulfamethoxazole and sulfasalazine. They help treat infections like urinary tract infections and pneumonia.
Some common sulfa drugs are:
Sulfa drugs cause hemolysis by creating reactive oxygen species that harm red blood cells. This is worse for people with glucose-6-phosphate dehydrogenase (G6PD) deficiency because their red blood cells can’t handle the stress well.
Sulfa-induced hemolysis is more common in those with G6PD deficiency. Their red blood cells are more likely to break down because of the sulfa drugs’ effect.
It’s important to watch patients closely who are taking sulfa drugs, even more so if they have G6PD deficiency. Before starting treatment, we do blood tests like a complete blood count (CBC) and G6PD screening.
While on treatment, look out for signs of hemolysis like jaundice, dark urine, and feeling tired. If hemolytic anemia is thought to be happening, stop the sulfa drugs and give the patient the right care.
Knowing the risks of sulfa drugs and monitoring patients carefully can help avoid hemolytic reactions. This way, we can make treatment safer for everyone.
G6PD deficiency is a genetic disorder that affects millions worldwide. It makes them more likely to get hemolytic anemia from certain medicines. This condition happens because of a lack of the glucose-6-phosphate dehydrogenase enzyme. This enzyme protects red blood cells from damage.
G6PD deficiency mostly affects males because it’s an X-linked recessive disorder. It comes from mutations in the G6PD gene, leading to less enzyme activity. This makes red blood cells more likely to break down when exposed to certain triggers, including drugs.
Key aspects of G6PD deficiency include:
Certain medications can cause hemolysis in people with G6PD deficiency. These include:
| Medication Class | Examples | Risk Level |
| Antimalarials | Primaquine, Pamaquine | High |
| Antibiotics | Sulfonamides, Nitrofurantoin | High |
| Analgesics | Aspirin (high doses) | Moderate |
Healthcare providers should know about these high-risk medications. They should also look for safer alternatives for G6PD-deficient patients.
Screening for G6PD deficiency is recommended for those at high risk. This includes people from areas with high rates of the condition, like parts of Africa, Asia, and the Mediterranean. The test measures G6PD enzyme activity in red blood cells.
Screening guidelines include:
Understanding G6PD deficiency and its effects on drug-induced hemolysis helps healthcare providers. They can then take steps to prevent hemolytic crises in at-risk patients.
Certain medications can cause an immune reaction that destroys red blood cells. This is called drug-induced immune hemolytic anemia. The immune system mistakenly sees red blood cells as foreign and attacks them. This usually happens because of a specific drug.
Immune-mediated hemolysis happens when the immune system makes antibodies against red blood cells. These antibodies mark the cells for destruction. This can start because of a drug.
Drug-dependent antibodies are a main cause. They form when a drug or its byproducts attach to red blood cells. This triggers an immune response. Another reason is the creation of autoantibodies against red blood cells. This can happen when a drug changes the antigens on the cells.
Many drugs can cause drug-induced immune hemolytic anemia. Antibiotics like penicillin and cephalosporins, anti-inflammatory drugs, and antimalarial medications are some examples. The risk depends on the drug and the patient.
To diagnose drug-induced immune hemolytic anemia, doctors use a few steps. They look at the patient’s symptoms, run lab tests, and check the patient’s medication history. Lab tests show signs of hemolysis like high LDH, low haptoglobin, and a positive DAT.
Diagnostic steps include:
Understanding how it works, knowing which drugs can cause it, and using the right tests help doctors manage drug-induced immune hemolytic anemia.
Hemolytic anemia is a condition where red blood cells are destroyed too early. It can be caused by certain blood pressure medicines. It’s important to know about these side effects.
Methyldopa is a blood pressure medicine linked to autoimmune hemolytic anemia (AIHA). AIHA happens when the immune system attacks the body’s own red blood cells. This can lead to their destruction.
A study found that methyldopa can cause AIHA in some people. This can lead to severe hemolysis, needing medical help.
“The exact mechanism of methyldopa-induced AIHA is not fully understood, but it is believed to involve the drug’s ability to alter the red blood cell membrane, making it more susceptible to immune-mediated destruction.”
Other heart medicines can also cause hemolytic anemia, but less often. This includes some beta-blockers and diuretics. Here’s a table showing some of these medicines and their risks.
| Drug Class | Specific Drug | Risk of Hemolytic Anemia |
| Centrally Acting Antihypertensives | Methyldopa | High |
| Beta-Blockers | Propranolol | Low |
| Diuretics | Hydrochlorothiazide | Low to Moderate |
It’s important for patients on these medicines to get regular checks. This helps catch hemolytic anemia early. The checks include:
Early detection and treatment of hemolytic anemia can greatly improve outcomes.
Antiviral and cancer medications are lifesavers but can cause hemolytic anemia. This happens when red blood cells are destroyed too fast. We’ll look at the medications that pose this risk and how to manage it.
Ribavirin and interferon treat hepatitis C and some viral infections. Ribavirin stops viruses from multiplying but can harm red blood cells. Interferon can trigger autoimmune reactions that harm red blood cells too.
It’s important to watch patients on these therapies closely. Regular blood tests can catch hemolytic anemia early, helping to act fast.
Chemotherapy is key in fighting cancer. But, some drugs can cause hemolytic anemia. This can happen through immune attacks or direct damage to red blood cells.
Some drugs, like platinum-based compounds and alkylating agents, are linked to this issue. The risk depends on the drug, dose, and patient health.
Managing hemolytic anemia from these medications involves several steps. Early detection through regular checks is essential. Adjusting doses or switching medications can help.
In severe cases, blood transfusions may be needed. Also, improving patient health and treating underlying conditions can lower the risk.
Managing these patients requires a team effort. Hematologists, oncologists, and other specialists should work together.
Clinical case studies offer insights into drug risks, including hemolytic anemia. They help us understand how drugs cause this condition and how to manage it.
Dapsone is used for leprosy and dermatitis herpetiformis but can cause hemolytic anemia. Several case studies show this risk is higher in patients with G6PD deficiency.
This case shows why it’s key to check for G6PD deficiency before starting dapsone.
Nitrofurantoin, used for urinary tract infections, can also cause hemolytic anemia. Case reports indicate that those with G6PD deficiency are at higher risk.
These findings stress the importance of choosing patients carefully and monitoring them when using nitrofurantoin.
Quinidine and quinine, for malaria and heart issues, can lead to drug-induced hemolytic anemia. Clinical evidence points to immune-mediated hemolysis.
These cases remind us to watch patients on these drugs for signs of hemolysis closely.
By studying these cases, healthcare providers can better understand drug risks. This knowledge helps them improve patient care and outcomes.
Diagnosing drug-induced hemolytic anemia is a detailed process. It includes lab tests, ruling out other conditions, and finding the drug that caused it. We’ll walk you through the key steps and what to consider.
Labs are key in diagnosing this condition. Tests show signs of hemolysis like high LDH and low haptoglobin. The blood smear might show schistocytes or spherocytes. Direct and indirect bilirubin levels are also checked to see if there’s hemolytic activity.
These lab results help confirm hemolysis and point to possible causes. A detailed lab check is needed for a correct diagnosis.
When diagnosing drug-induced hemolytic anemia, other causes of hemolysis must be considered. This includes autoimmune hemolytic anemia, hereditary disorders, and other acquired anemias. A detailed medical history and physical exam are essential in narrowing down the causes.
By carefully evaluating these factors, we can pinpoint the likely causes and make an accurate diagnosis.
After diagnosing hemolytic anemia, finding the drug that caused it is the next step. This involves looking closely at the patient’s medication history. In some cases, a drug challenge or rechallenge may be needed to confirm the drug, but this must be done with caution.
We must consider the risks and benefits of any diagnostic method. This ensures patient safety while trying to confirm the diagnosis.
Treating drug-induced hemolytic anemia involves quick action and ongoing care. It’s important to tackle the root cause, manage symptoms, and avoid future problems.
The first thing to do is stop the drug causing the problem. We need to check the patient’s medicines to find the culprit. Stopping the drug is key to stopping the hemolysis.
Key immediate management steps include:
Supportive care is essential in managing drug-induced hemolytic anemia. We aim to ease symptoms and help the patient recover. This includes:
In some cases, additional interventions may be needed to handle specific symptoms or complications.
In severe cases, blood transfusion might be needed. This is true when there’s significant anemia or symptoms. We decide on transfusion based on the patient’s condition and lab results.
Transfusion considerations include:
In conclusion, treating drug-induced hemolytic anemia needs a detailed plan. Understanding immediate steps, supportive care, and when to use transfusion helps us manage the condition well. This improves patient outcomes.
It’s important to know which medications can lead to hemolytic anemia. This article has covered several types, like antibiotics and antimalarial drugs. We also talked about some treatments for cancer and viruses.
Some people, like those with G6PD deficiency, are more likely to get hemolytic anemia from certain drugs. Knowing this can help prevent it. Taking steps to avoid these risks can make a big difference.
Doctors need to watch for signs of hemolytic anemia in their patients. This is true when they’re giving out drugs that might cause it. This way, they can catch and treat the problem early, helping patients get better.
In short, knowing about medications that can cause hemolytic anemia is key. Both doctors and patients need to be aware of these risks. By understanding and acting on this information, we can all help prevent drug-induced hemolytic anemia and improve care for those affected.
Hemolytic anemia is when red blood cells break down too early. Some medicines can cause this by attacking the cells, damaging them, or making them break down.
Antibiotics like penicillin, cephalosporins, and sulfonamides can lead to hemolytic anemia. They trigger an immune response that destroys red blood cells.
Primaquine and chloroquine can cause hemolytic anemia, mainly in those with G6PD deficiency. It’s important to check for G6PD deficiency before starting these medicines.
Sulfa drugs can cause hemolysis by creating oxidative stress, mostly in those with G6PD deficiency. It’s key to watch for signs of hemolysis in patients on sulfa drugs.
G6PD deficiency is a genetic disorder affecting the enzyme glucose-6-phosphate dehydrogenase in red blood cells. People with this deficiency are more likely to experience hemolysis from certain medicines, like antimalarials and sulfa drugs.
Yes, some antihypertensive drugs, such as methyldopa, can lead to autoimmune hemolytic anemia. It’s important to monitor patients on these medications for signs of hemolysis.
Yes, some antiviral drugs like ribavirin and interferon, and certain cancer treatments, can cause hemolytic anemia. It’s vital to watch for signs of hemolysis and adjust treatment as needed.
Diagnosis requires lab tests showing signs of hemolysis and a detailed medical history to find the cause. It’s also important to rule out other causes of hemolytic anemia.
Treatment includes stopping the medicine causing the problem, supportive care, and sometimes blood transfusions. It’s critical to monitor patients for signs of hemolysis and adjust treatment as necessary.
To reduce risk, screen patients carefully, test for G6PD deficiency, watch for signs of hemolysis, and choose safer alternatives when possible.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!