Last Updated on October 31, 2025 by
Managing atrial fibrillation well needs a full plan, and medicine is key. It’s important to control symptoms and stop complications for those with this condition.
Medicines are often the main treatment for AFib. They try to control heart rate, get the heart back to normal, and stop stroke. At Liv Hospital, we focus on trusted, patient-focused care. We use advanced methods and meet international standards in managing AFib.
Looking into the different drugs for treat AFib, how they work, and their side effects helps us understand our options. This way, we can make smart choices about our care.
Explore 12 medications to treat AFib and how they help control heart rate, rhythm, and prevent atrial fibrillation attacks.
Key Takeaways
- Medicines are a main treatment for AFib, aiming to control heart rate and prevent stroke.
- Liv Hospital provides patient-centered care for AFib management.
- Knowing the medicines available and their effects is key for good management.
- AFib treatment involves controlling heart rate and restoring normal sinus rhythm.
- Preventing thromboembolic events is a key part of AFib management.
Understanding Atrial Fibrillation and the Need for Medication
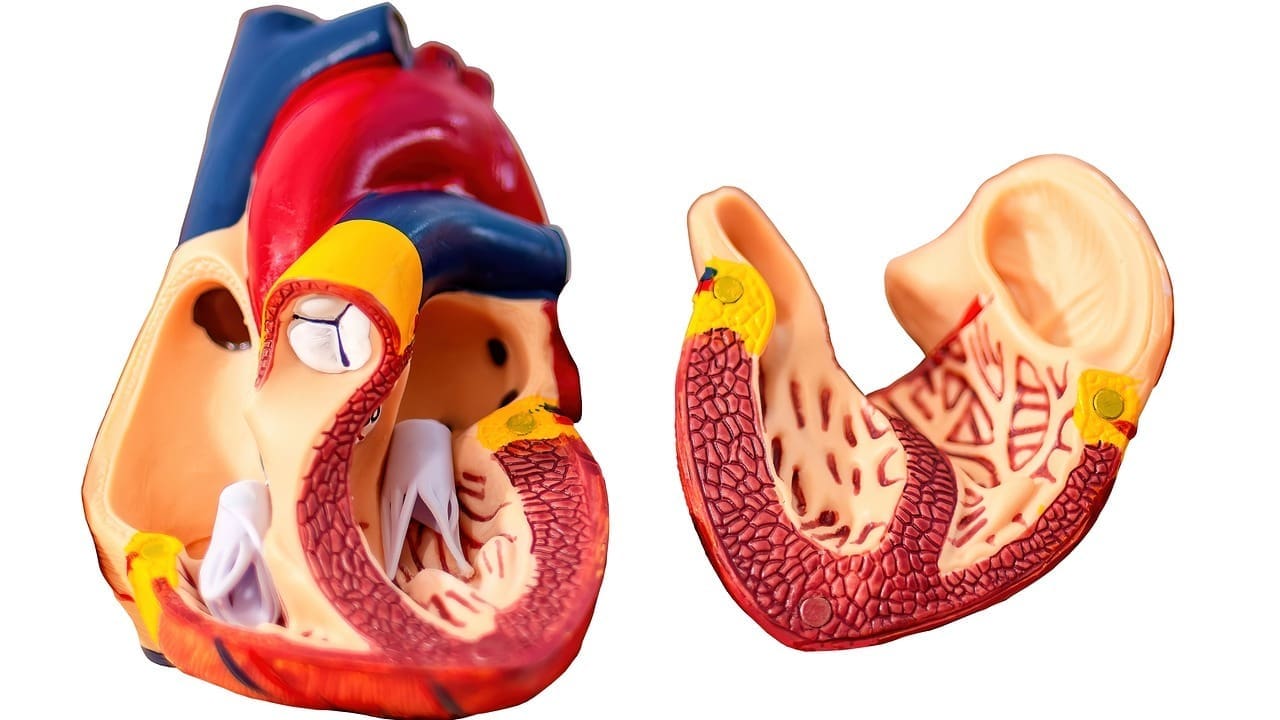
It’s important to know about atrial fibrillation to understand why medication is needed. Atrial fibrillation, or AFib, is a heart condition where the heart beats too fast and irregularly.
The heart’s upper chambers (atria) don’t beat in sync with the lower chambers (ventricles) during AFib. This can cause blood to pool, increasing the risk of blood clots.
What Happens During Atrial Fibrillation
In a normal heart, the atria contract in sync, pumping blood into the ventricles. But in AFib, the atria quiver instead of beating well. This leads to irregular ventricular contractions, causing symptoms like palpitations, shortness of breath, and fatigue.
Complications of Untreated Atrial Fibrillation
If AFib is not treated, it can lead to serious problems. The biggest risk is stroke, which happens when a blood clot forms in the heart and goes to the brain. Other issues include heart failure and a lower quality of life due to ongoing symptoms.
AFib patients face a much higher risk of stroke than those without the condition. Studies show AFib can increase stroke risk by four to five times.
| Complication | Description | Risk Factor |
| Stroke | Blood clot forms in the heart and travels to the brain | 4-5 times higher in AFib patients |
| Heart Failure | The heart is unable to pump enough blood to meet the body’s needs | Increased due to irregular heartbeats |
| Decreased Quality of Life | Persistent symptoms such as palpitations and shortness of breath | Common in untreated AFib |
Goals of Medication Therapy
The main goals of medication for AFib are to control heart rate, restore normal sinus rhythm, and prevent stroke. Medications are key in reaching these goals and improving life for AFib patients.
Understanding AFib and treatment goals helps healthcare providers create effective plans for each patient.
Categories of Atrial Fibrillation Treatment Drugs

AFib treatment includes several drug types, each tackling different parts of the condition. Knowing these categories is key for good treatment.
Rate-Control Medications
Rate-control meds are vital in managing AFib. They help control the heart rate, improving symptoms and life quality. Beta-blockers and calcium channel blockers are common. They slow the heart rate, easing symptoms like palpitations and shortness of breath.
Rhythm-Control (Antiarrhythmic) Medications
Rhythm-control meds, or antiarrhythmics, aim to keep the heart in a normal rhythm. They’re great for those who keep feeling symptoms even with rate-control meds. Amiodarone, sotalol, and flecainide are examples. But, they need close watch because of possible side effects.
Anticoagulants for Stroke Prevention
Anticoagulants are key in stopping strokes, a big risk with AFib. They stop blood clots that could cause strokes. Warfarin and direct oral anticoagulants (DOACs) are used. The right choice depends on the patient’s risk and what they prefer.
In short, treating AFib involves using rate-control, rhythm-control meds, and anticoagulants. Each type has its own benefits and things to consider. The right drug choice depends on the patient’s specific needs and situation.
Beta-Blockers: Metoprolol and Atenolol
Beta-blockers are key in managing atrial fibrillation by controlling heart rate. They block epinephrine’s effect on the heart. This reduces heart rate and contraction force.
This is good for atrial fibrillation patients. It helps with symptoms like palpitations, shortness of breath, and fatigue.
How Beta-Blockers Work for Atrial Fibrillation
Beta-blockers work by blocking beta-adrenergic receptors in the heart. This action lowers heart rate and contraction force. It helps manage atrial fibrillation symptoms.
“Beta-blockers are effective in controlling heart rate and improving symptoms in patients with atrial fibrillation,” as noted in clinical guidelines.
By controlling the ventricular rate, beta-blockers improve exercise tolerance. They also reduce the risk of tachycardia-induced cardiomyopathy. They are often the first choice for rate control in atrial fibrillation.
Metoprolol: Dosage and Administration
Metoprolol is a common beta-blocker for atrial fibrillation. Dosage varies based on the patient’s condition and response. The initial dose is usually 25-50 mg twice daily.
The dose can be adjusted based on heart rate response. The goal is a resting heart rate of 60-80 bpm.
Metoprolol comes in immediate-release and extended-release tablets. The extended-release version allows for once-daily dosing. This improves patient adherence.
Atenolol: Dosage and Administration
Atenolol is another beta-blocker for atrial fibrillation management. The starting dose is 25-50 mg once daily. The dose may be increased based on heart rate response.
The typical maintenance dose is 50-100 mg daily. Atenolol is generally well-tolerated. But, dose adjustments may be needed in patients with renal impairment.
Side Effects and Precautions
Beta-blockers are generally safe but can cause side effects. Common side effects include fatigue, dizziness, and cold extremities. Serious side effects like bradycardia and hypotension can also occur.
Patients with asthma or severe COPD should use beta-blockers with caution. They can worsen respiratory symptoms. Regular monitoring is key to ensure safe use and adjust dosages as needed.
Calcium Channel Blockers: Verapamil and Diltiazem
Calcium channel blockers are key in managing atrial fibrillation (AFib). They control heart rate by blocking calcium ions in heart and blood vessels. This leads to wider blood vessels and a slower heart rate.
Mechanism of Action in Atrial Fibrillation
Calcium channel blockers work by stopping calcium ions from entering heart and blood vessel muscles. This action slows down the heart rate. It helps reduce symptoms like irregular heartbeat, shortness of breath, and tiredness.
Verapamil: Usage Guidelines
Verapamil is a common drug for controlling heart rate in AFib. The starting dose is 40-80 mg, taken three or four times a day. The dose can be adjusted up to 480 mg daily. It comes in immediate and extended-release forms for different dosing needs.
Diltiazem: Usage Guidelines
Diltiazem is another drug for managing AFib. The initial dose is 30-60 mg, taken three or four times a day for immediate-release. For sustained-release, it starts at 120-180 mg once a day. The dose can be increased up to 360 mg daily for sustained-release.
Common Side Effects and Contraindications
Side effects of these drugs include dizziness, headaches, constipation, and swelling in the legs. Verapamil often causes more constipation than diltiazem. Both can lower blood pressure and should be used carefully in heart failure patients. They are not recommended for those with sick sinus syndrome, severe low blood pressure, or advanced heart block.
Digoxin for Heart Rate Control in Atrial Fibrillation
Digoxin is key in managing heart rate for people with atrial fibrillation. It’s used in certain situations. We’ll look at how it works, the right dosage, and its role in treating AFib today.
Regulating Heart Rate
Digoxin helps control heart rate by making heart contractions stronger. It slows the heart rate by affecting the AV node. This is done by blocking the sodium-potassium ATPase pump.
It’s most helpful for those with heart failure or who don’t move much. But, it might not work as well when the body is stressed or during exercise.
Dosing and Monitoring
Getting the right dose of digoxin is very important. The starting dose is usually between 0.125 to 0.25 mg a day. Adjustments are made based on how the patient responds and their digoxin levels.
It’s also important to check serum digoxin levels, kidney function, and electrolytes. This helps avoid too much digoxin.
Limitations and Toxicity Concerns
Digoxin has its downsides. Its safe range is very narrow. This means a small increase can be harmful. Kidney problems, imbalances in electrolytes, and other drugs can raise the risk of toxicity.
Signs of too much digoxin include nausea, vomiting, confusion, and irregular heartbeats. Keeping a close eye on patients and adjusting doses carefully is key to avoiding these issues.
Role in Modern AFib Management
In today’s treatment of atrial fibrillation, digoxin is often paired with other medications. It’s not usually the first choice because of its risks and limited effectiveness in some. Yet, it’s valuable for certain patients.
For example, those with heart failure or who can’t take other medications might benefit from digoxin. It’s a useful tool for doctors to manage heart rate in AFib.
| Aspect | Digoxin | Beta-Blockers | Calcium Channel Blockers |
| Mechanism of Action | Increases vagal tone, decreases AV node conduction | Reduces heart rate by blocking beta-adrenergic receptors | Slows heart rate by inhibiting calcium influx into cardiac muscles |
| Primary Use in AFib | Heart rate control, specially in heart failure | Heart rate control, rhythm control in some cases | Heart rate control, some effect on rhythm |
| Monitoring Requirements | Serum digoxin levels, renal function, electrolytes | Heart rate, blood pressure, ECG | Heart rate, blood pressure, ECG |
| Potential Side Effects | Toxicity (nausea, vomiting, arrhythmias), renal issues | Fatigue, dizziness, bronchospasm | Edema, constipation, dizziness |
Amiodarone: Powerful Antiarrhythmic for Atrial Fibrillation
Amiodarone is a strong antiarrhythmic drug for treating atrial fibrillation (AFib). It helps keep the heart rhythm normal. Knowing how it works is key to treating AFib well.
Unique Properties and Mechanism of Action
Amiodarone is special because it affects many heart channels. It blocks potassium, sodium, and calcium channels. It also has beta-blocking effects. This makes it great for keeping the heart rhythm steady in AFib patients.
Key benefits of amiodarone include:
- High efficacy in maintaining sinus rhythm
- Effective in patients with various heart conditions
- Can be used in patients with heart failure
Dosing Strategies and Administration
Starting amiodarone needs careful thought. We use a loading dose first, then a maintenance dose. The loading dose is 800-1600 mg daily for 1-3 weeks. The maintenance dose is 200-400 mg daily.
Amiodarone has a long half-life. This means it’s given once a day. But, it takes time to reach the right levels in the body.
Long-term Monitoring Requirements
Long-term checks are vital because of amiodarone’s side effects. We watch thyroid, liver, lung, and heart function closely. This includes regular ECGs to check the heart’s rhythm.
Managing Possible Organ Toxicities
Amiodarone is effective but can harm organs. We watch for thyroid, liver, and lung problems. Regular checks and patient education help manage these risks.
By understanding amiodarone’s special features and managing its use carefully, we can treat AFib well. This helps avoid serious problems.
Dronedarone: A Newer Alternative for Rhythm Control
Dronedarone is a newer choice for managing atrial fibrillation. It’s an antiarrhythmic drug designed to be safer than older options.
Development and Relation to Amiodarone
Dronedarone is similar to amiodarone but aims to have fewer side effects. It was made by removing iodine from amiodarone, which caused many side effects.
Here are the main differences between dronedarone and amiodarone:
- Less iodine means fewer thyroid problems
- It has a shorter half-life, which might reduce long-term risks
- It’s metabolized differently, which could lower the risk of drug interactions
Appropriate Patient Selection
Choosing the right patients for dronedarone is key. It’s best for those with paroxysmal or persistent atrial fibrillation. It’s also good for those who can’t take amiodarone.
Criteria for patient selection include:
- History of atrial fibrillation
- Can’t take amiodarone
- No advanced heart failure (NYHA Class III or IV)
- No significant left ventricular dysfunction
Dosing and Administration Guidelines
The dose of dronedarone is 400 mg twice daily, taken with meals. Taking it with food helps with absorption.
Important guidelines for administration include:
- Take with food to improve absorption
- Avoid grapefruit products, as they can interact with dronedarone
- Check ECG regularly, mainly during the start of treatment
Safety Profile and Monitoring Requirements
Dronedarone is generally safe but can cause side effects and has certain contraindications. Regular monitoring is needed for safe use.
Common side effects include:
- Diarrhea
- Nausea
- Abdominal pain
Monitoring needs include:
- Regular ECG to check for QT prolongation
- Liver function tests
- Pulmonary function assessment if symptoms arise
In conclusion, dronedarone is a valuable option for rhythm control in atrial fibrillation. It offers a safer choice than older drugs. Careful patient selection and monitoring are vital to ensure its benefits and minimize risks.
Sotalol and Flecainide: Important Atrial Fibrillation Treatment Drugs
For those with Atrial Fibrillation, Sotalol and Flecainide are key treatments. We’ll look at how they work, their success rates, and their safety.
Sotalol: Combined Beta-Blocker and Antiarrhythmic Effects
Sotalol is special because it has two benefits. It controls heart rate and keeps the heart rhythm steady in AFib patients.
Mechanism of Action: It makes the heart’s action longer and less likely to go out of rhythm.
Flecainide: Class IC Antiarrhythmic
Flecainide is a Class IC antiarrhythmic drug. It’s great at keeping the heart rhythm normal.
How it Works: It slows down heart signals. This stops arrhythmias without changing how long the heart’s action lasts.
Comparing Efficacy and Safety Profiles
Both Sotalol and Flecainide work well, but they’re not the same in safety. Sotalol can cause a dangerous heart rhythm called Torsades de Pointes. Flecainide might make heart problems worse or cause arrhythmias.
Choosing Between Them: The right choice depends on the patient’s heart health, any heart disease, and how likely they are to have arrhythmias again.
Anticoagulants: Warfarin vs. Novel Agents
Anticoagulants have changed how we treat atrial fibrillation, greatly reducing stroke risk. They are key in preventing strokes in patients with atrial fibrillation. Choosing between warfarin and newer DOACs depends on the patient’s health, other medications, and the anticoagulant’s features.
Warfarin: The Traditional Approach
Warfarin has been a mainstay in anticoagulation for years. It blocks vitamin K-dependent clotting factors in the liver. But, it needs regular INR checks to keep blood clotting right.
Key considerations for warfarin use include:
- Regular INR monitoring
- Dietary restrictions due to vitamin K interactions
- Potential for drug interactions
Direct Oral Anticoagulants (DOACs)
DOACs like dabigatran, rivaroxaban, and apixaban are easier to use than warfarin. They don’t need INR checks and are as good as warfarin in preventing strokes. They might also lower the risk of major bleeding.
Benefits of DOACs:
- No routine coagulation monitoring required
- Fewer dietary restrictions
- Less likely to interact with certain drugs
Choosing the Right Anticoagulant
Choosing between warfarin and DOACs depends on the patient’s health, other medications, and medical conditions. For example, dabigatran is not for patients with mechanical heart valves. Rivaroxaban and apixaban are safer for those with kidney problems.
When picking an anticoagulant, we look at:
- Patient’s renal function
- Presence of other medical conditions
- Potential drug interactions
- Patient preference and adherence
The final decision is made with a healthcare provider, considering the latest guidelines and the patient’s needs.
Medication Strategies for AFib with Rapid Ventricular Response
Atrial Fibrillation with Rapid Ventricular Response is a serious condition. It needs quick and effective treatment to control the heart rate and prevent complications. This condition is marked by an irregular and often rapid heart rate.
It can cause symptoms like palpitations, shortness of breath, and fatigue. If not managed, it can lead to heart failure and stroke.
Acute Management of AFib with RVR
The acute management of AFib with RVR aims to quickly control the heart rate. This helps alleviate symptoms and prevent immediate complications. We use intravenous medications for this purpose.
Drugs to lower heart rate like beta-blockers (e.g., metoprolol) and calcium channel blockers (e.g., diltiazem) are commonly used. These medications quickly reduce the ventricular rate. This improves cardiac output and reduces symptoms.
In some cases, if the patient is unstable, immediate cardioversion may be needed. But for stable patients, pharmacological control is usually the first step.
| Medication | Dose | Onset of Action |
| Metoprolol | 2.5-5 mg IV over 2 min | Within minutes |
| Diltiazem | 0.25 mg/kg IV over 2 min | Within minutes |
Long-term Control Strategies
After managing the acute phase, long-term control strategies are implemented. Oral medications are used for long-term management. AFib medication names like beta-blockers, calcium channel blockers, and digoxin are commonly prescribed.
The choice of medication depends on the patient’s health, any contraindications, and the specifics of their AFib.
For some, rhythm control strategies may be more suitable. This involves using antiarrhythmic drugs to maintain sinus rhythm. The decision between rate and rhythm control is based on patient factors and preferences.
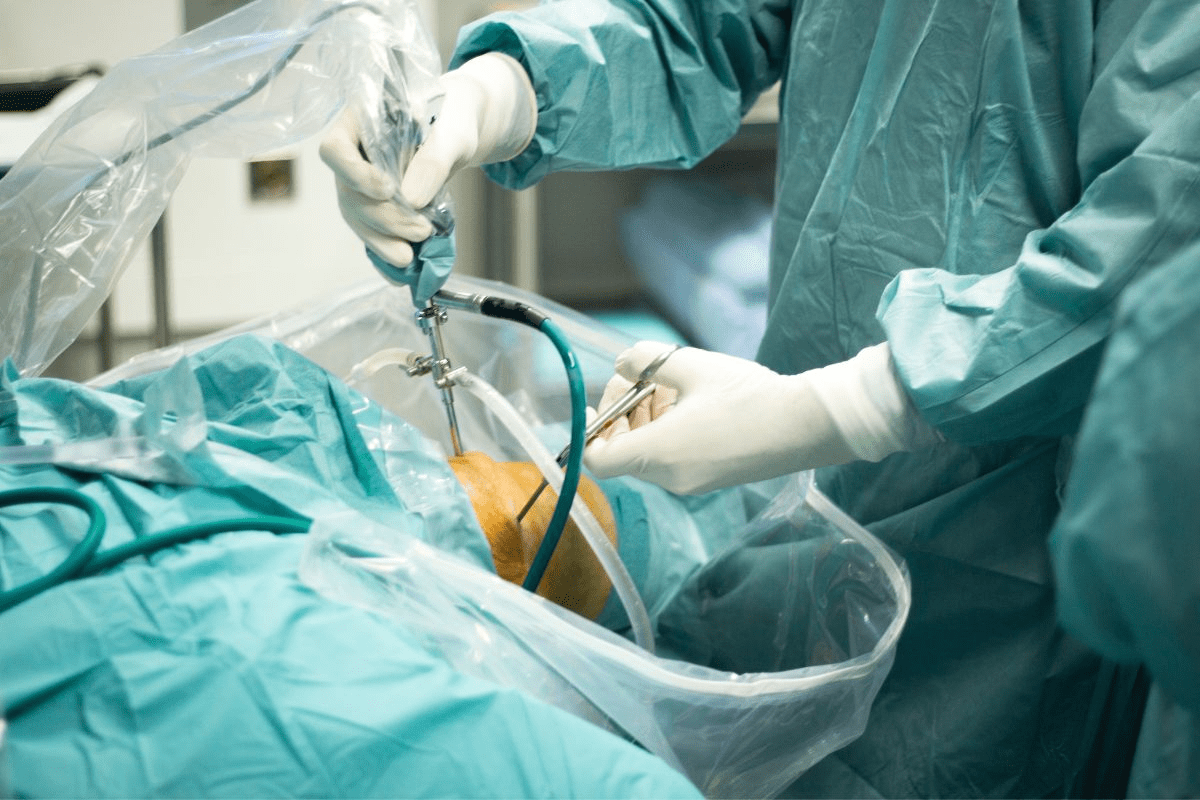
When to Consider Cardioversion or Ablation
In cases where pharmacological management is ineffective or not tolerated, or when symptoms persist despite rate control, we consider cardioversion or catheter ablation. Cardioversion uses electrical shocks to restore a normal heart rhythm. Catheter ablation destroys the abnormal electrical pathways in the heart.
These procedures are considered for patients with persistent symptoms or those at high risk of complications from AFib. The choice between cardioversion and ablation depends on various factors, including the duration of AFib, patient preference, and underlying heart disease.
Personalized Approaches to Atrial Fibrillation Management
Managing atrial fibrillation (AFib) needs a personalized approach. We tailor treatments to each patient’s unique situation. This includes their health conditions, symptoms, and lifestyle.
Patient-Specific Factors in Medication Selection
We look at many factors when picking AFib meds. These include heart failure, high blood pressure, and kidney health. For example, those with kidney problems might need different doses of certain drugs. Careful consideration of these factors helps us choose the best treatment.
Combination Therapy Approaches
Managing AFib often means using more than one medication. We might use drugs to control heart rate and prevent blood clots together. Finding the right mix helps control symptoms and prevent problems.
Monitoring Treatment Efficacy
Keeping a close eye on treatment results is key. We track heart rate, rhythm, and symptoms. We also watch for side effects. Based on this, we adjust the treatment plan as needed.
Lifestyle Modifications to Enhance Medication Effectiveness
Lifestyle changes are also vital in managing AFib. We suggest a healthy weight, regular exercise, and a heart-healthy diet. Drinking less alcohol and caffeine can also help manage symptoms.
By combining personalized meds with lifestyle changes, we can greatly improve AFib outcomes.
Conclusion
Atrial fibrillation treatment drugs are key in managing AFib, a common heart rhythm disorder. We’ve looked at different types of medication, like rate-control drugs and anticoagulants. These help prevent strokes.
It’s important to know how these drugs work and their side effects. This knowledge helps us choose the best treatment for each patient. This way, we can make their symptoms better and their lives better too.
Medicines like beta-blockers and amiodarone help control heart rate. Anticoagulants, like warfarin, prevent strokes. These are all important for treating AFib.
By using the right medication and lifestyle changes, we can help patients with AFib a lot. This approach improves their health and lowers the risk of serious problems.
FAQ
What are the primary goals of medication therapy in managing atrial fibrillation?
The main goals are to control heart rate and restore normal rhythm. Also, preventing stroke is key.
What classes of medications are used to manage atrial fibrillation?
Various medications are used. These include rate-control drugs, rhythm-control drugs, and anticoagulants to prevent stroke.
How do beta-blockers work in managing atrial fibrillation?
Beta-blockers slow the heart rate by reducing heart stimulation. Metoprolol and atenolol are often used.
What are the common side effects of calcium channel blockers used in atrial fibrillation management?
Side effects include vasodilation and possible heart weakening. Verapamil and diltiazem are common examples.
How does digoxin regulate heart rate in atrial fibrillation?
Digoxin boosts heart strength and slows rate. It does this by affecting the sodium-potassium ATPase pump.
What are the unique properties of amiodarone in managing atrial fibrillation?
Amiodarone is very effective in keeping the heart in rhythm. Its broad activity makes it stand out.
How do direct oral anticoagulants (DOACs) compare to warfarin in stroke prevention for atrial fibrillation?
DOACs are easier to use than warfarin. They are as good or better at preventing stroke.
What is the role of anticoagulation therapy in managing atrial fibrillation?
Anticoagulation is vital to prevent stroke. The choice between warfarin and DOACs depends on the patient.
How is atrial fibrillation with rapid ventricular response (RVR) managed acutely?
Acute management uses intravenous medications. Beta-blockers or calcium channel blockers are often used.
What lifestyle modifications can enhance the effectiveness of medications in managing atrial fibrillation?
Healthy weight, managing blood pressure, and less alcohol help. These lifestyle changes boost medication effectiveness.
What factors influence the selection of medications for atrial fibrillation management?
Many factors are considered. These include health conditions, other medications, and personal preferences.
References
- Unger, T., Borghi, C., Charchar, F., et al. (2024). 2023 ESH Guidelines for the management of arterial hypertension. European Heart Journal, 44(33), 3328–3441. https://pmc.ncbi.nlm.nih.gov/articles/PMC12027560/