Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we know how tough metastatic colorectal cancer (mCRC) can be. We focus on a detailed, custom treatment plan for each patient. Our team uses chemotherapy, targeted therapies, and immunotherapy along with surgery and interventional radiology to help patients get the best results. Explore the latest metastatic colon cancer therapy options and treatment advancements.
Figuring out if you have metastatic colon cancer takes several steps. We use imaging tests, lab tests, genetic testing, and tissue samples. We make sure each treatment plan fits the patient’s specific needs, using the newest medical discoveries.
We aim to give top-notch healthcare with full support for international patients. We believe in evidence-based care. We work with patients to offer hope and support during their treatment.
Key Takeaways
- Comprehensive treatment plans for metastatic colorectal cancer
- Multidisciplinary team approach at Liv Hospital
- Importance of molecular profiling in guiding treatment selection
- Combination of chemotherapy, targeted therapies, and immunotherapy
- Role of surgery and interventional radiology in treatment
Understanding Metastatic Colorectal Cancer

It’s key to understand metastatic colorectal cancer to improve treatment plans. This cancer spreads from the colon or rectum to other parts of the body. It can go to the liver, lungs, or distant lymph nodes.
Definition and Staging
The staging of metastatic colorectal cancer uses the TNM system. It looks at the tumor size (T), nearby lymph nodes (N), and distant spread (M). Stage IV means the cancer has spread to distant organs or tissues.
Getting the cancer’s stage right is vital. It helps doctors know what to expect and how to treat it. Now, doctors use molecular profiling to pick the best treatments. This has led to better results for patients with advanced disease.
Prevalence and Impact
Metastatic colorectal cancer is a big challenge. It affects patients’ quality of life and how long they live. Many patients are diagnosed when the cancer is already advanced.
The management of metastatic colorectal cancer needs a team effort. It includes medicines, targeted treatments, and sometimes surgery. Even though it’s not curable, there are times when surgery to remove metastases might be an option.
By grasping the details of metastatic colorectal cancer, we can make treatment plans that fit each patient. This helps improve outcomes for those facing this tough disease.
The Importance of Comprehensive Treatment Approaches

Metastatic CRC is complex and needs a detailed treatment plan. It’s important to address each patient’s unique needs. This ensures effective management of metastatic colorectal cancer.
Multidisciplinary Team Approach
A team of specialists is key in treating metastatic CRC. We have experts in medical oncology, surgical oncology, and more. They work together to create a detailed treatment plan.
This team effort helps us make accurate diagnoses and tailor treatments. It also lets us use the latest metastatic rectal cancer therapy options. This ensures patients get the best care available.
Individualized Treatment Planning
Every patient’s treatment plan is unique. We look at the cancer’s spread, the patient’s health, and genetic factors. We also consider the patient’s preferences and goals.
We discuss each patient in team meetings to get all perspectives. This helps us create a treatment plan that fits each patient’s needs. It aims to improve their chances of a good outcome.
Our approach combines a team effort with personalized plans. This way, we offer better care for patients with metastatic colorectal cancer. It’s vital for managing the complexities of metastatic CRC treatment effectively.
Molecular Profiling: The Foundation of Modern mCRC Treatment
In today’s world of precision medicine, molecular profiling is key for treating metastatic colorectal cancer (mCRC). It helps doctors choose the best treatments for each patient. This approach makes treatments more effective and improves patients’ lives.
Biomarker Testing
Biomarker testing is a big part of molecular profiling in mCRC. Important biomarkers include RAS and BRAF mutations. These mutations help decide which treatments to use.
RAS mutations are found in about 50% of colorectal cancers. They make some treatments less effective. BRAF mutations, found in about 10% of mCRC cases, often mean a tougher fight but can be treated with specific therapies.
To test biomarkers, doctors analyze tumor samples. These samples come from biopsies or surgeries. Advanced tests like next-generation sequencing (NGS) give detailed genetic information.
How Molecular Profiles Guide Treatment Decisions
Molecular profiles help doctors choose the right treatments. For example, patients with RAS wild-type tumors might get anti-EGFR therapies. Those with BRAF V600E mutations could get BRAF-targeted treatments.
Using molecular profiles in treatment plans makes care more personal and effective. Doctors can tailor treatments based on each tumor’s unique genetic makeup. This leads to better treatment choices, including targeted therapies and chemotherapy.
As research grows, so will the role of molecular profiling in mCRC treatment. New biomarkers and treatments are on the horizon. Keeping up with these advances is vital for effective mCRC treatment.
Systemic Chemotherapy for Metastatic Colon Cancer Therapy
Systemic chemotherapy is a key treatment for metastatic colon cancer. It offers several options to fight the disease. This approach helps improve patient outcomes and quality of life.
First-Line Chemotherapy Regimens
Many patients start with a combination chemotherapy regimen. FOLFOX and FOLFIRI are common choices. The right regimen depends on the patient’s health and tumor characteristics.
We look at patient-specific factors when picking a first-line treatment. For example, genetic profiles can influence the best regimen.
| Regimen | Components | Common Use |
| FOLFOX | 5-fluorouracil, leucovorin, oxaliplatin | First-line treatment for metastatic colon cancer |
| FOLFIRI | 5-fluorouracil, leucovorin, irinotecan | First-line or second-line treatment, depending on previous therapies |
Second-Line and Beyond Options
When first-line therapy fails, we explore second-line options. This might mean switching to a new regimen or adding targeted therapy.
Trifluridine/tipiracil is used in later treatment lines. It’s good for patients who’ve had other therapies.
Managing Side Effects
It’s important to manage chemotherapy side effects to keep patients’ quality of life high. Side effects like nausea, fatigue, and neuropathy are common. We use anti-nausea meds and adjust doses to help.
Teaching patients about side effects and how to manage them is key. This helps them cope with their treatment better.
Anti-EGFR Targeted Therapies
Anti-EGFR targeted therapies are key in treating metastatic colorectal cancer (mCRC). They have greatly improved treatment results for patients with certain molecular profiles.
Cetuximab and Panitumumab
Cetuximab and panitumumab are the main anti-EGFR drugs for mCRC. Cetuximab is a chimeric monoclonal antibody, and panitumumab is a fully human monoclonal antibody. Both target the EGFR, which is often high in colorectal cancer cells.
These drugs differ in how they are given and their side effects. Cetuximab starts with a big dose and then weekly doses. Panitumumab is given every two weeks. The choice depends on the patient and what the doctor prefers.
RAS Wild-Type Patient Selection
Choosing the right patients for anti-EGFR therapy is key. It’s based on the RAS gene’s mutational status (KRAS and NRAS). RAS wild-type status is needed for anti-EGFR treatment. RAS mutations make EGFR therapy less effective.
- Biomarker testing for RAS mutations is essential before starting anti-EGFR treatment.
- Patients with RAS wild-type mCRC can get anti-EGFR therapy.
- Testing RAS beyond KRAS exon 2 is recommended to check eligibility.
Efficacy and Side Effect Management
Anti-EGFR therapies have shown great results in improving survival and stopping cancer growth in RAS wild-type mCRC. Common side effects include:
- Skin rash (acneiform rash)
- Hypomagnesemia
- Fatigue
- Diarrhea
Managing these side effects is important to keep patients on treatment and improve their quality of life. Treating skin rash early and checking magnesium levels can help.
By choosing the right patients and managing side effects, we can make anti-EGFR therapies more effective in treating metastatic colorectal cancer.
Anti-VEGF Agents in mCRC Treatment
Anti-VEGF agents have changed how we treat metastatic colorectal cancer. They target therapy to the tumor. These agents block vascular endothelial growth factor (VEGF), a key protein in making new blood vessels for tumors.
Bevacizumab is a well-known anti-VEGF agent for mCRC. Studies show it improves patient outcomes.
Bevacizumab Across Treatment Lines
Bevacizumab is used in many treatment lines for mCRC. It’s often paired with chemotherapy. This makes it useful from the start to later treatments.
| Treatment Line | Bevacizumab + Chemotherapy | Overall Response Rate |
| First-line | FOLFOX or FOLFIRI | 45-60% |
| Second-line | FOLFIRI or IRIS | 20-40% |
Combination Strategies
Bevacizumab is often paired with other treatments. This includes chemotherapy regimens like FOLFOX or FOLFIRI.
Combination therapy offers:
- Higher response rates
- Longer time without disease progression
- Possible better survival rates
Patient Monitoring Requirements
Monitoring patients on bevacizumab is key. It helps manage side effects and ensures safety. This includes checking blood pressure, kidney function, and for signs of bleeding or blood clots.
Monitoring includes:
- Blood pressure checks
- Urine protein testing
- Complete blood counts
BRAF-Targeted Therapy Combinations
BRAF-targeted therapy combinations have changed how we treat BRAF V600E-mutated metastatic colorectal cancer. These treatments have greatly improved patient outcomes. They offer new hope where traditional chemotherapy has failed.
Encorafenib Plus Cetuximab
The mix of Encorafenib and Cetuximab is a strong treatment for BRAF V600E-mutated metastatic colorectal cancer. Studies show it boosts survival and response rates over traditional chemotherapy.
Benefits of this mix include:
- Improved overall survival rates
- Enhanced response rates
- Better tolerability compared to some traditional chemotherapy regimens
mFOLFOX6 Combinations
The mFOLFOX6 regimen, paired with targeted therapies, shows promise in treating BRAF V600E-mutated metastatic colorectal cancer. It combines oxaliplatin, leucovorin, and 5-fluorouracil in a complex chemotherapy regimen.
Advantages of mFOLFOX6 combinations include:
- Potential for improved progression-free survival
- Synergistic effects when combined with targeted therapies
- Flexibility in treatment sequencing
ASCO 2025 Updates for BRAF V600E-Mutated mCRC
The American Society of Clinical Oncology (ASCO) 2025 updates offer new insights into treating BRAF V600E-mutated metastatic colorectal cancer. They highlight the role of molecular profiling and BRAF-targeted therapy combinations in treatment.
Key takeaways from the ASCO 2025 updates include:
- Recommendations for BRAF testing in all patients with metastatic colorectal cancer
- Guidelines for the use of Encorafenib plus Cetuximab in the first-line setting
- Emerging data on novel combination regimens
As we learn more about metastatic colorectal cancer and its treatment, BRAF-targeted therapy combinations are key. Following the latest clinical guidelines, like those from ASCO, helps ensure patients get the best and most personalized care.
Immunotherapy for dMMR/MSI-H Metastatic Colorectal Cancer
Immunotherapy brings new hope to those with dMMR/MSI-H metastatic colorectal cancer. It uses the body’s immune system to fight cancer. This has changed how we treat this disease.
Checkpoint Inhibitors
Checkpoint inhibitors, like pembrolizumab, are very effective against dMMR/MSI-H metastatic colorectal cancer. They help the immune system attack cancer cells better.
These drugs are now used in different stages of treatment. This gives patients more options and better chances of recovery. Treatment guidelines are updated regularly to reflect new research.
Combination Approaches
We’re looking into combining immunotherapy with other treatments. This includes chemotherapy or targeted therapy. The goal is to make treatments more effective and longer-lasting for patients with dMMR/MSI-H metastatic colorectal cancer.
Studies are ongoing to find the best combinations. They help us understand which treatments work best for patients.
Patient Selection and Response Rates
Choosing the right patients for immunotherapy is key. Biomarkers like MSI-H/dMMR status help identify those who will benefit most.
Not all patients respond the same way to immunotherapy. But, many with dMMR/MSI-H tumors see long-lasting benefits. Below is a summary of some recent studies.
| Treatment | Response Rate | Median PFS |
| Pembrolizumab | 35% | 8.2 months |
| Nivolumab + Ipilimumab | 55% | 11.6 months |
| Pembrolizumab + Chemotherapy | 45% | 10.5 months |
As research keeps improving, we expect even better treatments for metastatic colorectal cancer. Immunotherapy is a big step forward in fighting this disease.
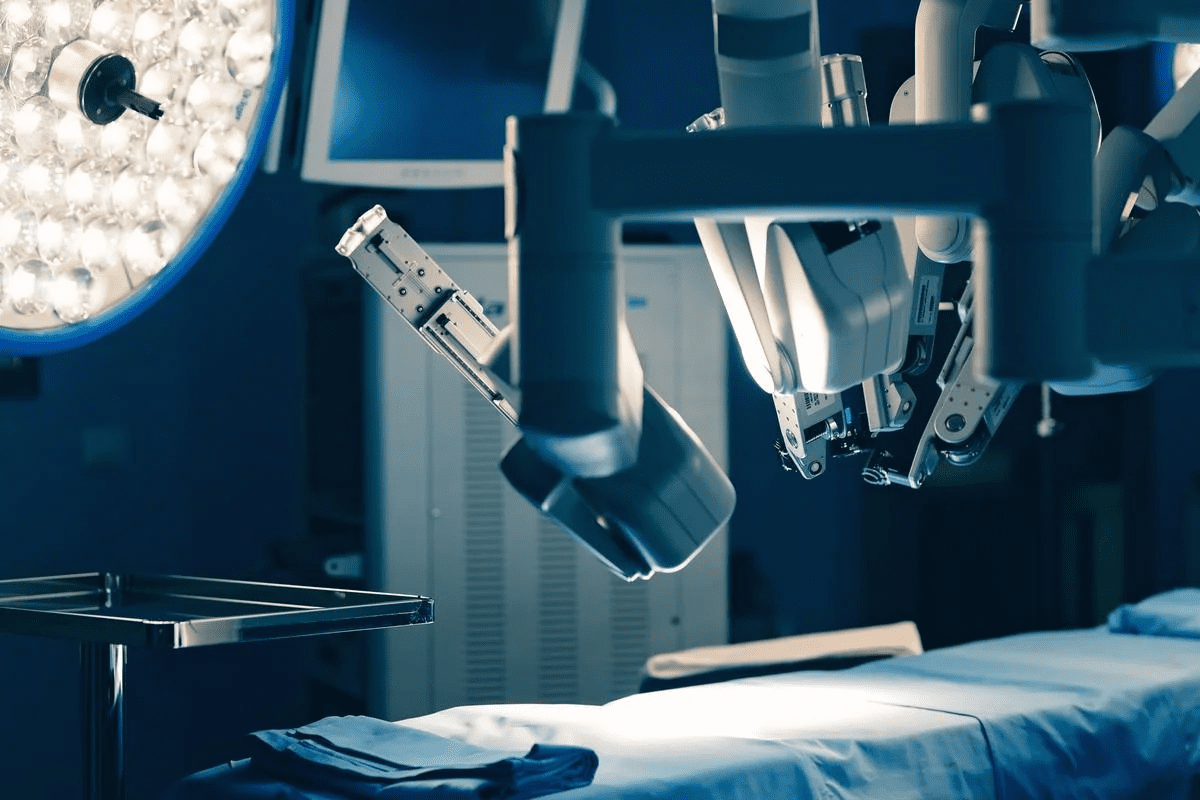
Surgical Management of Metastatic Disease
Surgery plays a key role in treating metastatic colorectal cancer. It’s a vital part of care for some patients. Advances in treatment have made surgery more important for certain patients.
Resection of Liver Metastases
Liver metastases are common in colorectal cancer. Surgery to remove these can be a cure for some. Studies show that selected patients can live long-term or even be cured.
Choosing to do surgery depends on several factors. These include the number and location of metastases, extrahepatic disease, and the patient’s health. Advances in surgery and treatments have helped more patients benefit from liver resection.
Multidisciplinary evaluation is key in finding the right candidates for surgery.
Lung and Other Distant Metastases
Surgery for lung and other distant metastases is also considered for some. The approach is similar to liver metastases, focusing on removing all disease while saving normal tissue.
Other distant metastases, like peritoneal or ovarian, may also be treated surgically. The decision is made based on disease extent and patient health.
Timing of Surgery in the Treatment Sequence
The timing of surgery varies based on several factors. In some cases, surgery is done first, like when the primary tumor is symptomatic or metastases are limited.
In other cases, surgery comes after systemic therapy. This is to see how the treatment worked or to make disease resectable. It’s important for medical and surgical oncology to work together to decide the best timing and sequence of treatments.
Interventional Radiology Techniques
Interventional radiology is key in fighting metastatic colorectal cancer. It brings new, less invasive ways to treat the disease. We’ll look at three main techniques: radiofrequency ablation, transarterial chemoembolization, and radioembolization.
Radiofrequency Ablation
Radiofrequency ablation (RFA) uses heat to kill cancer cells. A thin probe is inserted into the tumor under imaging. It sends electrical currents that heat up the area, killing the cancer.
RFA is good because it’s less invasive and has quick recovery times. It works best for smaller tumors.
Transarterial Chemoembolization
Transarterial chemoembolization (TACE) delivers chemotherapy directly to the tumor. It blocks the tumor’s blood supply. This is done by injecting drugs into the tumor’s artery and then blocking it.
TACE is very effective for liver metastases. It delivers high doses of chemotherapy right to the tumor, reducing side effects.
Radioembolization (Y-90)
Radioembolization, or Y-90 therapy, uses tiny radioactive beads. These beads are injected into the tumor’s arteries. They release radiation directly to the tumor, protecting healthy tissue.
This method is great for treating liver metastases. It has been shown to improve survival rates for some patients.
| Treatment | Primary Use | Benefits |
| Radiofrequency Ablation | Small tumors, mostly in liver or lung | Minimally invasive, quick recovery |
| Transarterial Chemoembolization | Liver metastases | High local chemotherapy dose, reduced systemic side effects |
| Radioembolization (Y-90) | Liver metastases | Direct radiation to tumor, spares healthy tissue |
Interventional radiology has greatly improved metastatic colorectal cancer treatment. These methods offer targeted, less invasive treatments. They improve patient outcomes and quality of life. As research goes on, we’ll see even better treatments.
Supportive Care Strategies
Supportive care is key to improving life quality for those with metastatic colorectal cancer. As we tackle the challenges of metastatic CRC treatment, we must meet patients’ diverse needs.
Pain Management
Managing pain is vital for those with management of metastatic colorectal cancer. We use medicines and other methods to keep patients comfortable. This is important for their treatment journey.
Nutritional Support
Nutrition is also critical for patients’ health and treatment tolerance. We help patients create nutrition plans that fit their needs.
Psychosocial Care
Psychosocial care helps with emotional and mental challenges for patients and their families. Our team offers counseling and support groups to help them cope.
| Supportive Care Strategy | Description | Benefits |
| Pain Management | Pharmacological and alternative therapies | Improved comfort, reduced distress |
| Nutritional Support | Personalized nutrition planning | Enhanced health, better treatment tolerance |
| Psychosocial Care | Counseling, support groups | Emotional support, coping strategies |
By using these supportive care strategies, we can greatly enhance life quality for metastatic colorectal cancer patients. Our all-encompassing care ensures patients get the support they need at every step.
Conclusion: The Future of Metastatic Colorectal Cancer Treatment
The treatment for metastatic colorectal cancer (mCRC) is changing fast, bringing new hope to patients. New discoveries in molecular profiling, targeted therapies, and immunotherapy have opened up more treatment options.
Research keeps going, helping us understand mCRC better. This leads to new treatments. The latest guidelines for treating mCRC include these new findings and strategies.
We’re looking forward to even better treatments and care for mCRC patients. The focus will be on treatments tailored to each patient and team care.
The outlook for mCRC treatment is bright, thanks to ongoing research and a dedication to better care. Healthcare providers can offer the best care by keeping up with these advances.
FAQ
What is metastatic colorectal cancer?
Metastatic colorectal cancer starts in the colon or rectum. It then spreads to other parts of the body. This can include the liver, lungs, or lymph nodes.
What are the treatment options for metastatic colorectal cancer?
Treatments include chemotherapy, targeted therapies, and immunotherapy. Surgery and interventional radiology are also options. Supportive care helps manage symptoms and side effects.
What is molecular profiling, and how does it guide treatment decisions?
Molecular profiling tests the tumor for genetic mutations. This helps choose the right treatment. It’s based on the tumor’s molecular profile.
What is the role of chemotherapy in treating metastatic colorectal cancer?
Chemotherapy kills cancer cells. It’s often used with other treatments. This helps fight metastatic colorectal cancer.
What are anti-EGFR targeted therapies, and how are they used?
Anti-EGFR therapies target the EGFR protein. They’re used for patients with RAS wild-type tumors. Medications like cetuximab and panitumumab are examples.
What is the role of immunotherapy in treating metastatic colorectal cancer?
Immunotherapy boosts the immune system to fight cancer. It’s used for patients with dMMR/MSI-H tumors. Checkpoint inhibitors are a type of immunotherapy.
Can surgery be used to treat metastatic colorectal cancer?
Yes, surgery can be used in some cases. It’s for cancer in the liver or lungs. The goal is to remove the cancerous tumors.
What is interventional radiology, and how is it used?
Interventional radiology uses minimally invasive procedures. It’s for treating cancer in specific situations. Examples include radiofrequency ablation and transarterial chemoembolization.
What is supportive care, and why is it important?
Supportive care manages symptoms and side effects. It improves quality of life. It’s a key part of treating metastatic colorectal cancer.
What are the latest advancements in metastatic colorectal cancer treatment?
New treatments include targeted therapies and immunotherapies. Combination regimens are also being explored. Research aims to improve treatment outcomes and quality of life.
How is metastatic colorectal cancer staged?
It’s staged using the TNM system. This considers the tumor size, lymph node involvement, and distant metastases.
What is the prevalence of metastatic colorectal cancer?
It’s a significant health issue worldwide. It affects many people, with a high prevalence in certain groups.
How is the management of metastatic colorectal cancer guided by treatment guidelines?
Guidelines, like those from the NCCN, offer evidence-based recommendations. They cover chemotherapy, targeted therapies, and other treatments.
What is the role of BRAF-targeted therapy combinations in treating metastatic colorectal cancer?
BRAF-targeted therapy combinations, like encorafenib plus cetuximab, treat patients with BRAF V600E mutations. They’re used for metastatic colorectal cancer.
What are the benefits of a multidisciplinary team approach in treating metastatic colorectal cancer?
A team approach ensures complete and coordinated care. It involves healthcare professionals from various specialties. It’s essential for treating metastatic colorectal cancer.
References:
Pietrangelo, A. (2024). Managing weight loss after gallbladder removal. Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/317659