Last Updated on December 2, 2025 by Bilal Hasdemir

Did you know that herniated discs affect millions of people worldwide? They cause a lot of pain and discomfort. For many, spinal surgery is the only way to find relief. Microdiscectomy, a minimally invasive surgery, is often suggested for herniated discs.
We will look into what microdiscectomy is and if it involves replacing the disc. This surgery removes the herniated part that presses on the nerve. It helps the patient feel better. Knowing about the disc removal process is key for those thinking about this microdiscectomy procedure.
Learn what the microdiscectomy procedure entails. Understand that the goal is to remove the herniated part, not replace the entire disc clearly.
Key Takeaways
- Microdiscectomy is a surgical treatment for herniated discs.
- The procedure involves removing the herniated disc fragment.
- It is a minimally invasive spinal surgery method.
- Understanding the surgery helps in making informed decisions.
- The goal is to relieve pressure on the nerve.
Understanding Herniated Discs and Spinal Anatomy
It’s important to know about spinal anatomy to understand herniated discs and their effects on our health. The spine is made up of vertebrae, discs, and nerves. These parts work together to support and move our body.
Structure of the Spinal Disc
A spinal disc is a soft, gel-filled cushion between vertebrae. It has two parts: the nucleus pulposus (soft inner gel) and the annulus fibrosus (tough outer layer). This disc helps absorb shock, allowing for spine flexibility and movement.
- The nucleus pulposus provides cushioning and support.
- The annulus fibrosus contains the nucleus and provides structural integrity.
How Disc Herniation Occurs
A herniated disc happens when the annulus fibrosus tears. This lets the nucleus pulposus push through and possibly compress nerves. This can be due to wear and tear, injury, or sudden strain on the spine.
“A herniated disc occurs when the disc’s soft inner gel pushes through a tear in the outer disc, potentially compressing nearby nerves.” – A’dan Z’ye Sağlık
Impact on Surrounding Nerves
When a disc herniates, it can press on nearby nerves. This can cause pain, numbness, and weakness in the affected area. The lumbar spine is often affected because it carries a lot of our body’s weight and stress.
- Pain and discomfort due to nerve compression.
- Numbness or tingling sensations in the limbs.
- Muscle weakness resulting from nerve impairment.
The Microdiscectomy Procedure
The microdiscectomy procedure is a minimally invasive surgery. It helps relieve pressure on nerves from herniated discs. This method is key in spinal surgery, providing a precise and effective solution for disc-related issues.
Definition and Purpose
Microdiscectomy is a surgery that removes herniated disc material pressing on a spinal nerve. Its main goal is to ease pain, numbness, and weakness from nerve compression.
Key aspects of microdiscectomy include:
- Minimally invasive approach, reducing tissue damage
- Use of an operating microscope for enhanced visualization
- Precise removal of herniated disc material
- Relief from nerve compression symptoms
History and Development
The microdiscectomy’s development comes from advances in neurosurgery and orthopedic surgery. Spinal surgeries were once more invasive and risky. But, with microsurgical techniques, surgeons now perform procedures with more precision and less tissue disruption.
| Evolution Stage | Description | Impact |
| Early Techniques | More invasive, larger incisions | Higher risk of complications |
| Introduction of Microscopy | Use of operating microscope | Improved visualization, less tissue damage |
| Modern Microdiscectomy | Minimally invasive, precise | Faster recovery, reduced risk |
When This Surgery is Recommended
Microdiscectomy is recommended for those who haven’t improved with conservative treatments. This includes physical therapy, medication, or injections. The decision to have surgery depends on the severity of symptoms and how they affect the patient’s life.
Indications for microdiscectomy include:
- Severe pain or numbness that persists despite conservative treatment
- Significant weakness or motor deficits
- Cauda equina syndrome, a condition requiring emergency surgery
- Large disc herniations causing significant nerve compression
The Truth About Disc Removal in Microdiscectomy
Understanding what happens to the disc during microdiscectomy can clear up many misconceptions. Microdiscectomy is a precise surgery for herniated discs causing pain or neurological symptoms.
Partial vs. Complete Disc Removal
Many patients worry if the whole disc is removed in microdiscectomy. The answer is usually no. Only the herniated portion of the disc is removed, which is pressing on the nerve roots.
Microdiscectomy removes only the herniated part of the disc, not the whole thing. This is called partial disc removal or discectomy. The goal is to ease nerve root pressure while keeping as much of the disc as possible.
What Actually Gets Removed
In a microdiscectomy, the surgeon takes out the herniated disc part that’s pressing on nerves. This might mean removing a disc fragment that’s gone beyond its normal space or just cleaning out the herniated material inside the disc.
| Component | Description | Action During Microdiscectomy |
| Herniated Disc Material | The portion of the disc that has bulged or ruptured. | Removed to relieve pressure on nerves. |
| Disc Space | The area between the vertebrae where the disc resides. | Partially cleaned or preserved. |
| Nerve Roots | Nerves that exit the spinal canal. | Decompressed by removing herniated material. |
Preserving Disc Function
Removing only the herniated part aims to keep the rest of the disc intact. This helps avoid long-term spinal instability and improves patient outcomes.
Microdiscectomy’s spinal decompression can greatly reduce symptoms by easing nerve root pressure. This careful method helps keep disc function and lowers the chance of complications.
Common Misconceptions About Microdiscectomy
Microdiscectomy is often misunderstood, which can stop people from getting this surgery. We meet patients who worry because they’ve heard wrong things about it. We need to clear up these myths and give the right info to help patients choose wisely.
Myth: The Entire Disc is Removed
Many think microdiscectomy means taking out the whole disc. But, it’s actually about removing just the herniated part that’s bothering the nerve. This way, the rest of the disc stays intact, keeping the spine stable.
“The key to a successful microdiscectomy is precision,” says a leading spine surgeon. “By removing only the problematic part of the disc, we minimize the impact on the surrounding spinal anatomy.” This method cuts down on recovery time and keeps the spine working right.
Myth: Microdiscectomy Always Requires Fusion
Some believe microdiscectomy always means spinal fusion. But, most of the time, it’s done alone without fusion. Fusion is usually needed only if there’s spinal instability or other issues.
- Microdiscectomy is generally not accompanied by fusion unless there’s significant spinal instability.
- The procedure is designed to be as minimally invasive as possible, reducing the need for more extensive surgeries like fusion.
- By preserving the disc and surrounding structures, microdiscectomy maintains the natural integrity of the spine.
Myth: Recovery is Extremely Lengthy
Many think recovery from microdiscectomy takes a long time. But, most people can get back to normal in just a few weeks. The minimally invasive nature of microdiscectomy helps it heal faster than bigger surgeries.
As we learn more, recovery from microdiscectomy gets easier. Patients can usually handle their pain well and get back to their daily life quickly.
We aim to clear up these myths so people understand what microdiscectomy is and what to expect. Our goal is to make sure patients are well-informed and ready for their journey to back pain relief.
Lumbar Microdiscectomy: The Most Common Type
Microdiscectomy is often used in the lumbar spine because it bears a lot of weight. The lumbar area, with five vertebrae (L1-L5), is prone to disc problems. This is due to its weight-bearing role and the stress it faces.
Anatomy of the Lumbar Spine
The lumbar spine has a unique shape and strong bones to carry our weight. The discs between the vertebrae help absorb shock and keep the spine flexible. The anatomy of the lumbar spine makes it more likely to have disc herniations, mainly at L4-L5 and L5-S1.
Why Lumbar Herniations Are Common
Lumbar herniations happen often because of the spine’s role in supporting our body. Heavy lifting, bending, or twisting can increase the risk of disc problems. Both degenerative changes and injuries can cause lumbar disc herniations, making surgery like lumbar microdiscectomy necessary.
Specific Techniques for Lumbar Procedures
Lumbar microdiscectomy uses special microsurgical methods to reduce damage and speed up healing. Surgeons use advanced tools for clear views of the disc and nerves. These precise techniques help remove herniated disc material without harming the spinal structures.
Understanding the lumbar spine’s anatomy and issues helps surgeons tailor treatments. This approach improves results in lumbar microdiscectomy for each patient.
Step-by-Step Breakdown of the Microdiscectomy Procedure
The success of a microdiscectomy depends on careful preparation and precise surgery. We will explain the key steps to help you understand the procedure fully.
Preoperative Preparation
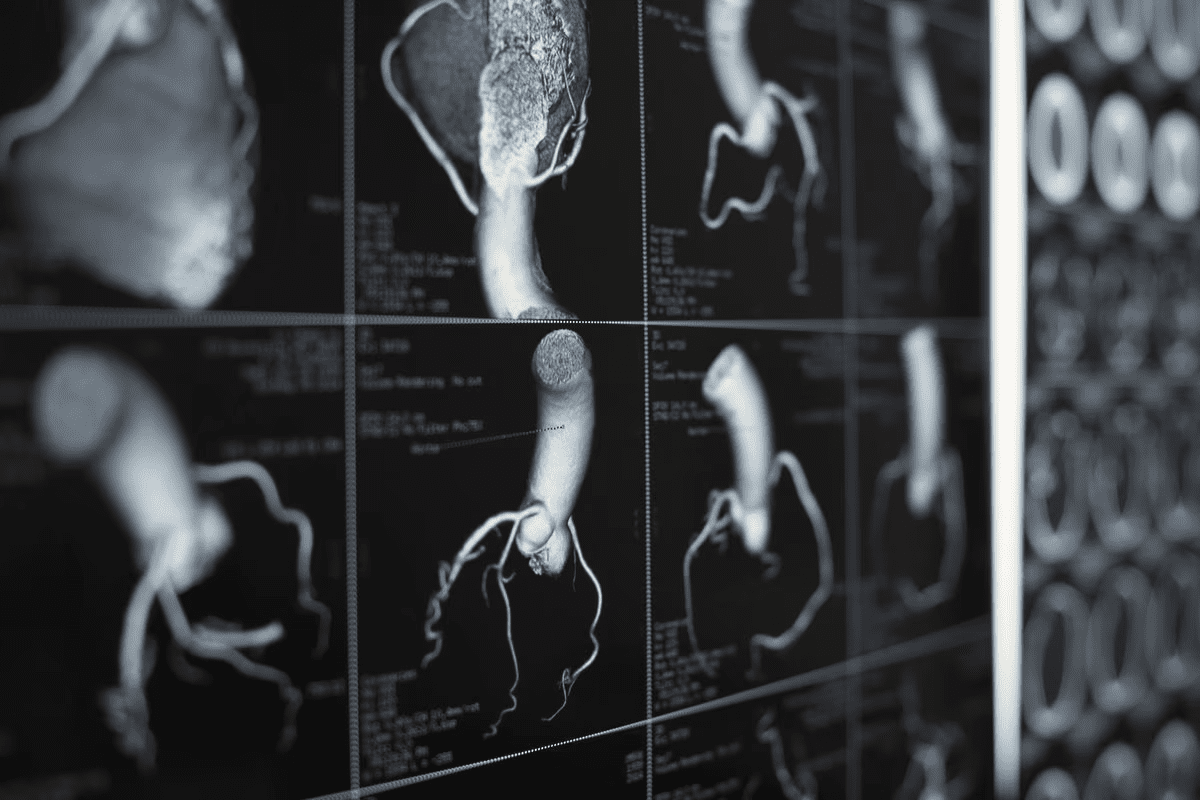
Before surgery, several steps are taken to prepare the patient. Preoperative preparation includes a detailed medical check-up and imaging tests like MRI or CT scans. Patients also discuss the risks and benefits of the surgery.
They are advised on how to prepare, including any changes to their medication. We review the patient’s medical history to identify any risks or complications. This includes checking for allergies, previous surgeries, or conditions that could affect the surgery or recovery.
Anesthesia and Positioning
On the day of the surgery, the patient gets general anesthesia or local anesthesia with sedation. The choice of anesthesia ensures the patient’s comfort during the procedure.
Once the anesthesia takes effect, the patient is positioned on the operating table. They lie on their stomach or side, depending on the disc’s location.
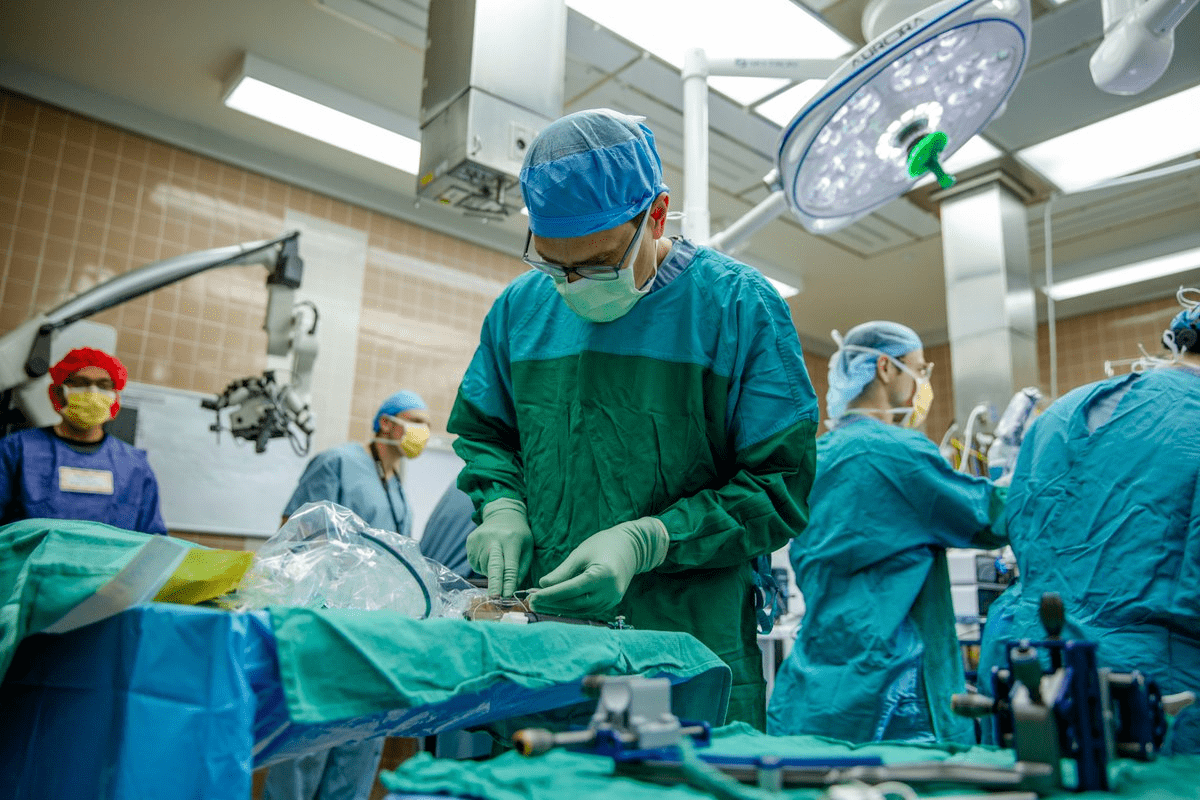
Surgical Technique
The procedure involves a small incision in the back, about 1-2 inches long. We use a microscope or endoscope to see the disc and nerves. This allows us to remove the herniated disc material precisely.
| Step | Description |
| 1. Incision | A small incision is made to access the spine. |
| 2. Visualization | A microscope or endoscope is used to visualize the disc and nerves. |
| 3. Discectomy | The herniated disc material is carefully removed. |
| 4. Closure | The incision is closed with sutures or staples. |
Throughout the procedure, we aim to minimize disruption to surrounding tissues and nerves. This helps in a smoother recovery for the patient.
Advanced Techniques in Modern Microdiscectomy
Medical technology has changed microdiscectomy for the better. Now, patients have more effective treatments. Spine surgery has seen big improvements, thanks to new techniques that make surgery more precise and quick.
Microscope-Assisted Surgery
Microscope-assisted surgery is a big step forward in microdiscectomy. It uses a surgical microscope for high magnification and illumination. This lets surgeons remove herniated disc material more accurately, keeping nearby tissue safe.
This method helps see the surgical area better. It lowers the chance of problems and makes patients do better.
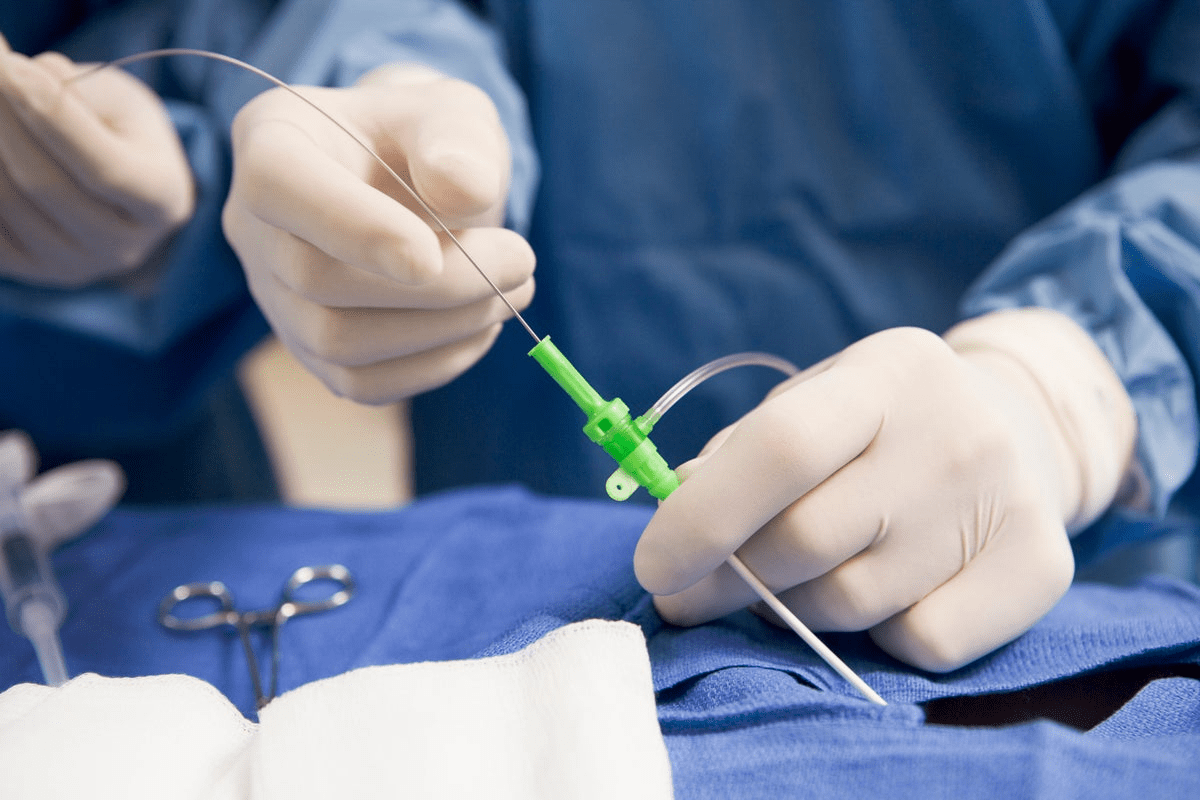
Endoscopic Approaches
Endoscopic methods are getting more popular in microdiscectomy. These minimally invasive procedures use an endoscope to see the disc herniation and nerves. They need smaller cuts, cause less damage, and help patients recover faster than old surgery methods.
Endoscopic microdiscectomy works well for patients with small disc herniations.
Tubular Retractor Systems
Tubular retractor systems are also used in modern microdiscectomy. They use a small corridor to the disc herniation, causing less damage. This method leads to less pain after surgery and quicker recovery times.
It’s very good for treating lumbar disc herniations.
In summary, new techniques like microscope-assisted surgery, endoscopic approaches, and tubular retractor systems have greatly improved microdiscectomy. These advancements have made patients’ outcomes better, recovery times shorter, and complications fewer. This marks a new chapter in spine surgery.
Potential Risks and Complications
Knowing the risks of microdiscectomy is key for making smart choices. This surgery is usually safe and works well. But, like any surgery, it comes with some risks.
Surgical Risks
Microdiscectomy can lead to nerve damage, bleeding, and infection. These are rare but can greatly affect recovery and health.
Nerve Damage: Nerve damage is a worry because nerves are close to the surgery area. It can cause numbness, weakness, or pain.
Recurrent Herniation
Recurrent herniation is a possible complication. It happens when the disc bulges again after surgery. The risk depends on how much disc is removed and the patient’s health.
| Risk Factor | Description | Impact on Recurrent Herniation |
| Amount of Disc Removed | The extent of disc removal during surgery. | Higher removal may increase risk. |
| Patient Age | The age of the patient at the time of surgery. | Younger patients may have higher risk. |
| Pre-existing Conditions | Presence of other spinal conditions or diseases. | Can complicate surgery and recovery. |
Spinal Instability Concerns
Spinal instability is a risk, mainly if a lot of the disc is taken out. This can cause vertebrae to move abnormally.
Infection and Other Complications
Infection is a risk with any surgery, including microdiscectomy. Other possible problems include bleeding, reactions to anesthesia, and unexpected issues.
It’s important for patients to talk to their doctor about these risks. This way, they can understand how they might be affected personally.
The Patient Experience: What to Expect
Thinking about surgery can be scary. That’s why we’re here to guide you through your microdiscectomy journey.
Before Surgery: Preparation and Testing
Before your surgery, you’ll go through tests and preparations. This makes sure you’re ready for the procedure. You’ll likely have:
- Medical Clearance: Your doctor will check your medical history and do a physical exam.
- Imaging Tests: You might need MRI or CT scans to confirm the diagnosis and plan the surgery.
- Blood Tests: These tests check for any conditions that could affect the surgery.
- Medication Adjustment: Your doctor might tell you to stop or change some medications before surgery.
| Preparation Step | Purpose |
| Medical Clearance | To ensure you’re fit for surgery |
| Imaging Tests | To confirm diagnosis and plan surgery |
| Blood Tests | To check for underlying conditions |
Day of Surgery Experience
On surgery day, you’ll arrive at the hospital or surgical center. Our staff will welcome you. Then, you’ll go to the operating room for preparation.
It’s normal to feel a mix of emotions, but rest assured that our team is experienced in making the process as smooth as possible.
Immediate Post-Operative Sensations
After surgery, you’ll go to the recovery room. There, you’ll be watched as you wake up from anesthesia. You might feel some discomfort, numbness, or tingling, but these feelings are usually short-lived.
Our team will help you through the immediate post-operative care. They’ll make sure you’re comfortable and answer any questions you have.
Recovery Timeline After Microdiscectomy
Recovering from a microdiscectomy involves several stages. Each stage has its own timeline and things to consider. Knowing these stages helps patients get ready for their recovery journey.
Hospital Stay Duration
Most people have microdiscectomy as an outpatient procedure. This means they can go home the same day. But, some might need to stay in the hospital for a short time. This is usually if there are concerns about their health or if the procedure was more complex. Generally, the hospital stay is less than 24 hours.
First Few Weeks at Home
The first few weeks at home are very important. Patients should rest and avoid heavy lifting, bending, or hard activities. Post-operative care during this time is key for a smooth recovery. It’s important to follow the healthcare team’s specific instructions. This might include managing pain, taking care of the wound, and slowly increasing physical activity.
In the first few weeks, some patients might feel discomfort, numbness, or weakness. These feelings are usually temporary. It’s important to watch these symptoms and talk to their healthcare provider if they get worse.
Long-Term Recovery Expectations
The time it takes to fully recover from microdiscectomy can vary. But most people see big improvements in 4 to 6 weeks. It might take a few months to get back to normal activities and sports. Maintaining a healthy spine is key for long-term spine health. This includes keeping good posture, exercising regularly, and eating a balanced diet.
We tell patients to be patient and not rush their recovery. It’s important to follow the post-operative instructions and go to all follow-up appointments. This helps ensure the best recovery outcome.
Physical Therapy and Rehabilitation
Rehabilitation is key for patients to get back their strength and mobility after microdiscectomy surgery. A good rehabilitation plan is vital for the best recovery.
Importance of Rehabilitation
Rehab after microdiscectomy is more than just healing from surgery. It’s about getting strong and flexible for everyday tasks. Physical therapy is customized for each person. It includes exercises that help with healing, posture, and spine health.
Through rehab, patients can see less pain and swelling, better movement, and get back to their usual life faster. We stress the need for a structured rehab plan for the best results.
Recommended Exercises
Physical therapists suggest different exercises for recovery. These might include:
- Gentle stretching to boost flexibility
- Strengthening exercises for the back and core
- Low-impact aerobic activities like walking or swimming to keep overall health without harming the spine
These exercises are made to get more challenging as the patient gets better. This ensures a safe and effective healing process.
Gradual Return to Activities
Going back to normal activities slowly is a big part of rehab. We tell patients to avoid heavy lifting, bending, or twisting at first. As they heal, they can start doing more, like going back to work or hobbies.
It’s important to listen to healthcare experts on when to start doing certain things again. This makes sure the spine is fully healed and strong.
When Disc Replacement Might Be Necessary
Total disc replacement is for people with certain disc problems. It replaces the damaged disc with an artificial one. This aims to fix spinal function and ease pain.
Indications for Total Disc Replacement
Doctors suggest total disc replacement for certain cases. These include:
- Significant disc degeneration shown by imaging
- Chronic back pain not helped by other treatments
- Specific disc herniation or degeneration suitable for replacement
Total disc replacement is an option for those with severe disc degeneration. It’s a choice instead of fusion surgery.The goal is to keep spinal mobility while fixing the pain source.
Artificial Disc Options
There are many artificial discs, each with its own design and materials. Some common ones are:
| Artificial Disc | Material | Key Features |
| Charité Artificial Disc | Metal-on-polyethylene | Modular design, allows for variable lordosis |
| ProDisc-L | Metal-on-polyethylene | Constrained design, promotes spinal stability |
Comparing Outcomes with Microdiscectomy
Comparing total disc replacement with microdiscectomy, several factors are important. Microdiscectomy removes the herniated part of the disc. Total disc replacement replaces the whole disc. Both can help with pain, but they work differently.
A study in the Journal of Neurosurgery: Spine showed total disc replacement can be as good or better than microdiscectomy for some patients. But, the best choice depends on the patient’s specific situation.
In summary, total disc replacement is a big surgery for certain disc problems. Knowing the reasons, artificial disc choices, and how it compares to microdiscectomy helps patients and doctors make the right choice.
Non-Surgical Alternatives to Consider
Before surgery, think about non-surgical treatments for herniated discs. Many find relief with conservative management or minimally invasive procedures. This might mean avoiding surgery altogether.
Conservative Treatment Options
Conservative treatment is often the first step for herniated disc symptoms. It includes physical therapy, pain management, and lifestyle changes. Physical therapy is key, strengthening muscles and improving flexibility. It also helps reduce pain.
Patients learn proper lifting techniques and posture correction to avoid back strain. Pain management is also vital. This might include pain relievers, muscle relaxants, or epidural steroid injections to reduce inflammation and pain.
Lifestyle changes, like maintaining a healthy weight and quitting smoking, are also important. Regular exercise can help manage symptoms.
Minimally Invasive Non-Surgical Procedures
For those not helped by conservative care, minimally invasive procedures are an option. These aim to reduce pain and inflammation with minimal body disruption.
Epidural steroid injection (ESI) is one such procedure. It involves injecting corticosteroids into the epidural space. This can reduce inflammation and relieve pain. Another option is nerve ablation, which uses heat or radiofrequency to disrupt pain signals.
When to Choose Surgery vs. Conservative Care
The choice between surgery and conservative care depends on several factors. These include symptom severity, daily life impact, and overall health. If conservative treatments don’t work, or if there’s significant nerve damage, surgery might be needed.
It’s important for patients to discuss their options with their healthcare provider. The decision will depend on the herniation size and location, patient preferences, and lifestyle.
Success Rates and Outcome Statistics
Many studies have looked into how well microdiscectomy works. It’s a common surgery for herniated discs in the lower back.
Pain Relief Outcomes
Research shows that microdiscectomy helps a lot with pain from herniated discs. Most patients see a big improvement in their symptoms after the surgery. A study in the Journal of Neurosurgery: Spine found that patients felt less pain and could move better.
The surgery removes the part of the disc that’s pressing on nerves. This stops the pain. Both surgery and other treatments are key to managing pain well.
Functional Improvement Metrics
Microdiscectomy also helps patients do more things and go back to work. Studies show that patients can do more daily tasks and work again. Most patients get better in a few weeks to months.
Rehab and physical therapy are important for getting better. They help patients get stronger and healthier again.
Factors Affecting Success
Many things can affect how well microdiscectomy works. Choosing the right patients and using the best techniques matter a lot. New surgical methods and tools also make the surgery better.
How well patients recover also depends on after-care. Following doctor’s orders and doing physical therapy is key for a good recovery.
Conclusion
Microdiscectomy is a key treatment for herniated discs. It brings back pain relief and boosts spine health. This surgery helps fix the main cause of pain, making life better for those with spinal problems.
We’ve looked into microdiscectomy’s details. From its start to today’s advanced methods, it’s a complex topic. Knowing how it works, like removing part of the disc, helps patients make informed choices.
Microdiscectomy isn’t for everyone. It’s a serious step that should be thoughtfully considered. Patients need to weigh their situation, like how bad the herniation is and their health. The right choice can lead to better health and a return to daily life.
FAQ
What is microdiscectomy, and does it involve disc replacement?
Microdiscectomy is a surgery to treat herniated discs. It removes the damaged part of the disc. This doesn’t mean replacing the whole disc. It aims to ease pressure on nerves by taking out the bad part.
What happens to the disc during a microdiscectomy procedure?
Only the bad part of the disc is taken out during microdiscectomy. This keeps the good part of the disc and helps keep the spine stable.
Is microdiscectomy a major surgery?
Microdiscectomy is a less invasive surgery. It’s smaller than open spine surgery. This means less damage and quicker healing times.
What are the benefits of choosing microdiscectomy over other treatments for herniated discs?
Microdiscectomy offers many benefits. It can relieve symptoms like sciatica and back pain. It’s less invasive and has quicker recovery times than other surgeries.
How long does it take to recover from a microdiscectomy?
Recovery times vary, but most people can get back to normal in a few weeks. The first few weeks are for rest and then you can start getting back to your activities slowly, with help from physical therapy.
Are there any risks or complications associated with microdiscectomy?
Like any surgery, microdiscectomy has risks. These include infection, bleeding, nerve damage, and herniation coming back. But serious problems are rare. It’s safe when done by skilled surgeons.
Can microdiscectomy be performed on any part of the spine?
Microdiscectomy is often done on the lower back. But it can also be used for the neck. The method used depends on where and how bad the herniation is.
What are the alternatives to microdiscectomy for treating herniated discs?
Other options include trying physical therapy, pain management, and changing your lifestyle. Or, you might choose other minimally invasive surgeries. The right choice depends on how bad your symptoms are and your overall health.
How successful is microdiscectomy in relieving symptoms?
Microdiscectomy works well for many people with herniated discs. It can help with pain, numbness, and weakness. But success can depend on how bad the herniation is and your overall health.
Will I need physical therapy after microdiscectomy?
Many people need physical therapy after microdiscectomy. It helps with recovery, improves strength, and makes it safer to get back to normal activities. How much physical therapy you need depends on your recovery and what your doctor says.
Reference
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa052259