Last Updated on October 31, 2025 by
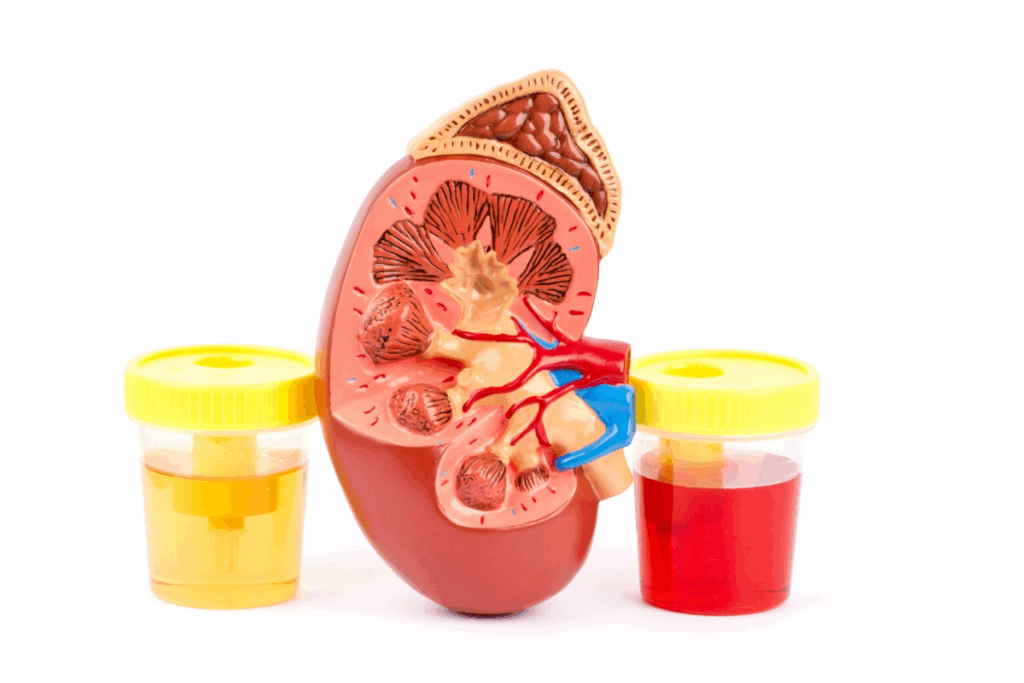
We often see hematuria, or red blood cells in the urine, in our work. It can be either visible to the eye or only seen through urinalysis.
About 4-5% of patients have microscopic hematuria. This means they have three or more red blood cells per high-power field on urinalysis. It can be without symptoms or linked to many causes, from harmless to serious diseases. Knowing the causes and how to check for them is key to the right diagnosis and treatment.
At LivHospital, we use the latest academic methods to find out if the hematuria is serious or not. Our goal is to make sure patients get the right care for their hematuria, helping doctors who are unsure.

Microscopic hematuria is when you have three or more red blood cells in your urine. It’s a common issue that can mean different things, from simple problems to serious diseases.
To find microscopic hematuria, doctors look at your urine under a microscope. They check for three or more red blood cells per field. This helps them decide if you need more tests.
The American Urological Association (AUA) says people with this issue should get checked out. They want to find out why it’s happening.
How common microscopic hematuria is can vary. It depends on who is being studied and how they are tested. In adults, about 2-4% have it when they get checked.
| Population Studied | Prevalence Range (%) |
| General Adult Population | 2-4 |
| Screening Populations | 0.2-21.1 |
Some people with microscopic hematuria don’t have any symptoms. Others might feel pain or have trouble urinating. The ones without symptoms are harder to diagnose because they might have serious health issues.
Doctors need to know if you have symptoms or not. This helps them figure out the best way to test and treat you.
People with symptoms might need to see a doctor right away. Those without symptoms might need more tests to find out why they have microscopic hematuria.
Risk stratification is key in managing microscopic hematuria. It helps find those at higher risk of cancer. Certain patient traits are important in determining risk.
Age is a big factor in risk assessment. People over 35 are at higher risk of cancer in the urinary tract. We recommend a more thorough investigation for patients in this age group.
Gender also affects risk assessment. Men are generally at a higher risk of urinary tract cancers than women. This is partly because bladder cancer is more common in men.
Smoking history is a big risk factor for urinary tract cancers. Quitting smoking is important, but past smoking affects risk. We take smoking history into account when evaluating the overall risk.
The difference between gross and microscopic hematuria is important. Gross hematuria, where blood is visible, is a higher risk for cancer. Patients with gross hematuria require immediate and thorough investigation.
To better understand risk stratification, let’s look at a table summarizing key risk factors:
| Risk Factor | High-Risk Characteristics | Implications |
| Age | Over 35 years | Increased risk of malignancy |
| Gender | Male | Higher incidence of bladder cancer |
| Smoking History | Past or current smoker | Increased risk of urinary tract malignancies |
| Type of Hematuria | Gross hematuria | Higher risk of malignancy, requires immediate investigation |
By understanding and applying these guidelines, we can better manage patients with microscopic hematuria. We can also identify those who need more diagnostic tests.
Urinary tract infections (UTIs) are common in women and the elderly. They often cause hematuria, which is blood in the urine. This usually leads to a doctor’s visit to find the cause.
Bacteria like Escherichia coli can cause UTIs. They invade the urinary tract, leading to inflammation and bleeding. This damage to the lining of the tract results in hematuria.
UTIs can happen anywhere in the urinary system. This includes the kidneys, bladder, or urethra. The severity and location of the infection can affect how much blood is in the urine.
People with UTIs may have symptoms like painful urination and frequent trips to the bathroom. They might also feel discomfort in the lower abdomen. The amount of blood in the urine can vary.
In older adults or those with weak immune systems, UTIs can be harder to spot. They might just feel generally unwell or confused.
Doctors use several methods to diagnose UTIs. These include a physical exam, urinalysis, and sometimes a urine culture. Urinalysis shows white blood cells and bacteria in the urine. It also checks for blood.
| Diagnostic Test | Typical Findings in UTIs |
| Urinalysis | Pyuria, bacteriuria, hematuria |
| Urine Culture | Positive for pathogenic bacteria (e.g., E. coli) |
| Imaging Studies | May be used to evaluate for complications or underlying conditions |
Treating UTIs involves antibiotics and supportive care. This includes staying hydrated and managing pain.
After treatment, it’s important to follow up. This ensures the infection is gone and checks for any ongoing issues. A repeat urinalysis can confirm the infection has cleared.
“The appropriate management of UTIs is not just treating the infection. It’s also about preventing complications and finding the cause of hematuria.”
— Clinical Guidelines on UTIs
Understanding UTIs helps us care for patients with hematuria. This includes diagnosing and treating the infection effectively.
Microscopic hematuria can signal urologic malignancies that need quick attention. Up to 5 percent of those with microscopic hematuria might have cancer in the urinary tract. This highlights the importance of a detailed diagnostic process.
Bladder cancer often shows up with painless blood in the urine. But it can also start with tiny amounts of blood. We suggest a full check-up for anyone with risk factors like smoking.
Seeing blood in the urine is the most common sign of bladder cancer. It means we need to do a thorough test. We use imaging and cystoscopy to find bladder cancer early.
Renal cell carcinoma can show up with blood in the urine, pain in the side, and a mass that can be felt. Not everyone will have all these symptoms. We should think about renal cell carcinoma for anyone with microscopic hematuria, even more so if they have risk factors.
| Symptom | Frequency |
| Hematuria | Common |
| Flank Pain | Less Common |
| Palpable Mass | Rare |
Prostate cancer can cause blood in the urine, often when there’s also prostatitis or blockage. We should think about prostate cancer in men with microscopic hematuria, even more so if they have other urinary issues.
Urothelial carcinoma, which includes cancers of the renal pelvis, ureters, and bladder, needs a detailed diagnostic process. We use imaging like CT urography and cystoscopy to find urothelial carcinoma.
It’s key to do a thorough test for urologic malignancies in patients with microscopic hematuria. Knowing how to spot and test for these cancers helps us improve patient care.
Urinary calculi, or kidney stones, are a big reason for hematuria, mainly in young men and those who’ve had stones before. These stones form when urine gets too full of salts and minerals. This makes the stones crystallize.
The making of urinary calculi is complex. Supersaturation of urine with salts like calcium oxalate is key. Other things like low urine volume, high urinary pH, and certain medications or dietary factors also play a part.
A top urology expert says, “Stone formation is about the balance of salts and inhibitors in urine.”
“Knowing how this works helps us prevent stones better.”
People with urinary calculi often have severe, colicky flank pain that goes to the groin. They also have hematuria. The pain is very bad and can make you feel sick, throw up, and need to pee a lot.
Imaging is key to finding urinary calculi. Non-contrast computed tomography (CT) is best because it finds stones well. Ultrasound and plain radiographs can also help, but they miss smaller stones.
How to manage urinary calculi depends on the stone’s size and where it is. Conservative management means drinking lots of water and taking pain meds. For bigger stones, surgical interventions like lithotripsy or percutaneous nephrolithotomy might be needed. To prevent stones, changing your diet and taking certain medications can help.
Understanding urinary calculi helps doctors treat symptoms and stop stones from coming back.
Glomerular disorders are a big part of why people get microscopic hematuria. They need a careful check-up. These issues show up as hematuria with odd-shaped red blood cells. They also bring protein in the urine and can hurt the kidneys.
IgA nephropathy, or Berger’s disease, is a common kidney problem. It often starts with hematuria after a cold. Doctors find it by looking at kidney tissue for IgA deposits.
Thin basement membrane disease is a mild condition. It causes ongoing hematuria and often runs in families. Doctors spot it by looking at the kidney’s basement membrane under an electron microscope.
Alport syndrome is a genetic disorder. It leads to hematuria, hearing loss, and kidney failure. Spotting it early is key to slowing its effects.
Doctors look for signs of glomerular bleeding, like odd-shaped red blood cells. They also check kidney function with blood tests. Sometimes, a kidney biopsy is needed to confirm the diagnosis.
| Condition | Key Features | Diagnostic Clues |
| IgA Nephropathy | Hematuria following infection, proteinuria | Renal biopsy showing IgA deposits |
| Thin Basement Membrane Disease | Persistent hematuria, family history | Thinning of the glomerular basement membrane on EM |
| Alport Syndrome | Hematuria, hearing loss, renal failure | Genetic mutations in type IV collagen genes |
Benign prostatic hyperplasia (BPH) and trauma are big reasons for microscopic hematuria. We need to look into how these issues cause hematuria. We will also talk about how to diagnose and manage them.
BPH is a common issue in older men where the prostate gland gets bigger. This can cause blood in the urine because of the swelling and inflammation.
The reasons behind BPH are complex. Hormonal changes, cell growth, and blood vessel issues all play a part. As the prostate grows, it can block urine flow, leading to more pressure and blood in the urine.
Urinary tract injuries can also cause blood in the urine. The amount of blood can vary based on the injury. People with these injuries might also feel pain or have trouble peeing.
We check patients who have had trauma for blood in their urine. This could mean they have a serious injury. We use imaging tests to see how bad the injury is.
Diagnosing BPH and hematuria starts with a detailed history and physical check-up. For BPH, we look at how bad the symptoms are and how big the prostate is.
For trauma-related hematuria, we use CT scans or ultrasounds to see the injury. Sometimes, we do a cystoscopy to look directly at the urinary tract.
For BPH-related hematuria, we treat the BPH itself. We use medicines to shrink the prostate and help with symptoms.
Managing trauma-related hematuria depends on the injury’s severity. For minor injuries, we just support the patient. But for more serious cases, surgery might be needed.
| Condition | Diagnostic Approach | Management Strategies |
| BPH | History, Physical Examination, Prostate Size Evaluation | Medical Therapy (Alpha-blockers, 5-alpha-reductase inhibitors) |
| Traumatic Hematuria | Imaging Studies (CT Scan, Ultrasound), Cystoscopy | Supportive Care, Surgical Intervention (if severe) |
When someone has microscopic hematuria, finding the cause is key. We’ll cover what steps healthcare providers take. This ensures they manage patients well.
First, doctors look at the patient’s history and do a physical check. They check for things like smoking, work exposures, and family health. The physical exam focuses on the urinary system.
Key elements of the patient history include:
Lab tests are important for checking microscopic hematuria. We suggest the following:
These tests help find possible causes and guide next steps.
“The American Urological Association guidelines recommend urinalysis and urine culture as initial steps in the evaluation of microscopic hematuria.”
Imaging is key to finding problems in the urinary tract. We suggest:
Cystoscopy is vital, mainly for high-risk patients or those with ongoing bleeding. It lets doctors see the bladder and urethra directly. This helps find tumors, stones, or other issues.
Cystoscopy is indicated in:
This procedure is key to finding problems not seen on images.
In summary, treating microscopic hematuria involves a detailed plan. This includes patient evaluation, lab tests, imaging, and cystoscopy when needed. This approach helps find the cause and manage it properly.
In about 50 percent of cases, doctors can’t find the cause of microscopic hematuria. We call this idiopathic microscopic hematuria. We keep an eye on these patients for any new symptoms or changes in their urine.
Even if no cause is found, it’s important to keep watching. Regular check-ups help catch any new problems early. This way, we make sure patients get the best care possible, even without a clear cause.
Being careful and proactive helps us reassure and support our patients. It also helps us catch any serious problems early. This shows how important it is to tailor care and follow up with each patient.
A: Microscopic hematuria is when you have red blood cells in your urine that you can only see with a microscope. It’s when you find three or more red blood cells per high-power field in your urine.
A: It can be caused by many things. These include urinary tract infections, cancer, kidney stones, and problems with the kidneys or prostate.
A: Doctors use several tests to find the cause. These include checking your urine, doing a urine culture, and using imaging like ultrasound and CT scans. They might also do a cystoscopy.
A: Risk stratification helps doctors figure out who might have a serious problem like cancer. They look at things like your age, if you smoke, and if you have blood in your urine.
A: Yes, it can happen without any symptoms. This makes it hard to catch early, as it might mean you have a serious problem with your kidneys or bladder.
A: UTIs can cause blood in your urine because of the infection and inflammation. Doctors treat it with antibiotics.
A: Cystoscopy is very important. It helps doctors check the inside of your bladder and ureters, which is key for finding problems like cancer in high-risk patients.
A: Doctors keep an eye on you for any changes or symptoms. They also check for cancer risk. This way, they can catch any new problems early.
A: Disorders like IgA nephropathy and Alport syndrome cause hematuria. It’s because of problems with the glomeruli or immune complexes.
A: The rate varies a lot. It can be as low as 0.2% or as high as 21.1%, depending on who is studied and how they are tested.
National Center for Biotechnology Information. (2025). 5 Causes of Microscopic Hematuria: A Clinical Workup. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534213/[5
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!