Last Updated on November 19, 2025 by Ilayda Cengizhan
Reaching the 100- days after stem cell transplant is a big deal. At this point, doctors check on several important things to see how well the patient is doing.
The Canadian Cancer Society says side effects usually show up right after the transplant. We help patients get through this important time with our detailed care plans.
Doctors look at survival rates, infection risk, and how well the immune system is recovering. Studies show that about 75-80% of adult patients make it to this point. But, how well they do can change a lot based on the type of stem cells used and how intense the treatment is.
Key Takeaways
- Survival rates are assessed at the 100-day mark after a stem cell transplant.
- Infection risk and immune recovery are critical factors evaluated during this period.
- Outcomes vary depending on stem cell source and conditioning intensity.
- Comprehensive care is essential for guiding patients through this pivot stage.
- About 75-80% of adult patients survive to the 100-day mark.
The Journey of Stem Cell Transplantation
Stem cell transplantation is a long journey with many steps. It starts with getting ready for the transplant and ends with care after it’s done. Knowing each step helps patients understand their recovery better.
Types of Stem Cell Transplants
There are two main types of stem cell transplants: autologous and allogeneic. Autologous stem cell transplants use the patient’s own stem cells. These cells are collected, stored, and then given back after treatment.
Allogeneic transplants use stem cells from another person. This can be a family member or someone else.
- Autologous transplants are often used for cancers like multiple myeloma or lymphoma.
- Allogeneic transplants are for genetic disorders or certain leukemias.
The Transplantation Process
The process starts with getting ready for the transplant. Then, stem cells are infused into the body. The first step is to get rid of the old bone marrow.
The Canadian Cancer Society notes that the type and dose of chemotherapy matter. A stronger chemotherapy might mean a longer recovery.
Pre-Transplant Conditioning Regimens
Getting ready for the transplant is key. This involves chemotherapy and/or radiation to weaken the immune system. It also kills any cancer cells.
- Chemotherapy kills cancer cells and gets the bone marrow ready for new stem cells.
- In some cases, radiation is used to weaken the immune system further.
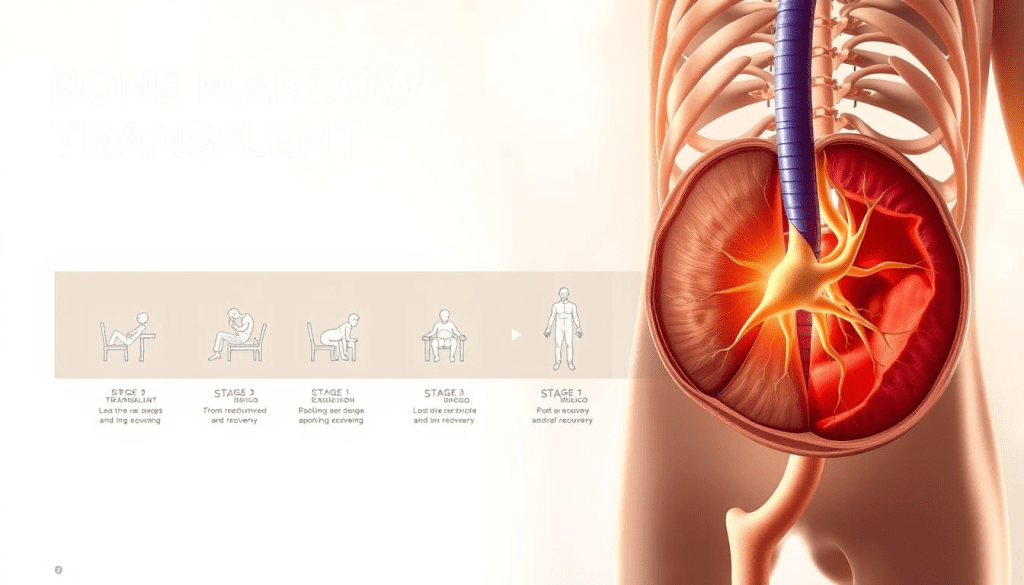
Bone Marrow Transplant Timeline Overview
Knowing the bone marrow transplant timeline is key to patient care. The process has many stages, each with its own challenges. It’s important to understand the recovery journey patients will take.
The timeline is very important during the intermediate recovery phase, from days 30 to 100 after the transplant. At this time, patients are watched closely for signs of engraftment, GVHD, and other issues.
Intermediate Recovery Phase (Days 30-100)
The intermediate recovery phase is a critical time in the bone marrow transplant timeline. Anthony Nolan says the focus is now on patient experience, not just timelines. This change recognizes that every patient’s recovery is different.
In days 30-100, important checks are done to see how the patient is doing. These include:
- Monitoring for engraftment and GVHD
- Assessing immune system reconstitution
- Managing possible infections and complications
Experts say the first 100 days after the transplant are key for success. This time has big milestones and challenges, needing careful care and focus on the patient.
We know the bone marrow transplant timeline can be complex and different for everyone. We aim to give personalized care, meeting each patient’s unique needs and experiences. 100 days after stem cell transplant, patients face crucial recovery milestones, improved immunity, reduced complications, and hopeful long-term outcomes
By understanding the bone marrow transplant timeline and its phases, we can better support patients. This helps ensure the best outcomes for them.
The 100 Days After Stem Cell Transplant Milestone
The 100-day mark after a stem cell transplant is a big milestone. At this point, we do detailed checks to see how the patient is doing. We look for any challenges they might face.
Clinical Assessments at This Checkpoint
At 100 days post-transplant, we focus on survival rates, infection risk, and immune recovery. We watch patients for signs of infection or graft-versus-host disease (GVHD). We then adjust their treatment plans as needed.
Some key assessments include:
- Monitoring of blood counts and immune function
- Evaluation of GVHD symptoms
- Assessment of organ function
Evolving Perspectives on Recovery Timelines
Recent studies have shown how complex recovery after a stem cell transplant can be. Dr. Rachel Salit’s study found that only 53% of patients were back to work at a median of 3 years post-transplant.
This highlights the need for ongoing support and care for patients during their recovery.
Adult Patient Survival Rates (75-80%)
Our data show that about 75-80% of adult patients survive to the 100-day mark after a stem cell transplant. While this is good, we know results can vary a lot.
Several factors can affect survival rates. These include:
- The source of stem cells
- The intensity of conditioning regimens
- Patient health before transplant
Factors Influencing Early Survival
Several factors can impact early survival rates after a stem cell transplant. These include the type of transplant, the patient’s overall health, and any comorbidities.
We work closely with patients to identify and reduce these risks. This helps improve their chances of a successful recovery.

By understanding what affects recovery, we can give better care and support to our patients. Our goal is to ensure each patient gets the best outcome after their stem cell transplant.
Immune System Reconstitution Progress
Rebuilding the immune system is key after a stem cell transplant. We watch how T-cells and B-cells grow back. These cells are vital for staying healthy.
T-Cell and B-Cell Regeneration
T-cells and B-cells are important for fighting off infections. T-cells help with cell-mediated immunity, and B-cells are key for humoral immunity. We keep a close eye on these cells to see how well the immune system is working.
A study in Frontiers in Pediatrics shows that T-cells and B-cells recover at different rates. The type of transplant, the patient’s age, and the treatment before transplant all play a role.
CD4+ T-Cell Recovery and Clinical Outcomes
CD4+ T-cell recovery is a big deal, mainly for those who got an autologous stem cell transplant. We’ve seen that quicker CD4+ T-cell recovery means better health and fewer infections.
- Important things that affect CD4+ T-cell recovery include:
- The patient’s age and health
- The type of stem cell transplant
- The treatment before transplant
By watching CD4+ T-cell recovery, we can help our patients’ immune systems get back on track. This supports their overall recovery.
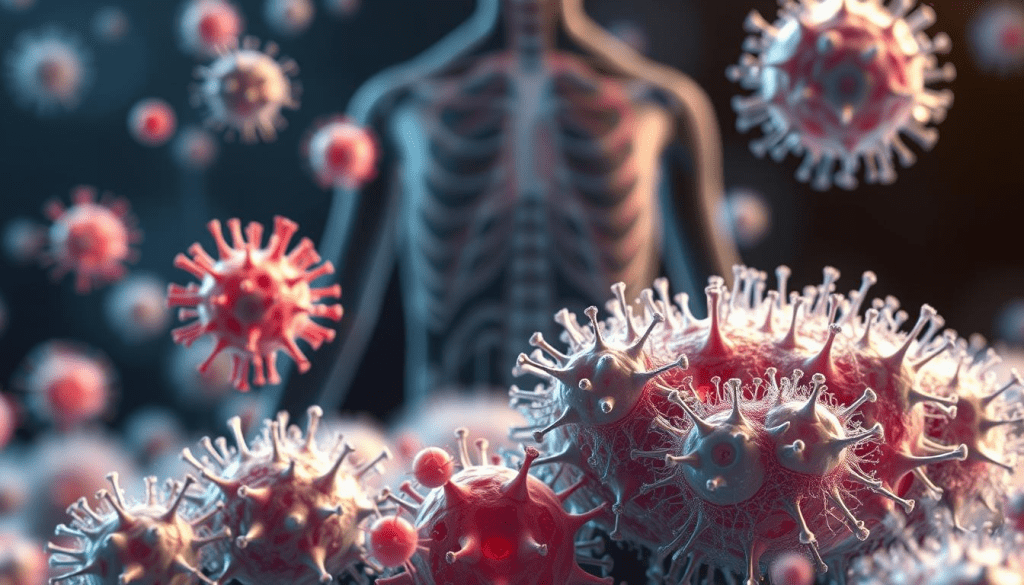
Infection Risks and Management Strategies
Infection risk is a big challenge in the first 100 days after a stem cell transplant. Patients are watched closely for signs of infection. We use preventive steps to lower this risk.
The Canadian Cancer Society says infection is a common side effect early on. The patient’s immune status, graft-versus-host disease, and preventive measures all play a role. We use proven strategies to manage these risks, giving our patients the best care.
Infection-Related Mortality Factors
Infection-related death is a big worry with stem cell transplants. Several things can affect this risk, like the patient’s health and the type of transplant. The CDC guidelines say managing these risks needs a detailed plan. This includes watching patients closely and acting fast when needed.
Preventive Protocols and Monitoring
We take many steps to prevent infections. These include:
- Using antimicrobial prophylaxis to stop infections
- Watching patients for early signs of infection
- Using isolation when needed to cut down on pathogen exposure
Our proactive and detailed approach to infection management helps improve patient outcomes in the 100 days after a stem cell transplant.
Graft-Versus-Host Disease Evaluation
After an allogeneic stem cell transplant, patients face the risk of graft-versus-host disease (GVHD). GVHD is a serious condition where the donor’s immune cells attack the recipient’s tissues. We provide detailed care for GVHD, using the newest treatments and monitoring methods.
Treatment Approaches and Response
Managing GVHD requires a variety of treatments, including medicines and supportive care. We customize our plans based on each patient’s needs and GVHD severity. We watch how treatments work and make changes to improve results.
- Immunosuppressive therapy to reduce the immune system’s attack on the recipient’s tissues
- Supportive care to manage symptoms and prevent complications
- Close monitoring of the patient’s condition to adjust treatment as needed
Transition to Chronic GVHD Monitoring
As patients move past the first 100 days after transplant, we focus on chronic GVHD. We check for signs of chronic GVHD regularly. Early detection is key to managing chronic GVHD effectively.
Key aspects of chronic GVHD monitoring include:
- Regular clinical assessments to detect signs of chronic GVHD
- Patient education on recognizing symptoms of chronic GVHD
- Multidisciplinary care to address the various organ systems that may be affected
Average Hospital Days by Transplant Type
The time spent in the hospital after a stem cell transplant varies. Patients getting umbilical cord blood transplants usually stay longer than those with peripheral blood stem cell transplants.
| Transplant Type | Average Hospital Days |
| Umbilical Cord Blood | 25-35 days |
| Peripheral Blood Stem Cell | 15-25 days |
Umbilical Cord Blood vs. Peripheral Blood Stem Cell Recovery
Recovery times differ for umbilical cord blood and peripheral blood stem cell transplants. Each transplant has its benefits and challenges. We watch each patient’s progress closely, no matter the transplant type, to offer personalized support.
Understanding each transplant type helps us better care for patients. We aim to help all patients recover well, regardless of their transplant type.
Patient-Centric Care Approaches
We focus on each patient’s unique needs after a stem cell transplant. This ensures a personalized recovery path. We know that everyone’s journey is different, needing special support and guidance.
Our care is centred on patient-centric care. We move away from strict timelines. Instead, we focus on what each patient goes through. Anthony Nolan highlights the importance of this approach for caring effectively and compassionately.
Individualized Recovery Assessment
We do individualized recovery assessments to offer the best care. These assessments help us see what each patient needs. Then, we create plans to support them.
The main parts of our assessment are:
- Looking at the patient’s medical history and current health
- Creating a care plan that meets their specific needs
- Keeping an eye on the plan and making changes as needed
This approach makes recovery better for those who have had stem cell transplants.
We’re dedicated to patient-centric care. Our support services help with the tough challenges patients face during recovery.
Autologous vs. Allogeneic Recovery Differences
It’s important to know the differences in recovery between autologous and allogeneic stem cell transplants. Each type uses different stem cells, which affects the recovery process. Autologous transplants use the patient’s own stem cells, while allogeneic transplants use donor stem cells.
Recovery Timelines
The autologous stem cell transplant timeline is usually shorter. Patients with autologous transplants often have an easier time recovering. They face fewer complications compared to those with allogeneic transplants.
Allogeneic recovery, on the other hand, is more complex. It comes with a higher risk of graft-versus-host disease. Dr. Rachel Salit’s study showed that allogeneic transplant patients stay longer at transplant centers.
Challenges in Allogeneic Recovery
Allogeneic recovery faces unique challenges that need careful management. We adjust our care to meet these specific needs. This helps reduce risks and supports the recovery process.
By understanding the bone marrow transplant timeline and recovery challenges, we can offer better support. This makes a big difference for our patients.
FAQ’s:
What is the significance of the 100-day mark after a stem cell transplant?
The 100-day mark is a key time in a patient’s recovery. Doctors check on survival rates, infection risk, and how well the immune system is recovering.
What are the different types of stem cell transplants, and how do they impact the recovery timeline?
There are two main types of stem cell transplants. Autologous uses the patient’s own stem cells, and allogeneic uses donor stem cells. Autologous transplants usually have a shorter recovery time. Allogeneic transplants can be harder because of the risk of graft-versus-host disease and other issues.
What is the intermediate recovery phase, and what are the key clinical milestones assessed during this period?
The intermediate recovery phase is from days 30 to 100 after the transplant. Patients are watched for signs of engraftment, graft-versus-host disease, and other complications.
What are the survival rates for adult patients 100 days after a stem cell transplant?
Studies show about 75-80% of adult patients survive to 100 days. But survival rates can change based on the stem cell source and how intense the treatment was.
How is immune system reconstitution monitored and supported after a stem cell transplant?
Doctors keep a close eye on how the immune system is coming back. They focus on T-cell and B-cell regeneration, like CD4+ T-cell recovery. They also help patients recover quickly to lower the risk of infections and other problems.
What are the infection risks after a stem cell transplant, and how are they managed?
Infection risk is high in the first 100 days after transplant. Patients are watched for signs, and steps are taken to prevent infections. This includes using proven strategies to reduce infection-related deaths.
What is graft-versus-host disease, and how is it evaluated and managed?
Graft-versus-host disease (GVHD) is a complication of allogeneic stem cell transplant. It happens when the donor’s immune cells attack the recipient’s tissues. GVHD is managed through various treatments and by watching for chronic GVHD signs.
How does the type of transplant impact the recovery timeline and hospital stay?
The type of transplant, like umbilical cord blood or peripheral blood stem cell transplant, affects recovery time and hospital days. Knowing these differences helps us tailor care and support to each patient.
What is patient-centric care, and how is it delivered after a stem cell transplant?
Patient-centric care focuses on each patient’s unique recovery journey. We provide personalized recovery assessments and support to help patients overcome the challenges they face.
What are the key differences between autologous and allogeneic recovery journeys?
Autologous transplants usually have a shorter recovery time. Allogeneic transplants are more challenging due to graft-versus-host disease and other complications. Understanding these differences helps us tailor care and support for each patient’s recovery journey.
References
- National Cancer Institute. (2023). Stem Cell Transplants in Cancer Treatment: Questions and Answers. Retrieved from https://www.cancer.gov/about-cancer/treatment/types/stem-cell-transplant
- U.S. National Library of Medicine. (2020). Immune Reconstitution After Allogeneic Hematopoietic Stem Cell Transplantation. Frontiers in Immunology, 11, Article 1500. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386861/
- U.S. National Library of Medicine. (2022). Graft-versus-Host Disease: Pathophysiology and Clinical Management. Cancers, 14(18), Article 4402. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9599554/