Last Updated on December 2, 2025 by Bilal Hasdemir
Are milk ducts mastectomy remove? Get the shocking, definitive answer and learn what it means for your body post-surgery. Many women have a mastectomy to save their lives. But it makes them wonder about their breast tissue and how it works. They often ask, “What happens to milk ducts after surgery?” It’s a scary time, and knowing the facts is key to making good health choices.
Women who have had a mastectomy might find it hard to breastfeed or make breast milk. How much this affects them depends on the surgery type and their health. We’ll look at the different mastectomy types and how they impact breast tissue.
Key Takeaways
- The type of mastectomy performed affects the removal of milk ducts.
- Breastfeeding ability may be impacted after a mastectomy.
- Understanding the anatomy of the breast is key to understanding mastectomy effects.
- We offer full support and care for mastectomy patients.
- Results can vary based on the surgery and overall health.
Understanding Mastectomy Procedures

A mastectomy is a big surgery choice. It involves different procedures based on the patient’s needs. Understanding these procedures enables patients to make informed decisions about their care.
Types of Mastectomy
There are a few types of mastectomy, like partial and total mastectomy. The choice depends on the cancer’s size and the patient’s health.
Partial Mastectomy: This removes the cancer and some healthy tissue. It’s often for early-stage breast cancer.
Total Mastectomy: This removes the whole breast, including the nipple-areola complex. It’s more extensive and recommended for bigger tumors or high risk of recurrence.
Indications for Mastectomy
Mastectomy is needed for many reasons, like treating breast cancer or reducing risk. It’s also used for some diagnostic tests.
- Breast cancer diagnosis
- High risk of breast cancer due to genetic mutations (e.g., BRCA1 and BRCA2)
- Recurrence after previous lumpectomy or radiation therapy
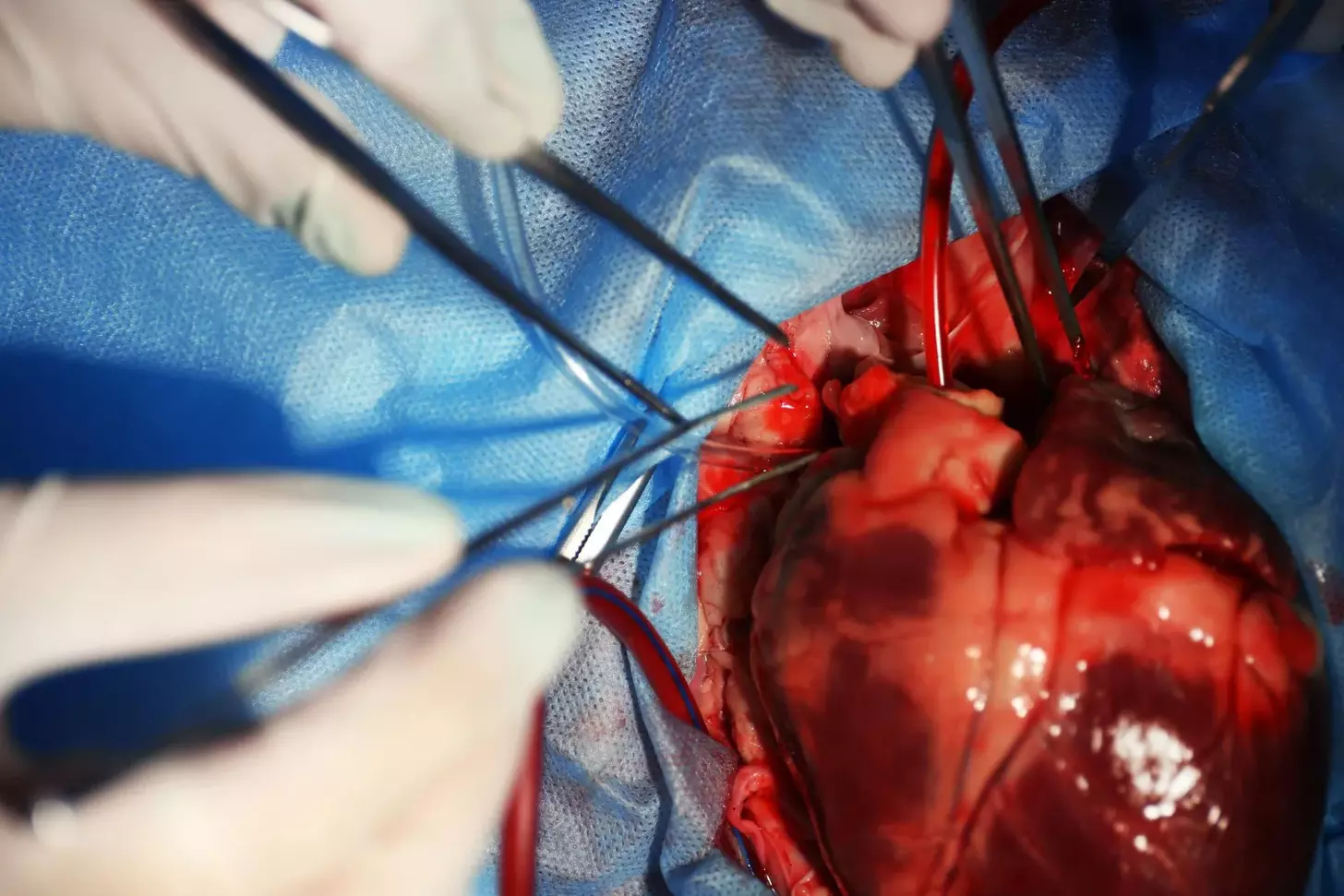
The Surgical Process
The surgery process includes several steps, from preparation to recovery. Knowing this can help reduce anxiety and prepare patients.
The surgery starts with anesthesia to keep the patient comfortable. Then, the surgeon removes the breast tissue, trying to save as much skin and muscle as possible.
After surgery, patients are watched in a recovery area, and pain is managed. Follow-up care includes checking for complications and supporting the patient’s recovery.
What Are Milk Ducts?
Milk ducts in the breast are key for making and moving milk. They are also known as lactiferous ducts. These ducts are vital for breastfeeding. Knowing how they work helps us understand their role in nursing and how surgery might affect it.
Function of Milk Ducts
Milk ducts carry milk from the lobules to the nipple. This network is designed for efficient milk delivery during breastfeeding. The ducts have epithelial cells and muscle cells to help push out milk.
Anatomy of the Breast
The breast has glandular, fatty, and connective tissue. Milk is made in the glandular tissue, where ducts are important. The ducts spread out like a tree, ending at the nipple. Knowing this helps us see how ducts work and how surgery might impact them.
Milk Ducts and Lactation
Lactation is how the body makes and releases milk for babies. Milk ducts are essential for this, carrying milk from the lobules to the nipple. Hormones make the muscle cells around the ducts contract, releasing milk. Damage to ducts from surgery can affect a mother’s ability to nurse.
Many worry about how mastectomy might affect milk ducts and lactation. Our team is here to offer detailed info and support. We aim to help you understand these changes and make choices about your health.
Impact of Mastectomy on Milk Ducts
Mastectomy procedures can affect milk ducts differently. The type of surgery done is key to how much is removed or damaged. We’ll look at how complete and partial mastectomies impact breast tissue.
Complete Mastectomy Explained
A complete mastectomy removes all breast tissue, including milk ducts. It’s often chosen for those with breast cancer or high risk. This surgery means no future lactation in the affected breast.
Duct preservation isn’t a goal in complete mastectomy. Patients should know it affects future pregnancies and breastfeeding.
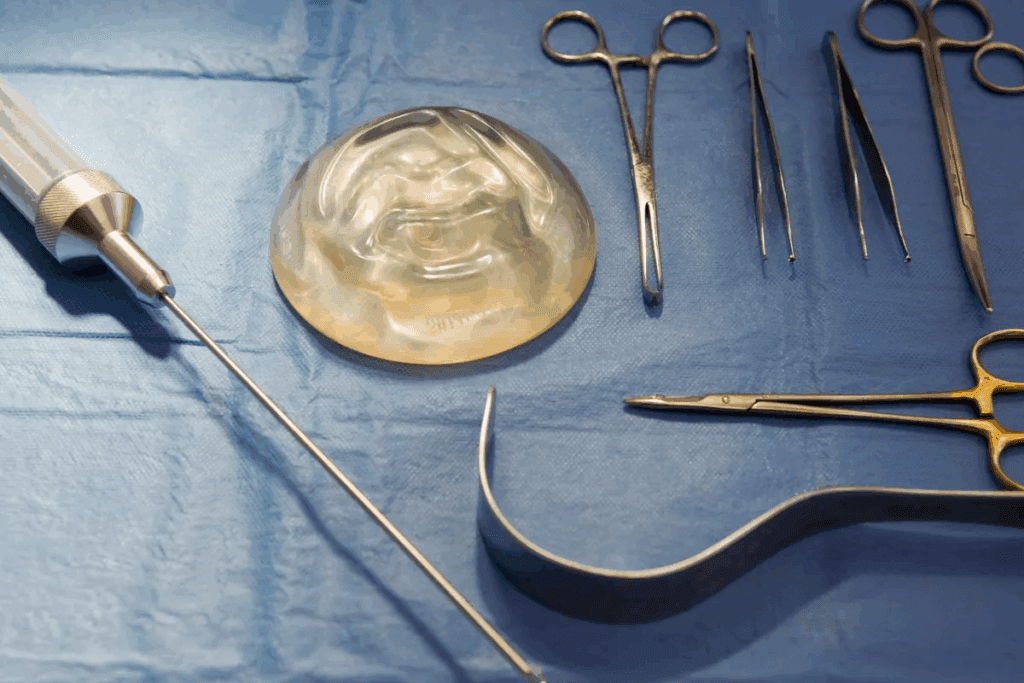
Partial Mastectomy and Duct Preservation
Partial mastectomy, or lumpectomy, aims to keep more of the breast. Duct preservation techniques might be used to help with breastfeeding. This depends on the cancer’s location and how much tissue is removed.
- The surgical method greatly affects duct preservation.
- Some patients can lactate after partial mastectomy, depending on duct preservation.
- Doctors decide on duct preservation based on the patient’s health and condition.
Changes in Breast Tissue
The tissue removal effect from mastectomy changes breast tissue a lot. These changes vary with complete or partial mastectomy. Patients should expect changes in how their breast looks and feels.
It’s important to understand these changes to manage expectations and deal with the surgery’s effects. Our team supports patients through every step, providing care and guidance.
Post-Surgery Breast Changes
Women often face many physical changes after a mastectomy. These changes can differ a lot from person to person. They depend on the type of mastectomy and the individual’s health.
Scarring and Tissue Regeneration
Scarring is a normal part of healing after a mastectomy. The amount of scarring can change based on the surgery method and how well the body heals. We aim to reduce scarring and help with the healing process.
After a mastectomy, the body starts to heal and rebuild tissue. This can sometimes cause scar tissue to form. Knowing about this process can help manage expectations and support recovery.
Changes in Sensation
Changes in feeling are common after a mastectomy. These can range from numbness to feeling more sensitive. We help patients manage these changes and support them during recovery.
The extent of these changes can vary a lot. Some people might have temporary changes, while others might have lasting ones. Our healthcare team is here to address these changes and provide personalized care.
The Role of Hormones
Hormones are key to breast health, and mastectomy can affect hormone levels. Understanding how hormones and breast tissue interact can help us grasp the changes after surgery.
We know how important hormones are for the body. We offer care that considers these factors. Our team is dedicated to supporting patients through the physical and emotional aspects of recovery, ensuring they get the care they need.
Nursing Considerations After Mastectomy
Women who have had a mastectomy face a complex journey to breastfeeding. We know how important breastfeeding is to motherhood. We’re here to offer the support and resources you need.
Future Pregnancies and Breastfeeding
Women after a mastectomy worry about future pregnancies and breastfeeding. Talking to healthcare providers is key to understanding your options. Some can breastfeed with one breast or use donor milk.
Women planning future pregnancies should talk to lactation consultants and healthcare providers. They can help create a breastfeeding plan tailored to you.
Lactation After Mastectomy
Lactation after mastectomy can be tough due to changes in the breast. But, with the right support, some women can produce milk. Donor milk alternatives are also an option for those who can’t produce enough.
- Lactation consultants can help with expressing milk and managing lactation.
- Donor milk banks provide safe, screened milk for mothers in need.
- Healthcare providers can advise on hormonal treatments to support lactation.
Support Resources for New Mothers
New mothers after a mastectomy need all-around support. We offer emotional, physical, and medical care. Our resources include:
- Access to lactation consultants for personalized breastfeeding support.
- Info on donor milk alternatives and how to get them.
- Emotional support through counseling and support groups.
We aim to support new mothers in their breastfeeding journey. We want to ensure they get the care and guidance they need.
Psychological Effects of Mastectomy
Mastectomy is a key treatment for breast cancer but it has deep emotional effects. It removes not just breast tissue but also brings emotional challenges. These can be hard to deal with.
Coping with Body Image Changes
Body image changes are a big psychological impact of mastectomy. Women often find it hard to accept losing a breast. This can hurt their self-esteem and confidence. Coping with these changes needs emotional support and professional help.
We know how important it is to address body image concerns. Our team offers full care, including emotional support for mastectomy challenges.
Support Networks and Therapy
A strong support network is key for women having mastectomy. This network can include family, friends, and support groups. Here, people can share their stories and get support.
Therapy is also very helpful. It lets women deal with their feelings and find ways to cope. Cognitive-behavioral therapy (CBT) and other talk therapies help manage mastectomy’s emotional effects.
Support Options | Description | Benefits |
Support Groups | Groups where individuals share their experiences | Provides a sense of community and understanding |
Cognitive-Behavioral Therapy (CBT) | A form of talk therapy focusing on coping strategies | Helps manage negative thought patterns and behaviors |
Family and Friends | Personal network providing emotional support | Offers emotional comfort and practical help |
Importance of Counseling
Counseling is vital for recovery, giving a safe place to talk feelings. Counselors help manage anxiety, depression, and other emotional issues after mastectomy.
We stress the need for counseling services in care plans. Our team ensures patients get the emotional support they need during recovery.
Monitoring Health Post-Mastectomy
After a mastectomy, it’s important to watch your health closely. This means regular check-ups and knowing the signs of complications. Being proactive helps catch problems early.
Regular Check-ups and Imaging Tests
Check-ups and imaging tests are key to keeping an eye on your health. Make sure to see your doctor regularly. These visits can include:
- Mammograms or other imaging tests on the remaining breast tissue
- Physical examinations to check for any signs of complications or recurrence
- Discussion of any concerns or symptoms you are experiencing
Imaging tests are vital for catching problems early. We use the latest technology to get accurate results.
Type of Test | Frequency | Purpose |
Mammogram | Annually | To detect abnormalities in breast tissue |
Ultrasound | As recommended | To further investigate detected abnormalities |
MRI | As recommended | To provide detailed images of breast tissue |
Signs of Complications to Watch For
Knowing the signs of complications is important. Look out for symptoms like:
- Unusual swelling or pain in the chest or arm
- Changes in the skin, such as redness or dimpling
- New lumps or thickening in the breast or underarm area
If you notice any of these, contact your doctor right away.
Importance of Breast Health Awareness
Being aware of breast health is important for everyone, but even more so after a mastectomy. Stay informed and proactive about your health. Know your risk factors and watch for signs of problems.
By staying informed and vigilant, you can play an active role in your health. We’re here to support you every step of the way.
Alternatives to Mastectomy
There are many options other than mastectomy for breast cancer treatment. These choices aim to remove the cancer while keeping as much of the breast as possible.
Options for Breast Conservation
Breast conservation therapy, or lumpectomy, removes the tumor and some tissue around it. Then, radiation therapy kills any cancer cells left. We help decide if this is right for you based on the tumor’s size and your health.
This method tries to keep the breast looking and feeling natural. It’s a good choice for those who want to keep more of their breast tissue.
Pros and Cons of Different Approaches
It’s important to think about the good and bad of each option. Breast conservation has many benefits:
- It keeps the breast looking and feeling normal
- It’s less invasive than mastectomy
- Recovery might be shorter
But, there are also downsides:
- There’s a chance you might need more surgeries
- You’ll need radiation therapy, which adds time and cost
- Radiation can change how the breast looks
Treatment Option | Pros | Cons |
Breast Conservation Therapy | Preserves breast tissue, less invasive | May require additional surgeries, radiation therapy |
Mastectomy | Can be more effective for larger tumors, reduces risk of recurrence | More invasive, significant scarring possible |
Discussing Options with Your Doctor
Talking openly with your doctor about treatment options is key. We encourage asking about the benefits and risks of each choice. Also, what to expect during recovery.
Together, we can create a treatment plan that fits your needs and preferences. This way, you get the best care for your situation.
Conclusion: Moving Forward After Mastectomy
Recovering from mastectomy is a journey of both physical and emotional healing. Understanding how mastectomy affects milk ducts and breast changes is key. It’s also important to know the emotional impact.
Embracing change and maintaining a focus on recovery is essential. Ongoing support is essential, not just at first but throughout your journey. Our team is here to provide exceptional care and support.
Path to Recovery
A holistic recovery plan includes access to resources for your physical and emotional health. This means regular check-ups, imaging tests, and counseling. These services help with the emotional side of recovery.
Ongoing Support and Wellness
We’re committed to ongoing support to make your recovery smooth. By focusing on health and wellness, we help you face mastectomy recovery with confidence. We empower you to embrace change.
We aim to provide complete care and support. This way, you can have a fulfilling recovery, focusing on your health and wellness.
FAQ
What happens to milk ducts after a mastectomy?
The effect of mastectomy on milk ducts varies. In a total mastectomy, most ducts are removed. But, a partial mastectomy might save some ducts, allowing for breastfeeding.
Can I stil breastfeed after a mastectomy?
Breastfeeding after a mastectomy is tough but possible. It depends on the surgery’s extent and if ducts were saved. We can explore options like donor milk to help.
How does a mastectomy affect breast tissue and sensation?
A mastectomy changes breast tissue and sensation. Scarring and tissue changes happen. Hormones also play a role in breast health. We’re here to support you through these changes.
Are there different types of mastectomy procedures?
Yes, there are different mastectomy types, like total and partial. The choice depends on your situation. Our team will explain your procedure’s details.
What are the implications for future pregnancies after a mastectomy?
Future pregnancies might affect breastfeeding after a mastectomy. But, we offer guidance and support for new mothers.
How can I cope with body image changes after a mastectomy?
Dealing with body changes after a mastectomy is tough. We stress the importance of support, therapy, and counseling. These can help you cope.
What are the signs of complications to watch for after a mastectomy?
It’s key to watch for health issues after a mastectomy. We’ll guide you on check-ups, tests, and staying aware of breast health.
Are there alternative treatments to mastectomy?
Yes, there are other treatments like breast conservation. We can discuss the benefits and drawbacks of each option to help you decide.
How can I maintain my health and well-being after a mastectomy?
Keeping healthy after a mastectomy needs ongoing care and support. We’re dedicated to providing top-notch care and resources to support your recovery.
Can I stil have nipple-sparing duct sparing surgery?
Nipple-sparing duct sparing surgery is possible in some cases. It might help with breastfeeding. But, it depends on your situation. We’ll discuss your options with you.
How do hormones influence breast health after a mastectomy?
Hormones are important for breast health, and changes can happen after a mastectomy. We can guide you on how hormones affect your breast health and overall well-being.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31053520/